Back Pain Battles: The Tale of Two Specialists
So, you’ve been wrestling with that nagging back pain, and now you’re at a crossroads: Should you dial up an orthopedic surgeon or seek out a neurologist? It’s a classic showdown, like Batman vs. Superman, but with more MRI scans and fewer capes. Let’s dive into this intriguing contest where bones meet nerves, and see which specialist takes the crown for your spine’s salvation.
Orthopedic Doctors: The Bone Whisperers
Orthopedic specialists are the architects of the musculoskeletal system. They know their way around bones, joints, muscles, and ligaments like a seasoned locksmith knows keys and locks. If your back pain stems from structural issues—think herniated discs, spinal stenosis, or injuries from slip-and-fall accidents—they’re the pros who can set you straight. Their toolkit ranges from minimally invasive surgeries (check out advanced surgical options) to tailored physical therapy regimens. Their expertise shines brightest when the pain is rooted in mechanical dysfunction.
Neurologists: The Nerve Navigators
On the flip side, neurologists reign supreme in the realm of the nervous system. They’re the detectives in your back pain saga, hunting for nerve damage, neuropathies, or conditions like sciatica where nerves scream louder than muscles. Their approach is less about cutting and more about diagnosing complex nerve-related mysteries. Think of them as the Sherlock Holmes of nerve conduction studies and electromyography tests. When your pain radiates, tingles, or causes numbness, a neurologist’s insight is indispensable.
But here’s the million-dollar question: Can one specialist do it all?
Truth be told, back pain is rarely a one-trick pony. Often, it’s a tango between bones and nerves, muscles and membranes. That’s why many patients find themselves bouncing between these specialists or benefiting from collaborative care models. For instance, an orthopedic surgeon might address the physical damage while a neurologist manages nerve-related symptoms. This dual approach often paves the smoothest road to recovery.
Interestingly, recent studies highlight how interdisciplinary management improves outcomes in chronic back pain cases (source: NIH). So, don’t be shy about assembling your own A-team of back pain experts.
If you’re curious about how orthopedic care specifically tackles nerve compression issues, take a peek at this insightful guide on effective nerve compression treatments. It’s a fascinating glimpse into how these specialists overlap in their missions.
Got your own back pain adventure or a specialist story to share? Drop your thoughts below, and let’s get the conversation rolling. Your experience might just help someone else decide which superhero to call!
When Should You Prioritize an Orthopedic Surgeon Over a Neurologist?
Understanding the timing and context of when to seek an orthopedic surgeon versus a neurologist can significantly impact your treatment success. Orthopedic surgeons excel when your back pain is connected to structural abnormalities such as vertebral fractures, degenerative disc disease, or ligament injuries. For example, if imaging like X-rays or MRIs reveals bone spurs or disc herniations compressing the spinal cord or nerve roots, an orthopedic specialist’s intervention—either surgical or non-surgical—becomes crucial.
Additionally, orthopedic surgeons often coordinate post-operative rehabilitation and tailor physical therapy plans to restore mobility and strength. Their approach is holistic, ensuring that once the mechanical issue is corrected, the patient regains optimal function. For detailed rehabilitation strategies after lumbar fusion, explore orthopedic rehab tips after lumbar fusion surgery.
Neurologists: The Pioneers of Nerve-Centric Diagnoses and Treatments
Neurologists specialize in diagnosing complex nerve pathologies that might present as back pain but are fundamentally neurological. Conditions like peripheral neuropathy, multiple sclerosis, or radiculopathies need their expertise to navigate the intricate nervous system. Their arsenal includes nerve conduction studies and electromyography, which pinpoint the origin and severity of nerve involvement. This precision helps avoid unnecessary surgeries when the cause is purely neurological.
Moreover, neurologists often manage chronic neuropathic pain with pharmacological strategies, nerve blocks, or referrals to pain specialists. For patients experiencing persistent radiating pain or numbness, neurologist-led interventions can provide significant relief and improve quality of life.
How Can Collaborative Care Between Orthopedic Surgeons and Neurologists Enhance Back Pain Outcomes?
