Unveiling the Hidden Risks: Why Orthopedic Evaluation After Auto Accidents Matters
Auto accidents can inflict a spectrum of injuries, some immediately apparent and others stealthily developing over time. Orthopedic injuries, in particular, often present complexities that require expert diagnosis to prevent long-term disability. Understanding what injuries to watch for after a collision is essential not only for immediate treatment but also for safeguarding your future mobility and quality of life. This article delves into the critical orthopedic concerns following auto accidents, highlighting subtle signs, expert insights, and the importance of timely intervention.
The Silent Threats: Common Orthopedic Injuries Post-Auto Accident
While fractures and obvious bruises are easily noticed, many orthopedic injuries evade immediate detection. Whiplash, a prevalent soft tissue injury affecting the cervical spine, can manifest as persistent neck pain or stiffness days after the incident. Ligament sprains and muscle strains in the back and limbs often mimic general soreness but may indicate deeper tissue damage requiring specialized care.
More severe injuries such as herniated discs or joint dislocations can cause radiating pain, numbness, or weakness, signaling nerve involvement. For example, a herniated lumbar disc pressured by trauma might lead to sciatica symptoms, severely impacting daily activities.
How Can You Recognize Orthopedic Injuries That Might Not Appear Immediately?
Recognizing subtle orthopedic damage requires vigilance. Persistent pain beyond the typical healing period, swelling, decreased range of motion, or neurological symptoms like tingling or numbness should prompt an immediate evaluation by an orthopedic specialist. Early diagnostic imaging, such as MRI or X-rays, often reveals injuries invisible to the naked eye. Taking prompt action can prevent chronic conditions and improve recovery outcomes significantly.
Expert Orthopedic Strategies: Navigating Diagnosis and Treatment
Orthopedic care after auto accidents extends beyond initial emergency treatment. Specialists employ advanced diagnostic tools—such as comprehensive orthopedic diagnostic imaging services—to accurately identify the injury pattern. Treatment plans are then personalized, often combining non-surgical therapies including physical rehabilitation and pain management injections, with surgical options reserved for severe cases.
For instance, if a patient suffers a slipped or bulging disc post-accident, effective non-surgical care for herniated discs can alleviate symptoms and restore function without invasive procedures. Rehabilitation guidance focusing on strengthening and mobility also plays a crucial role in long-term recovery.
The Legal and Medical Intersection: Why Accurate Orthopedic Documentation Is Crucial
Beyond health, orthopedic injury documentation holds significant value in personal injury claims. Detailed medical records and diagnostic reports support the legal process by substantiating injury severity and treatment necessity. This synergy between orthopedic care and legal advocacy underscores the importance of seeing specialists experienced in personal injury cases.
For patients in New Jersey, exploring resources like how orthopedic medical records help attorneys win cases can provide clarity on navigating the intersection of medical care and legal rights.
Engage with specialized orthopedic professionals to ensure comprehensive care and proper documentation, enhancing both your health outcomes and legal position.
If you’ve experienced an auto accident and suspect orthopedic injuries, learn what to expect from an orthopedic doctor after an auto accident to guide your next steps.
Interested in more expert orthopedic insights or personal injury recovery tips? Feel free to share your experiences or questions in the comments below and help build a knowledgeable community.
For authoritative information on whiplash and related injuries, the Centers for Disease Control and Prevention (CDC) offers comprehensive resources.
My Journey Through Orthopedic Recovery: Lessons Learned After the Accident
Reflecting on my own experience after a minor auto accident, I quickly realized that the journey toward recovery was as much about patience and informed decisions as it was about medical treatment. Initially, I thought the soreness in my back and neck would resolve on its own, but the discomfort lingered longer than expected. This prompted me to seek a comprehensive orthopedic evaluation—a step that proved crucial.
The orthopedic specialist I visited emphasized the importance of early diagnostic imaging, like MRI scans, to detect any hidden issues such as disc herniations or ligament strains. This personalized approach was a game-changer; it allowed targeted therapy that sped up my healing and prevented complications. For anyone navigating similar circumstances, I can’t stress enough how vital it is to advocate for thorough orthopedic assessments.
