Understanding Trigger Point Injections in Orthopedic Pain Management
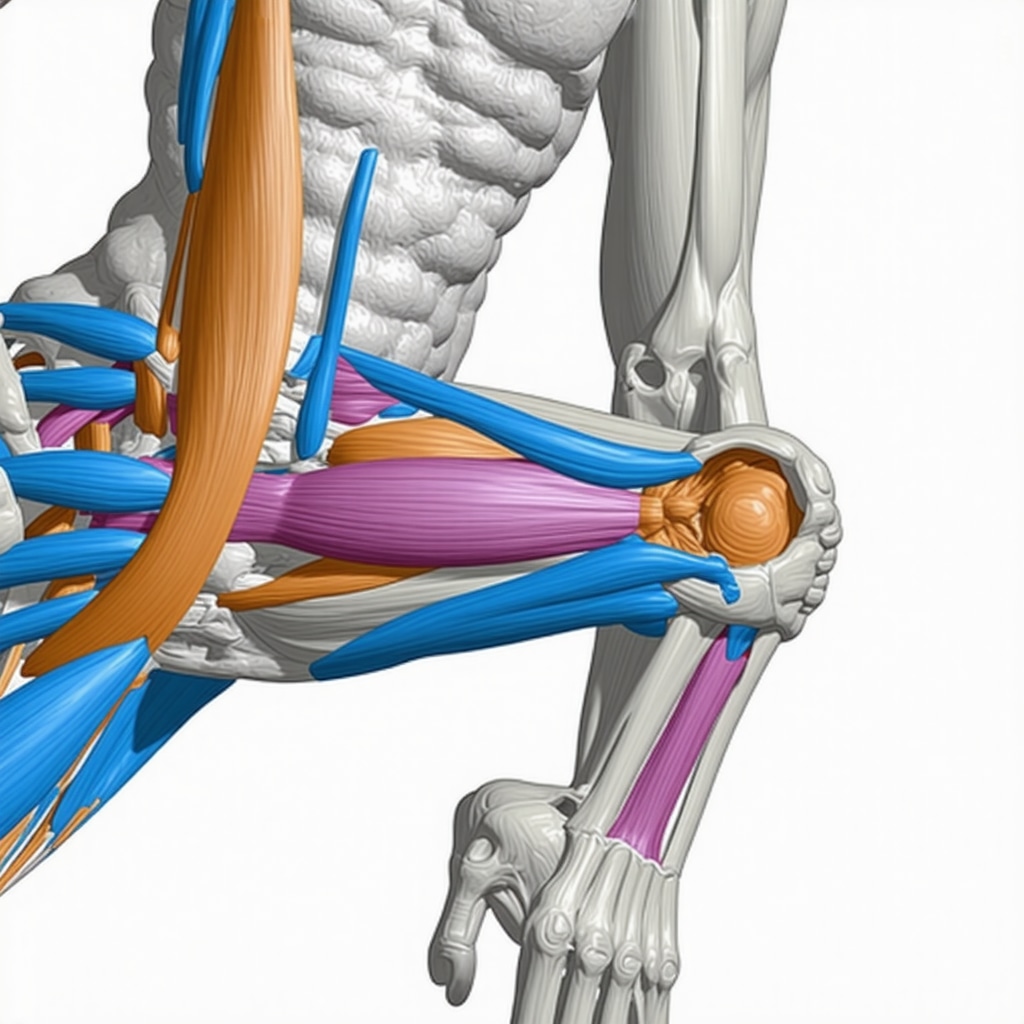
Trigger point injections (TPIs) represent a sophisticated approach in orthopedic pain management, targeting hyperirritable spots within skeletal muscle known as myofascial trigger points. These injections combine therapeutic precision with anatomical expertise to alleviate chronic musculoskeletal pain that is often resistant to conventional treatments. Rooted in detailed neuromuscular anatomy and pain physiology, TPIs serve as a pivotal intervention, particularly when integrated within multidisciplinary orthopedic care strategies.