The interplay between the musculoskeletal and nervous systems means that back pain often requires a multidisciplinary approach. Collaborative care models, where orthopedic surgeons and neurologists work side-by-side, yield superior results. This synergy allows for comprehensive evaluation and tailored treatment plans addressing both mechanical and neurological contributors.
For example, an orthopedic surgeon might perform a minimally invasive discectomy to relieve nerve compression, while a neurologist manages residual neuropathic pain through medication or nerve blocks. This integrated approach not only accelerates recovery but also reduces the risk of chronic pain syndromes.
Research published in the Journal of Pain Research underscores that interdisciplinary management reduces patient disability and enhances satisfaction (source: Journal of Pain Research).
Curious about non-surgical options that bridge orthopedic and neurological care? Check out this comprehensive guide on effective non-surgical care for herniated discs.
Have you experienced the benefits of combined orthopedic and neurological care for back pain? Share your story or questions in the comments below to help others navigate their treatment journey.
Innovative Therapeutic Modalities at the Intersection of Orthopedics and Neurology
As our understanding of back pain evolves, so too does the therapeutic landscape, blending orthopedic and neurological expertise into integrative care pathways. Cutting-edge treatments such as neuromodulation techniques—including spinal cord stimulation and peripheral nerve stimulation—are increasingly pivotal in addressing refractory back pain cases where conventional interventions fall short. These modalities exploit electrical impulses to modulate pain signaling, offering an alternative to pharmacologic therapies and invasive surgeries.
Moreover, regenerative medicine approaches, like platelet-rich plasma (PRP) injections and mesenchymal stem cell therapies, are emerging as potential game-changers. By fostering tissue repair at a cellular level, these treatments target degenerative disc disease and chronic soft tissue injuries that often straddle orthopedic and neurological domains.
What Role Does Advanced Imaging Play in Differentiating Orthopedic vs. Neurological Back Pain Etiologies?
Distinguishing the precise etiology behind back pain remains a clinical challenge, often necessitating sophisticated imaging modalities beyond standard MRI or X-rays. High-resolution diffusion tensor imaging (DTI) and functional MRI (fMRI) provide unparalleled visualization of nerve tract integrity and functional neural activity.
DTI, for instance, allows clinicians to detect microstructural nerve injuries by mapping water diffusion along nerve fibers, which conventional imaging might overlook. These insights inform whether the pain source is predominantly mechanical compression or intrinsic nerve pathology, thereby guiding more tailored interventions.
Additionally, ultrasound elastography is gaining traction for its capacity to assess soft tissue stiffness and inflammation in paraspinal muscles and ligaments, bridging the diagnostic gap between musculoskeletal and neurogenic pain origins.
Enhancing Patient Outcomes Through Personalized Multidisciplinary Care Plans
The future of back pain management lies in bespoke treatment algorithms crafted from comprehensive clinical assessments, advanced diagnostics, and patient-specific factors such as genetics and psychosocial context. Integrating orthopedic and neurological perspectives within multidisciplinary teams facilitates dynamic treatment adjustments, optimizing pain control and functional restoration.
For instance, integrating cognitive-behavioral therapy (CBT) and pain neuroscience education alongside physical and pharmacological therapies addresses the complex biopsychosocial nature of chronic back pain. This holistic framework reduces reliance on opioid analgesics and minimizes the risk of chronic disability.
Furthermore, telemedicine platforms are becoming instrumental in sustaining ongoing multidisciplinary collaboration and patient engagement, particularly for postoperative rehabilitation and chronic pain monitoring.
To delve deeper into the nuances of such integrative approaches, explore this expert resource on interdisciplinary chronic back pain management strategies, which details evidence-based protocols enhancing patient-centered outcomes.
Are you navigating the complexities of back pain treatment? Engage with our community by sharing your experiences or questions below—your insights could illuminate the path for others embarking on their recovery journeys.