What Are the Most Effective Non-Surgical Treatments for Post-Accident Orthopedic Injuries?
This question came up often during my recovery conversations with medical professionals and fellow patients. Based on my experience and supported by expert recommendations, non-surgical interventions can be profoundly effective if tailored correctly. Physical therapy focusing on strengthening and flexibility was at the core of my rehabilitation, complemented by pain management techniques including orthopedic injections that helped manage inflammation without heavy reliance on opioids.
Additionally, the use of orthopedic support bracing provided much-needed stability during the early recovery phase, preventing further injury while encouraging healing. According to the effective non-surgical care for herniated discs guide, combining these methods optimizes outcomes and reduces the need for invasive procedures.
One practical tip I found invaluable was to maintain open communication with my orthopedic team, ensuring adjustments to therapy plans based on progress and setbacks. This dynamic approach made me feel empowered rather than overwhelmed by my condition.
Understanding Insurance and Authorization: A Personal Reflection
Another layer of complexity after an auto accident is navigating insurance approvals and prior authorizations. I vividly recall the frustration of waiting for insurance clearance before certain treatments, which could potentially delay recovery. Learning about resources such as orthopedic prior authorization help was a turning point. These services can assist patients in expediting approvals, ensuring timely access to necessary care.
From my perspective, being proactive in understanding insurance requirements and maintaining meticulous records of medical interactions can avoid unnecessary delays. It’s not just about health but also about advocating for yourself through the administrative maze.
When Should You Seek a Second Opinion or a Specialist?
There were moments during my recovery when progress plateaued, and I wondered whether a different orthopedic specialist might offer new insights. Seeking a second opinion can be a valuable step, especially if symptoms persist or worsen despite treatment.
In New Jersey, for example, patients have access to top orthopedic spine specialists and comprehensive diagnostic services, such as those listed in top orthopedic spine specialists to trust in 2025. Consulting with a specialist can clarify complex issues like bulging discs or pinched nerves, enabling more precise interventions.
From personal experience, don’t hesitate to explore options if your current plan isn’t delivering the expected relief. Your health and mobility are worth the extra effort.
Have you or a loved one experienced orthopedic challenges after an auto accident? I’d love to hear your story or any tips you’ve found helpful in the comments below. Sharing our journeys can provide support and guidance to others facing similar challenges.
Decoding Complex Orthopedic Trauma: Beyond the Obvious Injuries
Post-auto accident orthopedic trauma can be deceptively intricate, involving multi-structural damage that challenges both diagnosis and treatment. Beyond fractures and soft tissue injuries, clinicians must remain vigilant for occult pathologies such as subtle vertebral endplate fractures, micro-tears in ligaments, and early osteochondral lesions that may not manifest on initial imaging. These injuries, if overlooked, can precipitate chronic pain syndromes and functional impairment.