The Mechanisms and Clinical Applications of Trigger Point Injections
At an expert level, TPIs function by disrupting the nociceptive feedback loop and facilitating muscle relaxation through direct administration of local anesthetics, corticosteroids, or saline solutions into the trigger points. This targeted delivery modulates peripheral and central sensitization mechanisms, reducing pain and improving functional mobility. Orthopedic specialists deploy TPIs for conditions such as myofascial pain syndrome, fibromyalgia adjunct treatment, and postural-related musculoskeletal dysfunctions, often in conjunction with physical therapy or advanced rehabilitation protocols.
What Are the Nuances and Challenges in Administering Trigger Point Injections Effectively?
Administering TPIs requires a nuanced understanding of musculoskeletal anatomy, palpation skills, and patient-specific pain patterns. Challenges include differentiating active trigger points from latent ones, avoiding neurovascular structures, and managing patient variability in pain perception and response. Imaging guidance, such as ultrasound, increasingly complements traditional palpation methods, enhancing accuracy and safety. Moreover, the selection of injectate and injection technique must be tailored to the patient’s diagnostic profile and comorbidities, underscoring the necessity for expert clinical judgment.
Integrating Trigger Point Injections Within Comprehensive Orthopedic Care Models
Trigger point injections are optimally utilized as part of a broader multidisciplinary orthopedic care model, which may include pharmacologic management, physical rehabilitation, and ergonomic adjustments. This integration maximizes therapeutic outcomes by addressing both symptomatic relief and underlying biomechanical contributors to pain. Contemporary research emphasizes individualized treatment plans, combining TPIs with non-surgical interventions to reduce reliance on systemic analgesics and invasive procedures.
For advanced insights into orthopedic rehabilitation following complex procedures, consider exploring our orthopedic rehab tips after lumbar fusion surgery.
Evidence-Based Perspectives and Future Directions in TPI Research
Peer-reviewed studies, such as those published in the Journal of Orthopaedic & Sports Physical Therapy, substantiate the efficacy of TPIs in reducing pain intensity and improving functional outcomes for selected patient populations. However, ongoing debates persist regarding optimal injectate composition and long-term benefits. Emerging innovations include biofeedback integration and regenerative medicine adjuncts, aiming to enhance the durability of pain relief while minimizing adverse effects.
Explore Further and Share Your Expertise
If you are a healthcare professional specializing in orthopedic pain management, we invite you to contribute your clinical experiences and insights on advanced injection techniques by visiting our contact page. Collaborative knowledge exchange is vital to advancing patient-centered care.
Optimizing Injection Techniques: Beyond Palpation to Ultrasound-Guided Precision
While traditional trigger point injection techniques rely heavily on tactile palpation to identify hyperirritable muscle nodules, advancements in imaging technology have revolutionized this approach. Ultrasound-guided trigger point injections enhance accuracy by visualizing muscle layers, adjacent neurovascular structures, and confirming needle placement in real time. This method reduces inadvertent injury risks and improves patient comfort, especially in anatomically complex regions such as the cervical spine or deep paraspinal muscles. Expert clinicians emphasize that combining palpatory findings with ultrasound guidance forms the gold standard for effective and safe TPIs.
Such innovations also facilitate tailored injectate delivery, allowing practitioners to distinguish between fibrotic and inflammatory tissue components within trigger points, ultimately optimizing therapeutic efficacy. For professionals interested in integrating ultrasound into their practice, reviewing comprehensive protocols can be invaluable.
Personalizing Injectate Selection: Balancing Efficacy and Safety
The choice of injectate is pivotal to TPI outcomes. Local anesthetics like lidocaine or bupivacaine provide immediate analgesia, while corticosteroids may reduce local inflammation and prolong pain relief in select cases. However, corticosteroid use raises concerns regarding potential muscle atrophy or systemic effects, necessitating judicious patient selection and dosage precision.
Emerging alternatives include saline injections and regenerative agents such as platelet-rich plasma (PRP), which aim to promote healing without the side effects associated with steroids. Current clinical trials suggest PRP may enhance tissue regeneration in chronic myofascial pain, though further research is required to establish standardized protocols. Integrating patient-specific factors—such as comorbidities, medication sensitivities, and pain chronicity—into injectate selection underscores the importance of individualized care plans.
How Can Multimodal Orthopedic Strategies Incorporate Trigger Point Injections for Sustainable Pain Relief?
