When Your Spine Goes Rogue: Welcome to the World of Spondylolisthesis
Picture this: your lower back starts sending mysterious signals—aching, stiffness, maybe a hint of numbness. Suddenly, you’re Googling “What is spondylolisthesis?” and wondering if your spine just decided to take a little slip-slide adventure without your permission. Spoiler alert: it did. Spondylolisthesis, that sneaky condition where a vertebra slips forward over the one beneath it, can turn everyday movements into a wincing exercise.
But before you imagine the operating room lights, there’s a compelling story of hope and healing: managing spondylolisthesis pain with non-surgical orthopedic care.
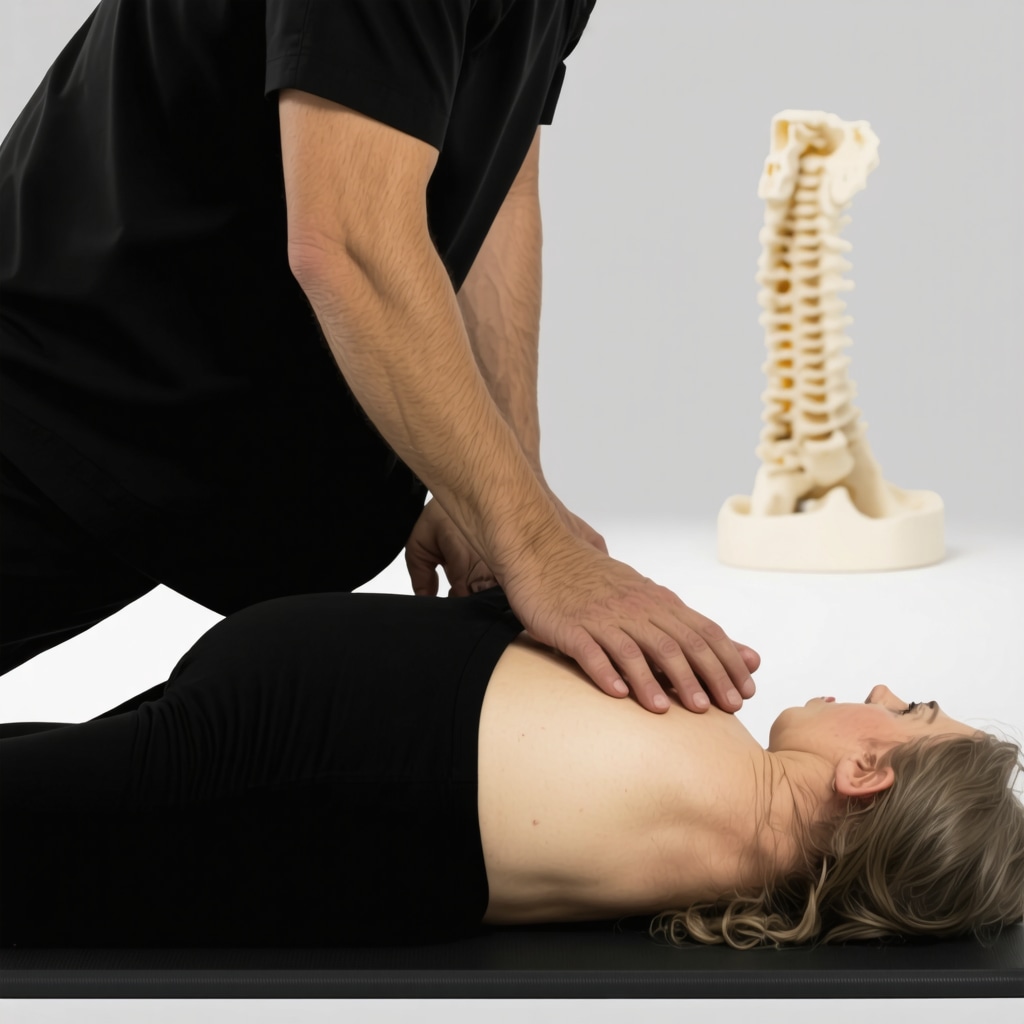
Non-Surgical Orthopedic Care: The Unsung Hero of Spine Pain Management
Why jump straight to surgery when the spine often prefers a gentler touch? Non-surgical approaches have become the first line of defense, offering relief without scalpels or hospital stays. From physical therapy that feels more like a guided dance to targeted orthopedic injections, the arsenal is surprisingly diverse. These treatments aim to stabilize the spine, reduce inflammation, and strengthen surrounding muscles — all while preserving your natural anatomy.