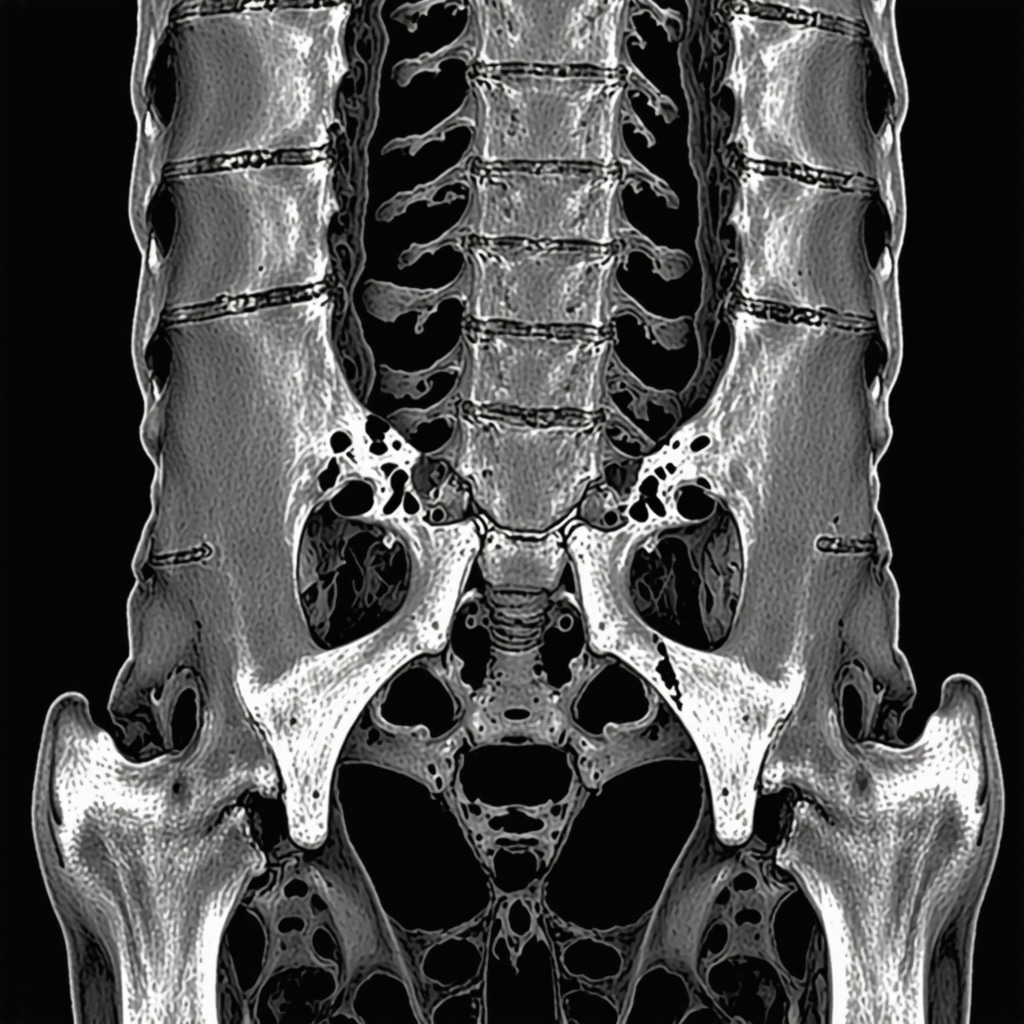
For example, damage to the thoracolumbar junction often escapes detection during routine evaluations but can contribute to persistent axial back pain and biomechanical instability. Advanced imaging modalities, including high-resolution MRI and CT scans with 3D reconstruction, are indispensable tools in unveiling these hidden complexities.
What Are the Latest Innovations in Orthopedic Diagnostic Imaging Post-Trauma?
Recent advancements in orthopedic imaging have revolutionized post-accident evaluations. Techniques such as diffusion tensor imaging (DTI) provide nuanced insights into nerve tract integrity, enhancing detection of nerve injuries secondary to disc herniations or vertebral fractures. Additionally, dynamic MRI assessments allow visualization of joint kinematics under physiological load, revealing instability not evident in static scans.
Moreover, ultrasonography has gained prominence as a real-time, radiation-free modality for assessing soft tissue injuries including ligamentous tears and muscle contusions. This modality permits guided interventions such as corticosteroid injections with precision, optimizing therapeutic outcomes.
Integrating these modalities into diagnostic protocols enables a more comprehensive understanding of injury patterns, facilitating personalized treatment strategies.
Harnessing Cutting-Edge Therapeutics: From Biologics to Minimally Invasive Surgery
Orthopedic treatment paradigms post-auto accident have evolved significantly, embracing biologic therapies and minimally invasive surgical techniques that prioritize tissue preservation and rapid recovery. Platelet-rich plasma (PRP) injections and stem cell therapies are increasingly utilized to stimulate regenerative processes in damaged ligaments and cartilage.