Decoding Back Pain: When to Choose Orthopedic Surgery vs. Neurological Care
Back pain can be an enigmatic puzzle, where the line between orthopedic and neurological causes blurs. Understanding the subtleties of when to prioritize one specialist over the other can dramatically influence your recovery journey. While orthopedic surgeons excel at structural corrections, neurologists shine in diagnosing and managing nerve-centric disorders. But what happens when the two domains overlap? Let’s unravel this complexity.
How Do Emerging Biomarkers and Genetic Profiles Influence Personalized Back Pain Treatment?
Recent advances in genomics and biomarker research are reshaping how clinicians approach back pain. Identifying specific genetic markers linked to disc degeneration or inflammation allows for stratified treatment protocols, tailoring interventions to individual biological predispositions. For example, patients exhibiting elevated pro-inflammatory cytokines may respond better to targeted anti-inflammatory therapies alongside orthopedic interventions.
This precision medicine approach fosters proactive care, potentially reducing the need for invasive surgeries. According to a 2023 review in Nature Reviews Rheumatology, integrating genetic profiling into back pain management protocols enhances patient outcomes by enabling earlier, customized therapeutic strategies (source: Nature Reviews Rheumatology).
For those interested in exploring non-invasive options that align with personalized care paradigms, check out our detailed guide on effective non-surgical care for herniated discs to understand how tailored therapies can complement orthopedic and neurological treatments.
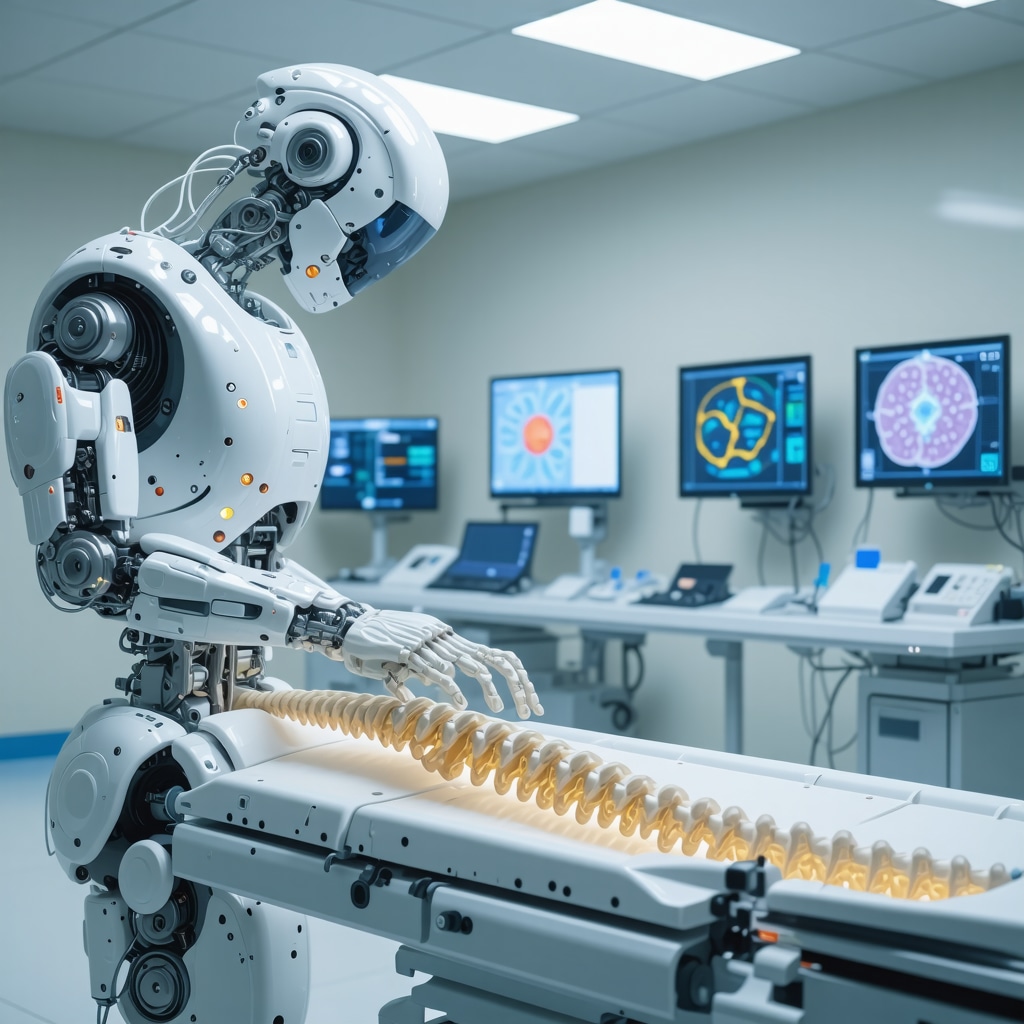
The Synergy of Advanced Robotics and AI in Orthopedic and Neurological Spine Treatments
Integrating robotics and artificial intelligence (AI) into spine care is no longer science fiction but a tangible reality enhancing precision and outcomes. Robotic-assisted surgeries enable orthopedic surgeons to navigate complex spinal anatomies with sub-millimeter accuracy, minimizing tissue disruption and accelerating recovery. Concurrently, AI algorithms analyze neurological data to predict pain patterns and optimize nerve-targeted therapies.
This convergence of technology not only refines surgical interventions but also aids neurologists in diagnosing elusive nerve pathologies through advanced pattern recognition in imaging and electrophysiological studies. Patients benefit from shorter hospital stays, reduced complications, and personalized treatment trajectories.
To explore how these cutting-edge innovations are transforming spine care, consider visiting our overview on minimally invasive back pain treatments explained and the impact of robotics in modern orthopedic surgery.
What Are the Psychological Dimensions in Chronic Back Pain, and How Can Integrated Care Address Them?