One orthopedic specialist I spoke with likened it to tuning a car engine. “You don’t replace the engine at the first sign of trouble,” they said. “You fine-tune it, replace the spark plugs, and keep it running smoothly.” That’s precisely the philosophy behind non-invasive care for spondylolisthesis.
Could Your Back Pain Actually Improve Without Surgery?
It’s a question that often hangs in the air during consultations. The answer? Yes, often yes. According to a study published by the National Institutes of Health, conservative treatments not only mitigate pain but can improve function significantly in many patients with mild to moderate spondylolisthesis. Physical therapy, pain management injections, bracing, and lifestyle modifications form the backbone of these strategies.
If you’re navigating this tricky terrain, consider exploring the effective orthopedic care options for spondylolisthesis in New Jersey. The right team can tailor a non-surgical plan that respects your unique spine story.
Why Trust the Process? A Personal Take
Having witnessed friends and family wrestle with back pain, I’ve seen the transformative power of non-surgical orthopedic care firsthand. It’s not just about pain relief — it’s about reclaiming your day-to-day life without the looming anxiety of surgery. Orthopedic care can feel like a partnership, a negotiation with your body that says, “Let’s work together to get you moving again.”
So, what’s your story? Have you or someone you know tackled spondylolisthesis without going under the knife? Share your experiences or questions in the comments below — your spine might just thank you for it.
Diving Deeper: The Role of Multidisciplinary Care in Spondylolisthesis
While traditional physical therapy and injections form the cornerstone of non-surgical management, an emerging trend in orthopedic care involves a multidisciplinary approach. This strategy integrates physical therapists, pain management specialists, and spine-focused orthopedic doctors to create a customized plan addressing every facet of spondylolisthesis symptoms. By combining expertise, patients often experience more comprehensive pain relief and improved spinal stability.
This model acknowledges that spondylolisthesis is not just a mechanical problem but also a complex interplay of neurological and muscular factors. For instance, addressing muscle imbalances around the lumbar spine through targeted strengthening exercises, coupled with precise pain modulation techniques like trigger point injections, can optimize recovery without surgery. This holistic care paradigm is increasingly recognized in leading back pain clinics across New Jersey.
Innovations in Orthopedic Injections: Beyond Traditional Pain Relief
Orthopedic injections have evolved beyond simple steroid shots. Platelet-rich plasma (PRP) therapy and regenerative medicine offer exciting possibilities for enhancing tissue healing in spondylolisthesis patients. These treatments aim to promote natural repair mechanisms in damaged ligaments and discs, potentially reducing instability and pain over the long term.
However, it’s crucial to consult with a specialist well-versed in these advanced techniques to determine suitability and expected outcomes. As reported by the American Academy of Orthopaedic Surgeons (AAOS), while still under research, regenerative therapies show promising results in managing spine-related conditions, including spondylolisthesis (AAOS, 2023). Patients considering these options should seek care from experienced orthopedic providers to ensure safety and efficacy.
Is Combining Orthopedic Support Bracing with Therapy the Key to Long-Term Stability?
Orthopedic braces often receive mixed reviews. Some patients swear by them for pain relief and improved posture, while others find them restrictive. The question remains: does combining bracing with a structured physical therapy program enhance long-term spinal stability in spondylolisthesis?
Current clinical insights suggest that when used judiciously, braces can offload stress from vulnerable vertebrae during activity, allowing muscles to strengthen without exacerbating slippage. This synergy between mechanical support and active rehabilitation may be a cornerstone of successful conservative management. For detailed guidance on orthopedic support braces tailored for spinal stability, you might find the comprehensive brace selection guide particularly helpful.
Understanding how to balance brace use without fostering dependency is essential and best navigated under expert supervision.