Minimally invasive spine surgeries, such as endoscopic discectomy and percutaneous vertebroplasty, reduce operative morbidity and hospital stay durations. These approaches are particularly valuable for patients with herniated discs or vertebral compression fractures, enabling symptom relief with expedited return to function.
Advanced rehabilitation programs now incorporate neuromuscular re-education and proprioceptive training, addressing not only structural healing but also functional restoration of movement patterns disrupted by trauma.
Integrating Multidisciplinary Care: The Future of Orthopedic Recovery Post-Accident
Optimal recovery from orthopedic injuries sustained in auto accidents increasingly depends on multidisciplinary collaboration. Physical therapists, pain specialists, orthopedic surgeons, and psychologists collectively address the multifactorial nature of post-traumatic sequelae, including chronic pain and psychosocial impacts.
Emerging evidence underscores the role of cognitive-behavioral therapy in mitigating pain catastrophizing, which can amplify disability and hinder rehabilitation adherence. Furthermore, telemedicine platforms are expanding access to expert consultations and remote monitoring, enhancing continuity of care.
Patients benefit most when care plans are individualized, dynamically adjusted based on progress, and informed by the latest evidence-based protocols.
For a comprehensive overview of state-of-the-art orthopedic diagnostic and therapeutic modalities, the American Academy of Orthopaedic Surgeons (AAOS) provides extensive resources and clinical guidelines.
Are you navigating complex orthopedic recovery after an auto accident? Engage with our expert community by sharing your questions or experiences below. Together, we can deepen understanding and optimize healing journeys.
Decoding Complex Orthopedic Trauma: Beyond the Obvious Injuries
Post-auto accident orthopedic trauma can be deceptively intricate, involving multi-structural damage that challenges both diagnosis and treatment. Beyond fractures and soft tissue injuries, clinicians must remain vigilant for occult pathologies such as subtle vertebral endplate fractures, micro-tears in ligaments, and early osteochondral lesions that may not manifest on initial imaging. These injuries, if overlooked, can precipitate chronic pain syndromes and functional impairment.
For example, damage to the thoracolumbar junction often escapes detection during routine evaluations but can contribute to persistent axial back pain and biomechanical instability. Advanced imaging modalities, including high-resolution MRI and CT scans with 3D reconstruction, are indispensable tools in unveiling these hidden complexities.
What Are the Latest Innovations in Orthopedic Diagnostic Imaging Post-Trauma?
Recent advancements in orthopedic imaging have revolutionized post-accident evaluations. Techniques such as diffusion tensor imaging (DTI) provide nuanced insights into nerve tract integrity, enhancing detection of nerve injuries secondary to disc herniations or vertebral fractures. Additionally, dynamic MRI assessments allow visualization of joint kinematics under physiological load, revealing instability not evident in static scans.
Moreover, ultrasonography has gained prominence as a real-time, radiation-free modality for assessing soft tissue injuries including ligamentous tears and muscle contusions. This modality permits guided interventions such as corticosteroid injections with precision, optimizing therapeutic outcomes.
Integrating these modalities into diagnostic protocols enables a more comprehensive understanding of injury patterns, facilitating personalized treatment strategies.
Harnessing Cutting-Edge Therapeutics: From Biologics to Minimally Invasive Surgery
Orthopedic treatment paradigms post-auto accident have evolved significantly, embracing biologic therapies and minimally invasive surgical techniques that prioritize tissue preservation and rapid recovery. Platelet-rich plasma (PRP) injections and stem cell therapies are increasingly utilized to stimulate regenerative processes in damaged ligaments and cartilage.
Minimally invasive spine surgeries, such as endoscopic discectomy and percutaneous vertebroplasty, reduce operative morbidity and hospital stay durations. These approaches are particularly valuable for patients with herniated discs or vertebral compression fractures, enabling symptom relief with expedited return to function.
Advanced rehabilitation programs now incorporate neuromuscular re-education and proprioceptive training, addressing not only structural healing but also functional restoration of movement patterns disrupted by trauma.