Chronic back pain is not purely a physical ailment; psychological factors such as anxiety, depression, and pain catastrophizing significantly modulate its perception and persistence. Neuroscience research highlights the role of central sensitization, where the nervous system amplifies pain signals, creating a feedback loop that complicates treatment.
Multidisciplinary programs combining orthopedic interventions, neurological pain management, and cognitive-behavioral therapy (CBT) are emerging as gold standards. These approaches address both the somatic and psychological facets of back pain, fostering resilience and functional improvement.
For a comprehensive exploration of multidisciplinary strategies, see our expert resource on interdisciplinary chronic back pain management strategies.
Your back pain story matters! Join the conversation by sharing your experiences or questions below. Engaging with a community of experts and fellow patients can illuminate new pathways to relief and recovery. And if you’re ready to take the next step, contact us to connect with top orthopedic spine specialists dedicated to personalized, cutting-edge care.
Expert Insights & Advanced Considerations
Precision Diagnostics Are Revolutionizing Specialist Selection
The emergence of advanced imaging techniques like diffusion tensor imaging (DTI) and functional MRI (fMRI) is reshaping how clinicians distinguish orthopedic from neurological back pain etiologies. These modalities provide granular visualization of nerve integrity and functional activity, enabling more targeted referrals and personalized treatment plans that optimize outcomes.
Interdisciplinary Collaboration Is the Gold Standard for Complex Back Pain
Back pain rarely fits neatly into a single specialty. The most successful interventions arise from integrated care pathways where orthopedic surgeons and neurologists co-manage patients. This synergy allows simultaneous addressing of structural abnormalities and nerve dysfunction, reducing chronic pain development and enhancing rehabilitation efficacy.
Genomic and Biomarker Profiling Enables Tailored Therapies
Incorporating genetic markers and inflammatory biomarkers into back pain evaluation facilitates stratified treatment approaches. For example, patients with pro-inflammatory cytokine elevations may benefit from adjunctive anti-inflammatory therapies alongside orthopedic interventions, paving the way for precision medicine in spine care.
Cutting-edge Therapeutics Are Bridging Orthopedics and Neurology
Innovations such as neuromodulation techniques (spinal cord and peripheral nerve stimulation) and regenerative medicine (PRP and stem cell therapies) exemplify the convergence of these specialties. These modalities address multifactorial pain mechanisms, offering options beyond conventional surgery or pharmacotherapy.
