I vividly remember the moment I sat in the sterile doctor’s office, clutching my shoulder in frustration. The nagging pain had become relentless, and despite countless visits, I felt stuck, like my body was sending mixed signals I couldn’t decode. When my doctor finally mentioned an EMG nerve test, I felt a wave of uncertainty and concern. Was this test necessary? Would it really reveal what’s going on? That lightbulb moment made me realize how confusing medical jargon and tests can be—yet, understanding their purpose can truly make a difference in your recovery journey.
Why Your Doctor Might Be Sending You for an EMG in 2026
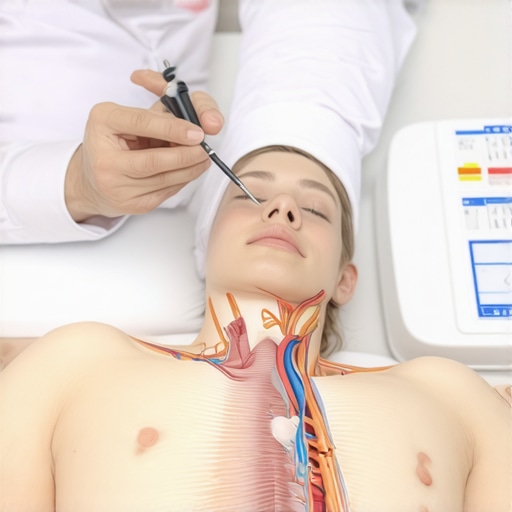
Over the years, I’ve learned that certain diagnostic tests, like the Electromyography or EMG, are crucial tools in pinpointing nerve and muscle issues. In 2026, doctors rely more than ever on EMG tests because they provide detailed insights that other imaging methods might miss. For instance, you might be surprised to learn that even if your MRI is clear, an EMG can detect nerve problems that aren’t visible on scans. This is especially true for conditions like herniated discs or nerve compressions that cause persistent pain and weakness. Understanding these reasons helped me accept the test as a necessary step rather than a daunting procedure.
Is an EMG Actually Worth It or Just Overkill?
I’ll admit, early in my experience, I thought, “Do I really need this nerve test? Can’t they just diagnose me with a physical exam?” That mistake almost led me to skip essential diagnostics. The truth is, EMGs are highly effective at providing concrete data about nerve function, which can prevent misdiagnosis and ensure targeted treatments. Studies show that EMG testing improves diagnostic accuracy for nerve-related issues, reducing unnecessary surgeries or treatments (source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6785382/). If you’re feeling overwhelmed or skeptical, remember that skipping important tests might delay your recovery—something I initially overlooked. It’s better to trust your healthcare team and ask questions about what’s best for your specific condition. Curious if this test is relevant for your situation? Feel free to explore [top-rated orthopedic specialists](https://njorthopedicdoctor.xyz/top-rated-orthopedic-spine-specialists-to-trust-in-2025) who can provide guidance tailored to your needs. Now, let’s see how you can proactively prepare and understand your EMG process to get the most out of it.
Preparing for Your Diagnosis and Follow-Up Appointments
Start by organizing your medical history, including any prior injuries or surgeries. Bring a detailed list of symptoms and questions to your appointment at an orthopedic clinic for slip and fall NJ or your trusted specialist. This ensures your doctor comprehensively understands your condition, facilitating accurate diagnosis. During the visit, request a clear explanation of diagnostic codes like those listed on orthopedic diagnosis codes to understand the basis of your assessment. After your initial consultation, schedule regular follow-ups as recommended—typically every 4-6 weeks—to monitor progress.
Setting Up Your Treatment Plan and Understanding Your Options
Once diagnosed, work with your orthopedic surgeon or specialist to develop a tailored treatment plan. For non-surgical back pain, consider options highlighted on non-surgical treatments like physical therapy, spinal decompression, or injections. For example, I had a herniated disc, and after trying minimally invasive approaches detailed on this page, my pain significantly decreased. It’s vital to understand which procedures — from steroid injections to nerve blocks — could be applicable, ensuring informed decisions. Always clarify with your doctor whether surgery is necessary by discussing signs that indicate escalation, as outlined on these signs.
Implementing Effective Rehabilitation Strategies
Effective recovery hinges on proper rehabilitation. Follow personalized physical therapy guided by your surgeon, emphasizing exercises from trusted sources like orthopedic rehab tips. For a quicker return to work, see the procedures at this link for clearance guidelines. Incorporate stretches, strength-building activities, and ergonomics adjustments to prevent re-injury. I remember enduring a long period of rehab after lumbar fusion; sticking to a disciplined routine and understanding each exercise’s purpose made a noticeable difference. Regular follow-up appointments are essential to track healing progress and modify your plan as needed.
Using Supportive Devices and Modifications
Leverage supportive braces or orthotics available from local providers to stabilize your injured area. Simple ergonomic modifications, like adjusting your workspace or sleeping arrangements, can alleviate strain. For instance, I upgraded my mattress based on recommendations from this resource, leading to better sleep and faster healing. Combining support with smart modifications reduces stress on your healing tissues and enhances your comfort during recovery.