Trigger point injections, while effective, are rarely standalone solutions. They yield the best results when integrated into comprehensive treatment regimens that address biomechanical imbalances, psychosocial factors, and functional impairments. Multimodal orthopedic strategies often combine TPIs with physical therapy modalities, ergonomic interventions, pharmacotherapy, and patient education to mitigate pain recurrence and improve quality of life.
For instance, addressing postural dysfunctions and muscle imbalances through targeted exercises complements the temporary relief provided by TPIs, fostering longer-term musculoskeletal health. Pain management specialists advocate for an individualized, biopsychosocial approach to chronic pain syndromes, recognizing that TPIs serve as a critical component rather than a cure-all.
To explore effective non-surgical interventions that often accompany TPIs in orthopedic care, visit our detailed guide on effective non-surgical care for herniated discs.
Expert Evidence and Clinical Guidelines Supporting Trigger Point Injection Use
A recent systematic review published in the Journal of Pain Research synthesizes clinical trial data, highlighting TPIs’ efficacy in reducing pain intensity and improving functional outcomes in patients with myofascial pain syndrome. The review emphasizes the importance of standardized injection protocols and outcome measures to advance clinical practice.
Furthermore, guidelines from professional orthopedic societies recommend TPIs as part of multimodal pain management, especially when conservative therapies alone fail to provide adequate relief. Ongoing research into optimizing dosing, frequency, and adjunct therapies continues to refine best practices for this intervention.
For those navigating orthopedic pain management complexities, understanding these evidence-based recommendations can enhance patient care strategies significantly.
Engage With Our Orthopedic Community
We encourage healthcare providers and patients alike to share their experiences and insights regarding trigger point injection therapies. Your contributions help enrich collective knowledge and improve treatment outcomes. Feel free to contact our team or comment below to participate in this evolving conversation.
Refining Patient Selection: Identifying Ideal Candidates for Trigger Point Injections
Given the heterogeneity of musculoskeletal pain presentations, expert clinicians emphasize the critical importance of meticulous patient selection to optimize trigger point injection outcomes. Beyond mere symptomatology, comprehensive assessment involves evaluating pain chronicity, psychosocial factors, and the presence of comorbid conditions such as neuropathic pain or systemic inflammatory diseases. Advanced diagnostic tools, including electromyography and functional MRI, are increasingly utilized to differentiate myofascial trigger points from other neuropathic or nociceptive pain sources, enabling tailored intervention strategies.
Moreover, understanding the interplay between central sensitization and peripheral trigger points informs prognostic predictions and guides adjunctive therapies. This nuanced approach ensures that TPIs are reserved for patients most likely to benefit, thereby enhancing resource allocation and clinical efficacy.
Innovations in Injectate Formulations: Exploring Regenerative and Biologic Therapies
The landscape of trigger point injection injectates is rapidly evolving, with regenerative medicine playing a transformative role. Platelet-rich plasma (PRP), autologous stem cells, and growth factor-enriched solutions have garnered attention for their potential to modulate the local microenvironment, promote tissue repair, and attenuate chronic inflammation. Clinical trials published in specialized journals such as Stem Cells Translational Medicine highlight promising outcomes, albeit emphasizing the need for standardized preparation protocols and long-term follow-up data.
Additionally, novel formulations combining local anesthetics with anti-fibrotic agents or neuromodulators are under investigation to synergistically address both pain and the underlying pathophysiology of trigger points. This frontier underscores the shift from symptomatic relief toward true tissue regeneration and functional restoration.
Can Advanced Imaging Biomarkers Enhance the Precision and Predictive Value of Trigger Point Injections?
Emerging research explores the utilization of advanced imaging biomarkers, such as elastography and diffusion tensor imaging, to characterize the biomechanical and microstructural properties of trigger points. These modalities offer quantitative data on tissue stiffness, fibrosis, and neural involvement, which may refine injection targeting and predict therapeutic responsiveness.
Incorporating such imaging biomarkers into clinical practice could revolutionize the current paradigm, facilitating personalized injection techniques and optimized injectate selection. However, challenges remain regarding accessibility, cost-effectiveness, and integration within routine orthopedic workflows.
