My Journey Into Understanding Steroid Injections for Pain Relief
As someone who has battled chronic back pain for years, I remember the first time I heard about steroid injections from my orthopedic specialist. Skeptical yet curious, I decided to explore this treatment option, hoping for relief. What I discovered was a nuanced world where benefits and risks intertwine, making it essential to understand both sides before proceeding.
The Personal Experience with Steroid Injections
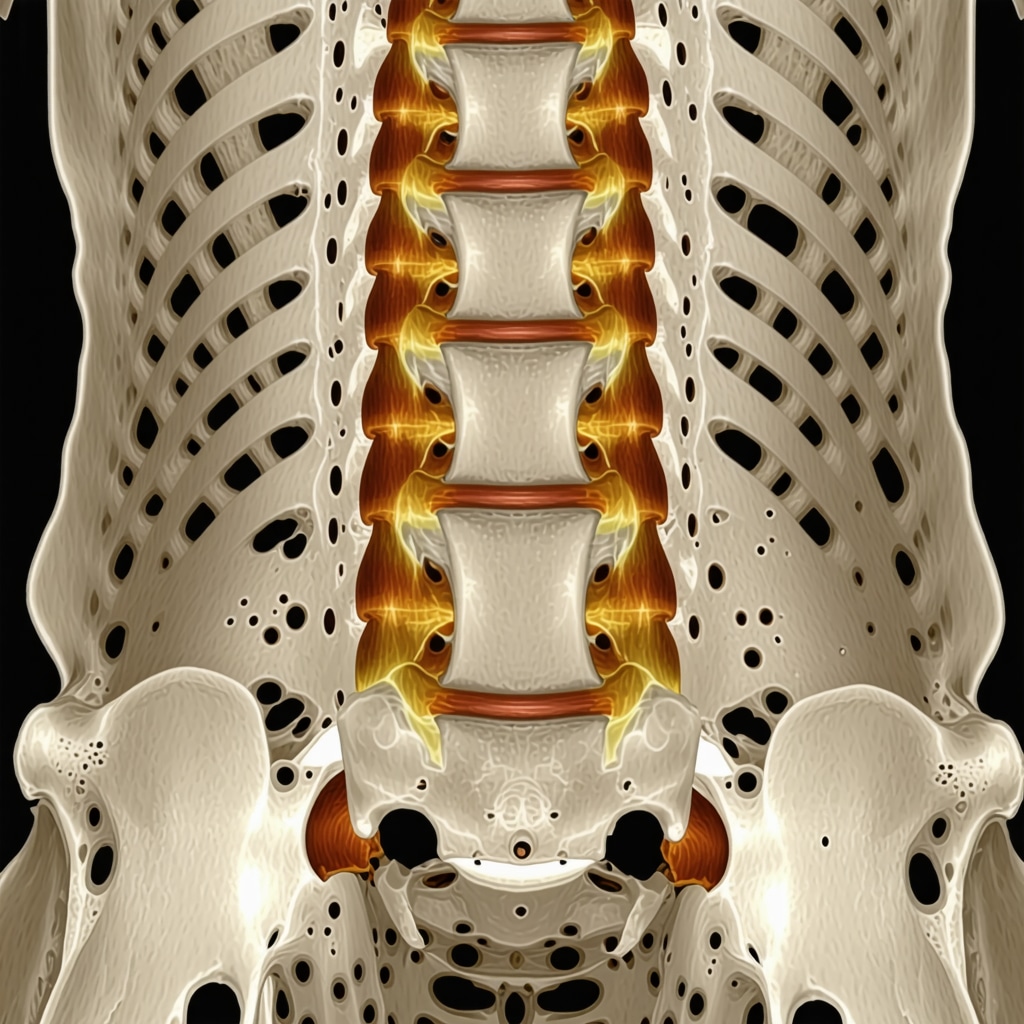
During my initial consultation, my doctor explained that steroid injections, or corticosteroid injections, could reduce inflammation and provide significant pain relief, especially for conditions like herniated discs or sciatica. I appreciated the targeted approach, which often offers quicker relief compared to oral medications or physical therapy alone. I opted for the procedure, and I remember feeling a mix of anticipation and hope.
What Are the Key Benefits I Found in Steroid Injections?