Staying Informed and Proactive
Stay engaged with reputable information—such as the guides on auto accident injury or workers’ compensation—to recognize early signs of complications. When symptoms worsen or new issues arise, consult your healthcare team promptly via direct contact. Document your recovery progress with photos or journals, which can be useful during follow-up visits or insurance claims. This proactive approach, combined with regular assessments, empowers you to navigate your recovery confidently and effectively.While many believe they fully understand orthopedic procedures like trigger point injections or the importance of follow-up schedules, a deeper dive reveals common misconceptions that can hinder recovery. For example, the myth that non-surgical back pain treatments are always less effective than surgery can be misleading; studies show that advanced minimally invasive approaches often yield better outcomes with fewer risks (learn more here).�The trap lies in oversimplifying diagnostic coding or follow-up intervals, which can lead to inadequate care and delayed healing. Did you know that not all follow-up schedules are created equal? Failing to schedule timely visits may compromise long-term recovery, especially in complex cases like spondylolisthesis or rotator cuff tears. �Have you ever fallen into this trap? Let me know in the comments.
Are Some Orthopedic Diagnosis Codes Overrated or Underestimated?
Many patients and even some practitioners overlook the significance of accurate coding. Relying on a generic list instead of precise, condition-specific codes can delay insurance approvals or alter treatment plans. According to expert guidance, precise codes are essential for ensuring appropriate coverage and avoiding claim denials (see the list here). This nuance becomes critical in cases like workers’ comp claims, where documentation differences might affect injury recognition. Recognizing these subtleties can make a substantial difference in timely, effective care.
Another overlooked aspect is the misconception that proceeding without a comprehensive follow-up plan minimizes costs. In reality, neglecting proper post-treatment assessments, especially after procedures like trigger point injections or minimally invasive surgeries, can lead to recurrent issues and even more expenses over time. Engaging top-rated orthopedic surgeons, such as those listed in this trusted directory, helps craft a tailored follow-up schedule that suits your injury’s complexity.
In sum, understanding the advanced nuances—like the significance of precise diagnosis codes or strategic follow-up planning—can elevate your orthopedic care from good to exceptional. It ensures you receive the most effective, personalized treatment engine, ultimately speeding up recovery and reducing the risk of complications. If you want to explore this further, a consultation with a specialized orthopedic doctor can help clarify your unique needs. Remember, the devil is in the details when it comes to healthcare decisions.Maintaining optimal orthopedic health over time requires more than just periodic visits to your doctor; it involves leveraging specific equipment, software, and methods designed to support recovery, track progress, and prevent setbacks. One essential piece of equipment I personally rely on is a high-quality ergonomic mattress, which significantly reduces strain on the spine during sleep—a critical factor in long-term back health. I recommend models with adjustable firmness and pressure relief, as they help maintain proper spinal alignment and alleviate chronic discomfort. Regular use of targeted physical therapy devices, such as portable muscle stimulation units, can accelerate healing by promoting blood flow and reducing muscle atrophy. I’ve found that integrating these into my daily routine makes a noticeable difference in sustaining progress after procedures like lumbar fusion.
How do I maintain orthopedic improvements over time?
In addition to physical tools, utilizing comprehensive tracking software like MyRehabApp allows me to monitor my mobility, pain levels, and exercise adherence. This app provides personalized reminders and logs that are invaluable for staying consistent with rehabilitation routines prescribed by your orthopedic specialist. Moreover, digital platforms that connect you directly with your care team ensure that adjustments can be made promptly, preventing minor issues from escalating. As technology advances, I predict a move toward AI-driven apps capable of analyzing your movement patterns via smartphone sensors to recommend real-time modifications, optimizing recovery and maintenance efforts.![]() this directory. Don’t forget, integrating advanced support methods like wireless EMG monitoring and AI-powered apps will shape the future of orthopedic maintenance, so staying informed and engaged is your best bet for lasting results.
this directory. Don’t forget, integrating advanced support methods like wireless EMG monitoring and AI-powered apps will shape the future of orthopedic maintenance, so staying informed and engaged is your best bet for lasting results.
Why the Small Details Make a Big Difference in Orthopedic Success
One of the most eye-opening lessons I learned was that meticulous attention to diagnosis codes can significantly impact treatment timelines and insurance approval. Relying on precise coding instead of generic categories has often meant the difference between swift recovery and unnecessary delays. Additionally, understanding the importance of personalized follow-up schedules helped me avoid setbacks and stay ahead of complications. These insights taught me that proactive communication with top-rated orthopedic surgeons and clinics, like those listed in this directory, can empower you to receive tailored care that accelerates healing.
Furthermore, I realized that many patients overlook the value of non-surgical back pain treatments, which can sometimes be more effective than invasive procedures. Combining physical therapy with minimally invasive options, as explained on this page, often leads to faster recovery and fewer risks. The biggest lesson? Staying informed about your condition and engaging actively with your recovery plan creates the best chance for a successful outcome.
My Arsenal of Resources for Better Orthopedic Outcomes
Over the years, I’ve come to trust several tools and sources that truly make a difference. The first is Effective Non-Surgical Care for Herniated Discs, which provides practical insights into alternatives to surgery. For ongoing rehab, Orthopedic Rehab Tips helped me craft routines that support healing. Digital tracking apps like MyRehabApp serve as daily motivators and monitors, ensuring I stay consistent with exercises and pain management strategies.
Lastly, I highly recommend consulting with top orthopedic specialists to develop a personalized recovery plan. Combining these resources has been instrumental in my journey beyond just healing—it’s about building resilience and understanding your body better.
Embrace the Road Ahead with Confidence
This journey into orthopedic health is a personal one, and your proactive involvement can transform challenges into opportunities for growth. Whether you’re navigating a slip and fall injury or managing chronic pain, remember that expert care exists and is accessible. The future of orthopedic recovery hinges on informed decisions, early intervention, and supportive technologies like AI-driven monitoring. Take the first step today by reaching out to a trusted specialist listed in this guide—your body will thank you for it. You’re capable of turning setbacks into comebacks, and every step forward is a victory worth celebrating.