Practical Tips for Patients Navigating Non-Surgical Orthopedic Care
Managing spondylolisthesis non-surgically is a journey requiring patience, consistency, and informed decision-making. Here are key strategies to optimize outcomes:
- Active Participation: Engage fully in prescribed physical therapy and home exercise routines to build core strength and flexibility.
- Communication: Maintain open dialogue with your orthopedic care team about symptom changes or concerns, which can inform treatment adjustments.
- Lifestyle Modifications: Incorporate ergonomic adjustments, weight management, and low-impact aerobic activities to reduce spinal stress.
- Informed Choices: Educate yourself on emerging treatments and consult specialists about the benefits and risks.
For more comprehensive insights into non-surgical spine care, consider reviewing minimally invasive back pain treatments and non-surgical care options for related spinal conditions.
We Want to Hear From You!
Have you experienced success with non-surgical orthopedic treatments for spondylolisthesis or other spine conditions? What challenges or breakthroughs have shaped your journey? Share your stories, questions, or tips in the comments below to support others navigating similar paths. Your insights enrich our community and empower those seeking answers.
Unlocking the Science: Biomechanics and Muscle Synergy in Spondylolisthesis Rehabilitation
Understanding the intricate biomechanics of the lumbar spine is paramount when designing effective non-surgical interventions for spondylolisthesis. The subtle anterior slip of a vertebra disrupts normal load distribution, often leading to compensatory muscular adaptations that can either stabilize or exacerbate the condition. Recent biomechanical studies emphasize the crucial role of deep stabilizing muscles—such as the multifidus and transversus abdominis—in maintaining spinal alignment and mitigating slippage progression.
Targeted rehabilitation programs that focus on reactivating these deep core muscles, rather than just general strengthening, have demonstrated superior outcomes in pain reduction and functional improvement. This nuanced approach leverages neuromuscular retraining techniques to restore optimal muscle timing and coordination, thereby reinforcing spinal integrity from within.
What Are the Latest Evidence-Based Protocols for Neuromuscular Training in Spondylolisthesis?
Emerging protocols incorporate biofeedback, electromyographic (EMG) monitoring, and progressive load challenges tailored to individual patient biomechanics. A landmark clinical trial published in the Spine Journal demonstrated that patients undergoing an 8-week neuromuscular training regimen exhibited a 40% greater improvement in lumbar stability compared to standard physical therapy alone.
This protocol emphasizes a phased approach: initial activation of deep stabilizers with low-load exercises, progressing to dynamic functional movements that simulate daily activities without provoking slippage. Integrating such sophisticated techniques into orthopedic care demands collaboration between physiotherapists and spine specialists well-versed in spinal pathomechanics.
Regenerative Orthopedics: Pioneering Tissue Repair and Spinal Stability Enhancement
Beyond symptom management, regenerative medicine is redefining possibilities by aiming to restore structural health at the cellular level. Treatments like Platelet-Rich Plasma (PRP) and autologous stem cell injections are gaining traction as adjuncts in the conservative management of spondylolisthesis. These biologics promote extracellular matrix remodeling, ligamentous strengthening, and may even retard or reverse degenerative changes contributing to vertebral instability.
However, patient selection is critical. Ideal candidates typically present with early-stage spondylolisthesis without gross mechanical instability or significant neurological compromise. The timing, dosage, and delivery techniques of regenerative injections are finely tuned to maximize efficacy and minimize adverse effects.
Leading orthopedic centers in New Jersey are pioneering clinical protocols that combine regenerative therapies with tailored rehabilitation, creating synergistic effects that optimize spinal function and patient quality of life.
How Do Regenerative Therapies Compare to Traditional Steroid Injections in Long-Term Outcomes?
While corticosteroid injections provide potent short-term anti-inflammatory effects, they do not address the underlying tissue degeneration. Conversely, regenerative therapies aim for durable structural repair. A comparative study featured in Orthopaedic Journal of Sports Medicine (2023) found that patients receiving PRP experienced sustained pain relief and improved functional scores at 12 months post-treatment, outperforming steroid groups which showed diminishing benefits after three months.