Integrating Multidisciplinary Care: The Future of Orthopedic Recovery Post-Accident
Optimal recovery from orthopedic injuries sustained in auto accidents increasingly depends on multidisciplinary collaboration. Physical therapists, pain specialists, orthopedic surgeons, and psychologists collectively address the multifactorial nature of post-traumatic sequelae, including chronic pain and psychosocial impacts.
Emerging evidence underscores the role of cognitive-behavioral therapy in mitigating pain catastrophizing, which can amplify disability and hinder rehabilitation adherence. Furthermore, telemedicine platforms are expanding access to expert consultations and remote monitoring, enhancing continuity of care.
Patients benefit most when care plans are individualized, dynamically adjusted based on progress, and informed by the latest evidence-based protocols.
For a comprehensive overview of state-of-the-art orthopedic diagnostic and therapeutic modalities, the American Academy of Orthopaedic Surgeons (AAOS) provides extensive resources and clinical guidelines.
Are you navigating complex orthopedic recovery after an auto accident? Engage with our expert community by sharing your questions or experiences below. Together, we can deepen understanding and optimize healing journeys.

Frequently Asked Questions (FAQ)
What are the most common orthopedic injuries following an auto accident?
Common orthopedic injuries include fractures, ligament sprains, muscle strains, whiplash affecting the cervical spine, herniated discs, and joint dislocations. While some injuries are immediately visible, many soft tissue and nerve-related injuries develop symptoms days or weeks later, necessitating careful monitoring and evaluation.
Why is early orthopedic evaluation important after a car accident?
Early evaluation enables prompt identification of hidden injuries such as disc herniations or ligament tears that might not be evident initially. Timely diagnosis using advanced imaging can prevent progression to chronic pain, functional impairment, or disability, improving recovery outcomes through tailored treatment plans.
What diagnostic tools do orthopedic specialists use to detect hidden injuries?
Orthopedic specialists utilize a range of advanced modalities including MRI, CT scans with 3D reconstruction, diffusion tensor imaging (DTI), dynamic MRI for joint kinematics, and ultrasonography for soft tissue assessment. These techniques enhance detection of subtle fractures, nerve injuries, and soft tissue damage that standard X-rays might miss.
How effective are non-surgical treatments for orthopedic injuries after auto accidents?
Non-surgical treatments such as physical therapy, pain management injections (including platelet-rich plasma), and orthopedic bracing are often highly effective, especially when personalized based on injury severity and patient response. These approaches can reduce inflammation, restore mobility, and avoid the risks associated with surgery.
When should a patient consider seeking a second opinion or specialized care?
If symptoms persist, worsen, or plateau despite initial treatment, consulting a specialist or obtaining a second opinion is advisable. Complex cases involving nerve involvement, bulging discs, or biomechanical instability often benefit from evaluation by orthopedic spine specialists with access to comprehensive diagnostic services.
How do orthopedic evaluations intersect with legal claims after auto accidents?
Accurate and detailed orthopedic documentation substantiates injury severity, treatment necessity, and prognosis, which are critical in personal injury claims. Collaboration between orthopedic professionals and legal advocates ensures that medical evidence supports legal processes effectively.
What advancements in orthopedic therapeutics are shaping recovery today?
Emerging treatments include biologic therapies such as stem cell injections and platelet-rich plasma to promote tissue regeneration, minimally invasive surgeries like endoscopic discectomy, and integrative rehabilitation approaches incorporating neuromuscular re-education and cognitive-behavioral therapy to address both physical and psychological aspects of recovery.
How does multidisciplinary care improve outcomes after orthopedic trauma?
Multidisciplinary care involving orthopedic surgeons, physical therapists, pain specialists, and psychologists addresses the complex interplay of physical injury, pain management, and mental health. This holistic approach enhances functional recovery, reduces chronic pain risks, and supports patient adherence to rehabilitation protocols.
Can telemedicine support orthopedic recovery after an auto accident?
Yes, telemedicine facilitates remote consultations, monitoring, and rehabilitation guidance, improving access to expert care and continuity, especially for patients with mobility limitations or those living in underserved areas. It complements in-person care by enabling timely adjustments to treatment plans.