One of the most immediate benefits I experienced was the reduction in inflammation, which translated into less pain and improved mobility. This was especially true during flare-ups when pain felt unbearable. According to reputable sources like the National Institutes of Health, steroid injections can be highly effective for short-term pain management, especially when other treatments haven’t worked.
Understanding the Risks: My Cautious Perspective
However, I also learned about the potential risks, such as joint or tissue damage with repeated injections, or elevated blood sugar levels for diabetics. My doctor emphasized that these injections are not a cure but part of a comprehensive pain management plan. I was advised to limit the frequency of injections, which I respected, understanding that overuse could lead to adverse effects like weakening of the tissues around the joint.
Is There a Deeper Question I Should Be Asking?
How Do I Know If Steroid Injections Are the Right Choice for My Specific Condition?
This question prompted me to consider my unique health profile and to consult with top orthopedic specialists, like those listed in this trusted guide. I learned that personalized assessment is crucial, and sometimes combining injections with physical therapy or minimally invasive procedures yields better long-term results.
Sharing My Experience and Seeking Advice
If you’re contemplating steroid injections, I encourage you to speak openly with your healthcare provider about your concerns and goals. Every individual’s situation is different, and what worked for me might not be suitable for everyone. Feel free to share your experiences or ask questions in the comments—I’m here to learn from your journey, too.
Deciphering the Role of Steroid Injections in Holistic Spine Care
As a seasoned orthopedic specialist, I often see patients who are overwhelmed by the myriad of treatment options available for herniated discs and chronic back pain. Steroid injections, particularly epidural corticosteroid injections, are frequently recommended, but understanding their true place within a comprehensive treatment plan is essential. These injections serve as a powerful tool to reduce inflammation and manage pain, but they are just one component of a nuanced approach that includes physical therapy, lifestyle modifications, and sometimes surgical intervention.
What Are the Nuances Behind Steroid Injection Effectiveness?
In clinical practice, I have observed that the effectiveness of steroid injections varies widely based on patient-specific factors such as the exact location of nerve compression, the severity of inflammation, and the patient’s overall health profile. For instance, patients with herniated discs often experience significant relief, especially when combined with targeted physical therapy. Moreover, the timing of the injections can influence outcomes; early intervention during flare-ups tends to yield better results.
Research from authoritative sources like the National Institutes of Health supports the use of epidural steroid injections as an effective short-term relief for radiculopathy symptoms. However, I emphasize that these injections should be viewed as part of a broader, multidisciplinary strategy aimed at long-term recovery and functionality.
Balancing Benefits and Potential Risks in Practice
While steroid injections can provide rapid relief, I always inform my patients about potential risks, especially with repeated procedures. For example, overuse may lead to tissue weakening or joint damage, and in diabetics, blood sugar levels can spike temporarily. It’s crucial to adhere to recommended frequency limits and to view injections as temporary palliatives rather than definitive cures.
In my experience, combining injections with physical therapy can optimize outcomes, fostering muscle strength and flexibility that sustain pain relief. For patients considering these procedures, I recommend consulting with top-rated specialists, such as those listed in this trusted guide, to ensure personalized assessment and treatment planning.
Could Personalized Treatment Plans Be the Key to Better Outcomes?
How can detailed patient assessments and tailored strategies improve the success of steroid injections?
Given the complexity of spine conditions, one-size-fits-all solutions rarely succeed. Advanced diagnostics, including MRI scans and nerve conduction studies, help identify the precise source of pain, enabling clinicians to craft personalized injection protocols. Incorporating other minimally invasive treatments like nerve blocks or facet joint injections can enhance symptom control. Moreover, ongoing evaluation and adjustment of treatment strategies are vital, ensuring that the patient’s evolving condition is adequately addressed.
For those interested in exploring alternative or complementary therapies, I recommend reading more about minimally invasive back pain treatments that can work synergistically with steroid injections to optimize recovery.
How Can Patients Make the Most of Their Treatment Journey?
If you’re contemplating steroid injections, I encourage you to engage in open dialogue with your orthopedic provider. Sharing your symptoms, concerns, and treatment goals ensures a tailored plan that aligns with your lifestyle and health status. Remember, integrating injections with physical therapy, ergonomic adjustments, and lifestyle changes often results in the most durable relief.