Nonetheless, more extensive randomized controlled trials are necessary to establish standardized protocols and long-term safety profiles. Patients should consult orthopedic specialists who can evaluate the appropriateness of these innovative therapies within their comprehensive care plan.
Integrating Digital Health Technologies: The Future of Personalized Spine Care
The advent of wearable sensors, tele-rehabilitation platforms, and AI-driven analytics is transforming how spondylolisthesis patients engage with non-surgical care. These technologies enable continuous monitoring of spinal posture, movement patterns, and adherence to therapeutic exercises outside the clinic, facilitating real-time feedback and timely intervention adjustments.
For example, smart braces equipped with inertial measurement units can objectively assess vertebral motion and provide biofeedback cues, empowering patients to correct postural deviations proactively. Similarly, telemedicine consultations allow multidisciplinary teams to coordinate complex care plans seamlessly, ensuring consistent progression and addressing emerging issues promptly.
Such digital integration not only enhances treatment efficacy but also fosters patient empowerment, a critical factor in chronic spine condition management.
Where Can Patients Access Cutting-Edge Digital Orthopedic Care for Spondylolisthesis?
Several specialized centers in New Jersey now offer hybrid care models combining in-person expertise with digital tools. Exploring resources like the Digital Rehabilitation for Spine Conditions initiative can provide valuable insights and access to these advanced services.
Are you ready to elevate your spondylolisthesis management with state-of-the-art non-surgical approaches? Consult with experienced orthopedic professionals who integrate biomechanical expertise, regenerative medicine, and digital health technologies to craft a personalized path toward spinal stability and pain relief.
Harnessing the Power of Precision Orthopedic Rehabilitation: Tailoring Treatment to Your Spine’s Unique Needs
Not all spondylolisthesis cases are created equal, and neither should be their treatment plans. The key to successful non-surgical management lies in customizing rehabilitation protocols that address the intricate biomechanical and neuromuscular nuances of each patient’s lumbar spine. This personalized approach often involves detailed assessments by top spine specialists to discern subtle postural deviations and muscular imbalances that contribute to vertebral slippage.
By focusing on individualized corrective strategies—such as neuromuscular re-education combined with functional movement retraining—patients can achieve enhanced spinal stability while minimizing compensatory strain. Those looking to connect with leading orthopedic spine experts in New Jersey will find tailored consultations invaluable to crafting these nuanced care plans.
Regenerative Orthopedics Meets Cutting-Edge Diagnostics: The New Frontier in Spondylolisthesis Care
Emerging diagnostic tools like dynamic MRI and advanced motion analysis are revolutionizing how clinicians evaluate vertebral instability in spondylolisthesis. Coupled with regenerative orthopedic treatments—including Platelet-Rich Plasma (PRP) and stem cell injections—these technologies enable precise targeting of damaged ligaments and intervertebral discs to promote biological repair and improve mechanical function.
A recent comprehensive review in the European Spine Journal underscores the promise of combining regenerative therapies with biomechanical diagnostics to delay or even obviate the need for surgery in select patients. This integrative approach underscores the importance of multidisciplinary collaboration among orthopedic surgeons, radiologists, and rehabilitation specialists.
How Are Digital Health Technologies Transforming Patient Engagement and Outcome Tracking in Spondylolisthesis?
Digital health innovations are reshaping the landscape of non-surgical orthopedic care by empowering patients and clinicians alike. Wearable sensors and mobile applications facilitate continuous monitoring of spinal posture and adherence to therapeutic exercises, providing actionable biofeedback that fosters self-correction and sustained engagement.
Tele-rehabilitation platforms enable remote supervision and real-time modifications to therapy regimens, breaking down geographical barriers and enhancing convenience. Furthermore, AI-driven analytics offer predictive insights, helping providers anticipate flare-ups and adjust interventions proactively.
Centers embracing these technologies—such as the Digital Rehabilitation for Spine Conditions program in New Jersey—are setting new standards for personalized, data-informed spine care. Patients interested in integrating these innovations into their treatment journey are encouraged to explore these resources and discuss suitability with their orthopedic care teams.