Psychosocial Factors Demand Integrated Pain Management Strategies
Recognition of central sensitization and psychological comorbidities in chronic back pain underscores the necessity of multidisciplinary treatment, including cognitive-behavioral therapy and pain neuroscience education. This holistic approach mitigates pain amplification and supports sustained functional recovery.
Curated Expert Resources
- National Institutes of Health (NIH) PMC Article on Interdisciplinary Chronic Back Pain Management: An evidence-based overview of collaborative strategies that enhance patient outcomes through integrated orthopedic and neurological care (read here).
- Nature Reviews Rheumatology – Genomics in Back Pain: A comprehensive review detailing how genetic and biomarker profiling is transforming personalized spine treatment (explore the article).
- Journal of Pain Research – Interdisciplinary Approaches: Highlights the clinical benefits of combined orthopedic and neurological interventions in reducing disability and improving quality of life (view study).
- NJ Orthopedic Doctor Resources: For practical patient-oriented guidance on minimally invasive treatments and non-surgical options, including minimally invasive back pain treatments and effective non-surgical care for herniated discs.
- Expert Orthopedic Spine Specialists in NJ: Discover leading specialists combining advanced orthopedic and neurological expertise for complex back pain cases (find top specialists).
Final Expert Perspective
Back pain management is evolving beyond traditional silos, demanding a nuanced understanding of both orthopedic and neurological dimensions. The integration of precision diagnostics, personalized medicine, and multidisciplinary collaboration represents the frontier of effective spine care. For patients and clinicians alike, embracing this holistic paradigm enhances diagnostic accuracy, optimizes therapeutic outcomes, and mitigates the risk of chronic disability.
If you’re navigating the complexities of back pain, consider exploring how to choose the right orthopedic surgeon and learn about non-surgical treatment options that bridge specialties. Engage with experts, share your experiences, and stay informed to make empowered decisions on your journey toward relief and recovery. Ready to take that step? Contact us to connect with top orthopedic spine specialists committed to personalized, cutting-edge care.


This post insightfully highlights the challenge many of us face when deciding between an orthopedic surgeon and a neurologist for back pain. From my experience, the collaboration between the two specialists is crucial because back pain rarely has a single cause. After dealing with persistent sciatica for months, I saw both specialists; my orthopedic doctor addressed the structural disc herniation causing nerve compression, and the neurologist managed the nerve pain through targeted nerve blocks. This team approach made a huge difference in my recovery, which aligns with the research cited here on interdisciplinary management. What intrigues me more is the role of advanced imaging like DTI to distinguish nerve injury versus mechanical issues—it seems like a game changer for personalized treatment plans. Has anyone else had an experience with such precision diagnostics? How did they influence your treatment path or outcomes? Also, with emerging regenerative therapies and neuromodulation techniques mentioned, I wonder how patients are deciding between these novel options and traditional surgical interventions? It would be great to hear more personal stories or clinical experiences about navigating these choices on the journey to relief.
This article sheds light on a crucial aspect of back pain management—recognizing when to seek either orthopedic or neurological expertise. Having experienced both sides, I can attest that early and accurate diagnosis is key. For instance, I initially saw an orthopedic specialist for what I thought was a mechanical issue, but persistent numbness and radiating pain prompted me to consult a neurologist. It turned out I had nerve compression that required specific neurological intervention. What I found interesting is the growing role of advanced imaging, like DTI, in differentiating nerve injuries from structural problems. I wonder, for those who’ve undergone these diagnostics, how much did they influence your treatment approach? Additionally, as regenerative therapies and neuromodulation are becoming more popular, how do clinicians determine the best route—surgery, regenerative medicine, or less invasive options? Are there clear guidelines to help patients navigate these choices, or is it still very case-dependent? Personally, I believe a multidisciplinary approach combining both orthopedic and neurological insights offers the best shot at long-term relief.