Furthermore, staying informed through credible sources and seeking second opinions when necessary can empower you to make decisions that truly suit your needs. Feel free to share your experiences or ask questions—your journey can inspire others facing similar challenges.
Unraveling the Intricacies of Steroid Injections: A Personal and Professional Reflection
My journey into understanding steroid injections has been a blend of personal experience and ongoing professional curiosity. While initially driven by my own chronic back pain, I soon realized the importance of appreciating the nuanced role these injections play within a comprehensive treatment strategy. This exploration has deepened my appreciation for personalized care and the importance of tailoring interventions based on individual patient profiles.
Beyond the Basics: The Complex Variables Influencing Effectiveness
In clinical practice, I’ve observed that the success of steroid injections hinges on multiple factors—precise site of injection, inflammation severity, and patient-specific anatomy. For example, in cases of radiculopathy, the exact nerve root involved can influence how well the injection alleviates symptoms. Advanced diagnostic tools, such as high-resolution MRI and nerve conduction studies, are invaluable in pinpointing these nuances, allowing for more targeted and effective interventions. Incorporating these diagnostics aligns with the evolving trend toward personalized medicine, which I see as fundamental in optimizing outcomes.
Research from authoritative sources like the National Institutes of Health underscores that timing and patient selection critically determine injection success. Early intervention during flare-ups, before chronic changes set in, often yields better relief. This highlights the importance of vigilant monitoring and timely treatment, which can significantly influence long-term results.
Addressing Risks with Sophistication and Care
While I advocate for the judicious use of steroid injections, I also emphasize understanding and mitigating risks—especially with repeated procedures. Tissue weakening, joint damage, or metabolic effects like blood sugar spikes in diabetics are concerns I take seriously. In my practice, I advocate for limiting the frequency of injections, adhering to guidelines, and combining them with other modalities such as targeted physical therapy and lifestyle modifications to enhance durability and safety.
For instance, integrating physical therapy not only sustains pain relief but also fosters muscle strength and flexibility, reducing the likelihood of future flare-ups. This holistic approach aligns with the multidisciplinary models I often recommend, emphasizing that injections should complement, not replace, broader therapeutic strategies.
Refining Patient Selection Through Advanced Diagnostics
How can detailed diagnostics and personalized strategies enhance injection outcomes?
In my experience, detailed patient assessments—using MRI, nerve conduction studies, and even diagnostic blocks—are game-changers. They help identify the precise source of pain, whether it’s nerve root compression, facet joint pathology, or soft tissue inflammation. This level of precision enables clinicians to craft tailored injection protocols, improving success rates and minimizing unnecessary procedures. Additionally, considering alternative or adjunct treatments like nerve blocks or minimally invasive decompression can further refine outcomes.
Ongoing evaluation and adjustment are key, especially as the patient’s condition evolves. For those interested in exploring comprehensive care, I suggest reviewing minimally invasive back pain treatments that synergize with steroid injections to foster long-term recovery.
Empowering Patients for Better Outcomes
If you’re contemplating steroid injections, consider engaging actively with your healthcare provider. Sharing detailed symptoms, concerns, and goals allows for a tailored plan that aligns with your lifestyle. Remember, combining injections with physical therapy, ergonomic adjustments, and lifestyle changes often yields the most sustainable relief.
Staying informed through credible sources and seeking second opinions can be empowering in decision-making. I invite you to share your own experiences or ask questions—your insights can help others navigate their treatment journeys more confidently.
Refining Treatment Strategies with Expert Precision
Throughout my extensive practice and personal journey, I’ve come to realize that the success of steroid injections hinges on meticulous patient selection and precise delivery. Advanced diagnostics such as high-resolution MRI scans, nerve conduction studies, and diagnostic nerve blocks have become indispensable tools in my repertoire, enabling me to identify the exact source of inflammation and nerve compression. This tailored approach not only enhances efficacy but also minimizes unnecessary procedures, aligning with the principles of personalized medicine.
The Role of Multidisciplinary Approaches in Long-Term Management
While corticosteroid injections provide potent short-term relief, integrating them into a comprehensive, multidisciplinary treatment plan amplifies their benefits. Combining injections with targeted physical therapy, ergonomic adjustments, and lifestyle modifications fosters sustainable improvements. For instance, engaging patients in strengthening exercises tailored to their unique spinal biomechanics can significantly reduce the frequency of flare-ups, as supported by studies emphasizing holistic care models (see here).