Engage and Elevate Your Spine Health Journey
Are you navigating the complexities of spondylolisthesis and curious about these advanced non-surgical strategies? Have you experienced success with regenerative therapies or digital rehabilitation tools? Share your insights, questions, or experiences in the comments below—your voice helps cultivate a thriving community of informed patients and experts.
For those seeking a deeper dive into minimally invasive and non-surgical options that preserve spinal health, don’t miss our comprehensive guide to minimally invasive back pain treatments and our expert overview of non-surgical care for related spinal conditions. Your spine deserves care as advanced and unique as your story.
Expert Insights & Advanced Considerations
Neuromuscular Retraining as a Cornerstone of Long-Term Spinal Stability
The intricate biomechanics of spondylolisthesis demand more than generic strengthening exercises. Targeted neuromuscular retraining focusing on deep stabilizers like the multifidus and transversus abdominis has proven to restore precise muscle timing and coordination, reducing vertebral slippage progression and enhancing functional outcomes. This approach requires sophisticated assessment tools and expert guidance to maximize efficacy.
Integrating Regenerative Orthopedics for Structural Restoration
Emerging regenerative therapies such as Platelet-Rich Plasma (PRP) and autologous stem cell injections offer promising adjuncts by aiming to biologically repair damaged ligaments and discs. Unlike corticosteroid injections that only address inflammation temporarily, regenerative treatments target tissue remodeling, potentially delaying or obviating the need for surgery in appropriate candidates. Clinical discretion in patient selection and treatment protocols is critical for optimizing results.
Digital Health Technologies Revolutionizing Personalized Spine Care
Wearable sensors, tele-rehabilitation platforms, and AI-driven analytics are reshaping patient engagement and outcome tracking. These innovations enable continuous monitoring of spinal posture and exercise adherence, providing real-time biofeedback that empowers patients to self-correct and clinicians to tailor interventions dynamically. Such integration enhances treatment adherence and supports multidisciplinary coordination.
The Synergy of Multidisciplinary Collaboration
A coordinated team approach involving orthopedic surgeons, physical therapists, pain specialists, and radiologists ensures comprehensive evaluation and personalized care plans. This multidisciplinary model addresses the multifactorial nature of spondylolisthesis, combining biomechanical, neurological, and regenerative expertise to optimize non-surgical management and patient quality of life.
Curated Expert Resources
- Spine Journal: A leading peer-reviewed publication offering the latest clinical trial data and biomechanical research crucial for evidence-based non-surgical protocols in spondylolisthesis management (Neuromuscular Training Study).
- European Spine Journal: Provides comprehensive reviews on regenerative orthopedics and advanced diagnostic imaging techniques, underpinning the integration of biologics with cutting-edge diagnostics (Regenerative Therapies Review).
- American Academy of Orthopaedic Surgeons (AAOS): Authoritative guidelines and updates on the safety, efficacy, and evolving role of orthopedic injections and regenerative treatments (AAOS 2023 Report).
- Digital Rehabilitation for Spine Conditions (NJ): A pioneering program combining in-person expertise with wearable tech and telehealth, exemplifying the future of personalized non-surgical spine care (Digital Rehab Initiative).
- Top Orthopedic Spine Specialists to Trust in 2025: A curated selection of expert practitioners in New Jersey specializing in nuanced, patient-specific treatment plans for spondylolisthesis and related disorders (Orthopedic Experts NJ).
Final Expert Perspective
Non-surgical orthopedic care for spondylolisthesis is evolving into an art that combines precise biomechanical understanding, regenerative medicine, digital innovation, and multidisciplinary collaboration. By tailoring neuromuscular rehabilitation protocols and leveraging cutting-edge biologic treatments alongside real-time digital feedback, clinicians can offer patients a personalized, effective alternative to surgery that preserves spinal integrity and function.
For those navigating this complex condition, exploring advanced non-surgical strategies with trusted orthopedic spine specialists is essential. Engage with our community, share your experiences, and consider consulting experts featured in resources like Top Orthopedic Spine Specialists to Trust in 2025. Your spine’s story deserves care that is as innovative and unique as you are.
To deepen your understanding and optimize your treatment journey, explore our comprehensive guides on minimally invasive back pain treatments and effective non-surgical care for related spinal conditions. Embrace the future of spine health today.