Strategic Integration of Trigger Point Injections within Multidisciplinary Rehabilitation Frameworks
Trigger point injections achieve maximal benefit when embedded within strategic rehabilitation programs that integrate physical therapy, cognitive-behavioral therapy, and ergonomic interventions. Orthopedic specialists advocate for synchronized timing of TPIs with manual therapies and neuromuscular re-education to exploit windows of reduced pain and muscle hypertonicity.
This integrative approach not only enhances immediate symptom relief but also addresses perpetuating factors such as maladaptive movement patterns and psychosocial stressors, thereby reducing recurrence risk. Cutting-edge rehabilitation models incorporate wearable technology and biofeedback to monitor patient progress and adapt interventions dynamically.
For clinicians aiming to refine their multimodal treatment protocols, ongoing education on these integrative strategies is indispensable.
Engage with Our Expert Orthopedic Insights
We invite practitioners and researchers to deepen their expertise by accessing our comprehensive resources on advanced trigger point injection techniques and multidisciplinary management strategies. Connect with our orthopedic community via the contact page to share experiences or inquire about collaborative opportunities.
Leveraging Cutting-Edge Biomarkers to Elevate Trigger Point Injection Outcomes
The integration of advanced imaging biomarkers into trigger point injection protocols represents a paradigm shift in orthopedic pain management. Utilizing modalities like ultrasound elastography and diffusion tensor imaging, clinicians can quantify tissue stiffness and neural involvement within myofascial trigger points, thereby enhancing diagnostic precision and tailoring therapeutic interventions. These biomarkers facilitate differentiation between fibrotic and inflammatory tissue states, enabling a more nuanced selection of injectates and injection depths, ultimately optimizing analgesic efficacy and functional recovery.
However, despite promising initial data, widespread clinical adoption remains constrained by technical challenges, cost considerations, and the need for standardized interpretation frameworks.
Synergistic Multimodal Approaches: Integrating Regenerative Therapies with Trigger Point Injections
Emerging research underscores the potential of combining regenerative biologics, such as platelet-rich plasma (PRP) and mesenchymal stem cells, with traditional trigger point injections to foster tissue repair and attenuate chronic nociceptive signaling. These advanced formulations may modulate the local inflammatory milieu, stimulate angiogenesis, and promote extracellular matrix remodeling, thereby addressing the underlying pathophysiology rather than solely providing symptomatic relief.
Clinical trials documented in the Stem Cells Translational Medicine journal reveal encouraging outcomes, though further studies are essential to establish standardized protocols and long-term safety profiles.
How Does Real-Time Ultrasound Elastography Enhance Precision in Trigger Point Identification and Injection?
Real-time ultrasound elastography enables dynamic assessment of muscle tissue elasticity, offering a quantifiable measure of trigger point hardness and fibrosis. This facilitates more accurate localization and characterization of active trigger points, allowing clinicians to deliver injectates precisely where pathological tissue alterations are most pronounced. Such precision improves therapeutic outcomes, decreases procedural discomfort, and minimizes risks of inadvertent injury to adjacent neurovascular structures.
Implementing elastography-guided injections requires specialized training and equipment investment but promises to redefine best practices in myofascial pain interventions.
Augmenting Therapeutic Windows with Coordinated Rehabilitation Technologies
Strategically timed trigger point injections can be potentiated through integration with neuromuscular re-education and biofeedback mechanisms. Wearable sensor technologies and virtual reality platforms are increasingly employed to monitor muscle activation patterns and patient adherence to rehabilitative exercises post-injection. This data-driven approach enables real-time adjustments to therapy, promoting sustained functional improvements and reducing recurrence of trigger point activation.
Orthopedic specialists advocate for incorporating these technologies within multidisciplinary frameworks that also address psychosocial contributors to chronic pain, ensuring holistic patient management.
Engage with Advanced Orthopedic Pain Solutions
For clinicians and researchers dedicated to pioneering orthopedic pain management, exploring these advanced techniques and integrating regenerative strategies can significantly elevate patient outcomes. We invite you to connect with our expert community through the contact page to share insights, collaborate on innovative protocols, and stay abreast of evolving best practices in trigger point injection therapies.