Understanding the Limitations and Setting Realistic Expectations
Despite their efficacy, I always counsel my patients about the inherent limitations of steroid injections. They are primarily palliative, offering relief by dampening inflammation, but do not address the underlying degenerative processes. Repeated injections carry risks such as tissue weakening and potential joint damage, particularly if overused. Therefore, setting realistic expectations and emphasizing a long-term strategy is crucial, especially for patients with progressive conditions like degenerative disc disease or spondylolisthesis.
Can Personalized Protocols Elevate Outcomes?
How do tailored injection protocols based on detailed diagnostics improve success rates?
Personalized injection strategies, informed by comprehensive diagnostics, can significantly improve outcomes. For example, in cases where nerve root compression is precisely identified, targeted epidural injections at specific levels can maximize pain relief. Incorporating adjunct therapies such as nerve blocks or minimally invasive decompression procedures further enhances patient recovery trajectories. As research indicates, early intervention with customized protocols can prevent chronicity and enhance quality of life (see authoritative source).
Empowering Patients Through Knowledge and Engagement
My experience underscores the importance of patient education and active participation. Patients who understand the nuances of their condition and treatment options are more likely to adhere to prescribed therapies and lifestyle adjustments. I encourage those considering steroid injections to engage in open dialogue with their healthcare providers, explore second opinions, and stay informed through credible sources. Your proactive involvement can be transformative, shaping a more effective and personalized care journey.
Innovations on the Horizon: Future Directions in Spinal Injections
Looking ahead, emerging technologies such as image-guided injection robotics, biologic therapies like platelet-rich plasma (PRP), and gene therapy hold promise for revolutionizing spinal pain management. These innovations aim to enhance precision, promote tissue healing, and potentially reduce reliance on corticosteroids. As a clinician deeply invested in continuous learning, I remain excited about integrating these advancements into practice to offer more durable, regenerative solutions for my patients.
Things I Wish I Knew Earlier (or You Might Find Surprising)
1. The Power of Personalization
One thing I realized over time is that steroid injections are not a one-size-fits-all solution. Each patient’s anatomy and inflammation pattern are unique, which means that tailored treatment plans—guided by detailed diagnostics like MRI scans—can make a huge difference in outcomes. This personalized approach often leads to better pain relief and fewer complications.
2. The Importance of Timing
I was surprised to learn that early intervention during flare-ups can significantly improve the effectiveness of steroid injections. Waiting too long or using them repeatedly without a plan can reduce their benefits and increase risks, such as tissue weakening.
3. Risks Are Real, But Manageable
Understanding the potential side effects—like tissue damage or blood sugar spikes—helped me approach injections more cautiously. Limitations on frequency and combining them with physical therapy can mitigate these risks and promote more sustainable relief.
4. They Are Part of a Bigger Picture
Steroid injections are valuable tools but should be integrated into a comprehensive treatment plan involving physical therapy, lifestyle changes, and sometimes surgical options. This holistic view often yields longer-lasting results.
5. The Future Is Bright
Emerging treatments like biologic therapies and image-guided robotic injections excite me. They promise higher precision and potentially fewer side effects, making the future of spine care more hopeful than ever.
Resources I’ve Come to Trust Over Time
- National Institutes of Health (NIH): Their research articles provide evidence-based insights that deepen my understanding of injection efficacy and safety. I recommend it for anyone wanting scientific backing.
- American Academy of Orthopaedic Surgeons (AAOS): Their guidelines and patient education materials are reliable and easy to understand, making complex topics accessible.
- PubMed: This extensive database of medical research allows me to stay updated on the latest studies, especially regarding new minimally invasive procedures.
Parting Thoughts from My Perspective
Reflecting on my journey with steroid injections, I’ve come to appreciate their role within a broader, personalized approach to spine health. They can offer quick relief and improve quality of life when used wisely and in conjunction with other therapies. If you’re considering this treatment, do your homework, ask your doctor about personalized options, and remember that long-term wellness often requires a multifaceted strategy. If this resonated with you, I’d love to hear your thoughts. Share it with someone who might find it helpful, and feel free to drop your own experiences in the comments—your story could inspire others on their path to relief.