What should I do if I notice new or worsening symptoms weeks after an accident?
New or escalating symptoms such as persistent pain, numbness, weakness, or decreased range of motion warrant immediate orthopedic evaluation. Delayed presentation of injuries is common, and prompt reassessment can prevent long-term complications.
Trusted External Sources
- American Academy of Orthopaedic Surgeons (AAOS) – Provides comprehensive clinical guidelines, educational resources, and updates on best practices in orthopedic diagnosis and treatment, essential for understanding state-of-the-art post-accident care.
- Centers for Disease Control and Prevention (CDC) – Offers authoritative information on injury prevention, whiplash and soft tissue injury epidemiology, and public health guidelines relevant to auto accident trauma.
- National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) – A key research institution providing evidence-based insights into musculoskeletal disorders, rehabilitation, and emerging therapies that inform orthopedic clinical care.
- Journal of Orthopaedic Trauma – A peer-reviewed academic journal presenting cutting-edge research on complex trauma patterns, advanced imaging techniques, and innovative treatment modalities post-auto accidents.
- Insurance Research Council (IRC) – Offers data and analysis on the intersection of orthopedic injuries and insurance claims, aiding understanding of how medical documentation supports legal and administrative processes.
Conclusion: Advancing Orthopedic Care After Auto Accidents for Optimal Recovery
Orthopedic evaluation following auto accidents is a critical step in identifying both overt and subtle injuries that can impact long-term function and quality of life. Leveraging advanced diagnostic imaging and personalized, multidisciplinary treatment strategies—including innovative biologics and minimally invasive surgeries—enhances recovery trajectories and pain management. Furthermore, precise orthopedic documentation plays a vital role in supporting legal claims and ensuring comprehensive patient advocacy.
Patients are encouraged to seek early specialist consultation, maintain open communication with their care teams, and remain proactive in navigating insurance and authorization processes. Integrating emerging technologies such as telemedicine further expands access to expert guidance and continuous care.
Understanding the complexities of post-accident orthopedic trauma empowers patients and clinicians alike to optimize healing and restore mobility. We invite you to share your experiences, ask questions, and explore our related expert content to deepen your knowledge and support your recovery journey.


Reading this post really highlights how tricky orthopedic injuries after auto accidents can be, especially those that don’t show immediate symptoms. I appreciate the emphasis on persistent or unusual pain as a signal to seek evaluation. From my own experience, I initially dismissed stiffness and mild tingling after a minor car accident, assuming it was just muscle soreness. However, it eventually turned out that I had a small disc herniation requiring targeted physical therapy. Early imaging and diagnosis definitely made a huge difference in my recovery timeline. I’m curious, though, how do others balance the need to avoid unnecessary tests with ensuring subtle injuries aren’t missed? Are there particular signs or timelines you follow before pushing for more advanced imaging like MRI? And in your experience, how accessible are specialists who offer comprehensive orthopedic evaluations promptly after an accident, especially for those navigating insurance hurdles? I’d love to hear strategies or experiences from the community about advocating effectively for timely diagnosis and care after auto accidents.
Marissa, your question about balancing the need for timely advanced imaging versus avoiding unnecessary tests is really important. From my observation, one effective approach is closely monitoring symptom progression over the first couple of weeks post-accident. Persistent or worsening signs like radiating pain, numbness, or functional limitations should prompt earlier MRI evaluation. Waiting too long risks missing hidden injuries, but unnecessary early imaging can also create strain on healthcare resources and insurance approvals. In terms of accessibility, I’ve found that in many urban areas, specialists offering comprehensive orthopedic evaluations can be booked relatively quickly, but insurance authorizations often cause frustrating delays. Patient advocacy becomes crucial here—maintain thorough documentation of symptoms, insist on referrals when red flags arise, and don’t hesitate to escalate to patient care coordinators or use prior authorization support services if available. Has anyone else found telemedicine helpful for quicker initial specialist consultations to triage the urgency of imaging? Considering the legal implications mentioned in the post, ensuring prompt and accurate diagnosis also supports claims if pursuing compensation. Overall, a proactive, informed approach seems to make a big difference in navigating both medical and administrative hurdles after an auto accident.