Expert Insights & Advanced Considerations
Precision Through Multimodal Imaging Enhances Therapeutic Outcomes
Integrating real-time ultrasound elastography and diffusion tensor imaging into trigger point injection protocols allows clinicians to quantify tissue stiffness and neural involvement with unprecedented accuracy. This precision not only improves injectate delivery but also aids in prognostic assessment, tailoring intervention plans to individual patient pathology and enhancing overall pain relief efficacy.
Regenerative Biologics Are Reshaping the Future of Trigger Point Therapy
The advent of platelet-rich plasma (PRP) and mesenchymal stem cell adjuncts is shifting the paradigm from purely symptomatic relief to true tissue regeneration. These biologics modulate local inflammation and promote extracellular matrix remodeling, offering potential longer-term benefits for chronic myofascial pain syndromes when combined strategically with conventional TPIs.
Strategic Rehabilitation Synchronization Maximizes Injection Benefits
Optimal trigger point injection outcomes are achieved when coordinated with neuromuscular re-education, biofeedback, and ergonomic interventions. Emerging wearable technologies and virtual reality platforms facilitate dynamic monitoring of muscle activation and patient adherence, enabling clinicians to personalize rehabilitation and reduce recurrence risk effectively.
Patient Selection Is Paramount for Maximizing Efficacy
A meticulous assessment encompassing pain chronicity, psychosocial factors, and advanced diagnostics such as electromyography ensures that TPIs are reserved for candidates with the highest likelihood of benefit. This approach optimizes resource allocation and clinical outcomes, minimizing unnecessary interventions.
Balancing Injectate Choices with Safety and Efficacy
While local anesthetics provide immediate analgesia, and corticosteroids offer anti-inflammatory advantages, emerging alternatives like saline and regenerative agents present safer profiles for long-term use. Individualizing injectate selection based on patient-specific factors is essential to mitigate adverse effects and enhance therapeutic durability.
Curated Expert Resources
- Journal of Orthopaedic & Sports Physical Therapy: Offers peer-reviewed research on the efficacy and protocols of trigger point injections within multidisciplinary orthopedic care.
- Stem Cells Translational Medicine: Explores cutting-edge regenerative biologic therapies, including PRP and stem cell applications relevant to musculoskeletal pain management.
- Journal of Pain Research: Provides systematic reviews and clinical trial analyses on myofascial pain interventions, emphasizing standardized protocols and outcome measures.
- Ultrasound in Medicine and Biology: Focuses on advanced imaging modalities like elastography that enhance diagnostic precision for trigger point identification.
- Orthopedic Rehabilitation Guidelines – NJ Orthopedic Doctor: Comprehensive resources including orthopedic rehab tips after lumbar fusion surgery and effective non-surgical care for herniated discs, providing practical frameworks for integrating TPIs with rehabilitation.
Final Expert Perspective
Trigger point injections stand at the intersection of precise anatomical targeting and evolving regenerative medicine within orthopedic pain management. By leveraging advanced imaging biomarkers, personalizing injectate formulations, and embedding injections within synchronized rehabilitation frameworks, clinicians can achieve superior and sustained patient outcomes. Recognizing the criticality of patient selection and multimodal synergy underscores the nuanced expertise required to maximize TPI benefits. For those seeking to deepen their practice or navigate complex cases, engaging with our expert community through the contact page is a valuable step toward advancing your orthopedic pain management strategies.

Reading through this comprehensive guide on trigger point injections really highlights the intricate balance between anatomical knowledge and technological advances in orthopedic pain management. I’ve noticed in clinical settings that the move towards ultrasound-guided TPIs has made a significant difference, especially when dealing with tricky areas like the cervical spine where precision is critical. The integration of regenerative therapies like PRP alongside traditional injections also piques my interest — it seems to offer a promising avenue for sustained recovery rather than just symptomatic relief. However, from my experience, patient selection remains a persistent challenge: determining who will truly benefit from TPIs requires nuanced judgment beyond just identifying trigger points. It makes me wonder how fellow practitioners are incorporating psychosocial assessments or advanced imaging tools like elastography into their decision-making process to refine treatment plans. For those combining TPIs with rehabilitation, what strategies have you found effective in synchronizing injection timing with physical therapy to maximize recovery outcomes? I’d love to hear insights on balancing this multidisciplinary approach in daily practice and any tips on managing patient expectations for longer-term pain relief.