Marissa and Daniela, your points about balancing early imaging with avoiding unnecessary tests really resonate with me. From my experience after a rear-end collision, I found that careful symptom monitoring over the first two weeks was key. I was particularly alert to any escalating numbness or weakness, which prompted me to advocate for an MRI that revealed a small disc bulge. What helped was maintaining a detailed symptom diary—this documentation was invaluable not only for my orthopedic consultations but also when navigating insurance approvals. Regarding accessibility, I’ve noticed that while urban centers tend to have quicker orthopedic appointments, insurance prior authorizations often introduce frustrating delays. However, some clinics now offer telemedicine triage consultations, which helped me get preliminary advice on the urgency of imaging without needing in-person visits right away. I wonder if others here have found telemedicine a practical tool in expediting evaluations post-accident? Also, how do you strike a balance between patient advocacy and working collaboratively with insurance providers to avoid delays in care? It seems that fostering informed communication on all fronts really supports both health outcomes and legal claims, as highlighted in the post.
This post really highlights how crucial early and thorough orthopedic assessment is after an auto accident, especially when symptoms are subtle or delayed. I vividly remember experiencing neck stiffness and mild tingling a few days after a minor collision, which I initially brushed off. It wasn’t until the discomfort persisted and worsened that I sought medical evaluation—ultimately leading to a diagnosis of a herniated disc. The importance of advocating for imaging like MRI cannot be overstated, particularly because soft tissue injuries often don’t show up on initial X-rays. What I found helpful was keeping a symptom diary, which provided valuable details to my doctor and insurance provider. I wonder, in your experience, how do you balance the desire to avoid unnecessary tests with the need to detect hidden injuries early enough for effective treatment? Do you think telemedicine could streamline initial assessments and triage urgency, especially in our busy or resource-limited settings? Sharing strategies on timely evaluation could help others prevent long-term complications and ensure they get appropriate care as quickly as possible.
This comprehensive post really underscores the importance of early and thorough orthopedic assessment after accidents, especially given how many injuries can go unnoticed initially. From personal experience, I once underestimated neck stiffness following a minor collision, thinking it would resolve on its own. It lingered long enough that I finally sought specialized evaluation, which revealed a soft tissue injury that could have worsened without prompt care. I believe that maintaining a detailed symptom diary can be a game-changer, as it provides concrete evidence of progression and can support both medical and legal processes. In your opinion, what are the best ways for patients to advocate for timely advanced imaging without overdoing unnecessary tests? Also, have you found telemedicine especially useful in triaging injuries or cutting down wait times? It seems increasingly valuable, especially in areas with limited access to specialists. Ultimately, vigilance and proactive communication seem key to preventing long-term complications or chronic pain, which resonates deeply with this insightful article.
I completely agree with the emphasis this post places on the importance of early orthopedic evaluation following an auto accident, especially given how many injuries are not immediately obvious. From my own experience, I initially underestimated lingering neck stiffness after a minor collision, writing it off as muscle soreness. However, persistent discomfort and occasional numbness eventually led me to seek an orthopedic specialist. Early MRI imaging revealed a ligament sprain and subtle disc bulge that wouldn’t have been diagnosed otherwise. What truly helped was having a clear symptom timeline and communicating those details to my doctor. I’ve noticed that proactive patients who maintain detailed records tend to receive more thorough evaluations and care, which can also strengthen legal claims as noted in the article. I’m intrigued by the mention of telemedicine as a tool for preliminary consultations. Has anyone else used telemedicine for post-accident orthopedic assessments? How effective did you find it for determining the urgency of in-person imaging or treatment? Given the challenges with insurance approvals mentioned, I wonder if telehealth might become a more vital resource in speeding up access to care while still ensuring accurate diagnosis.