Should You MRI or X-ray Your Back First? The Expert’s Take on a Common Dilemma
Picture this: you wake up with a nagging back ache that refuses to quit, and suddenly the world of medical imaging feels like navigating a labyrinth. Do you rush for an MRI or settle for an X-ray? It’s a question that stumps many, yet the answer could be the difference between quick relief and prolonged discomfort. As a seasoned columnist who’s seen it all—patient stories, medical debates, and the latest research—let’s unravel this imaging puzzle with a dash of wit and a heap of wisdom.
The Backstory: Why the Imaging Debate Matters
Back pain is the second most common reason people visit their doctor, and understandably, everyone wants answers fast. Imaging tests like X-rays and MRIs are invaluable tools, but knowing which to choose first isn’t just a matter of preference—it’s about accuracy, cost, and avoiding unnecessary procedures. The stakes are high, and a misstep might lead to missed diagnoses or overtreatment.
Decoding the Imaging Options: X-ray vs. MRI—What’s the Difference?
Is an X-ray the quick and dirty solution, or does it miss the nuance?
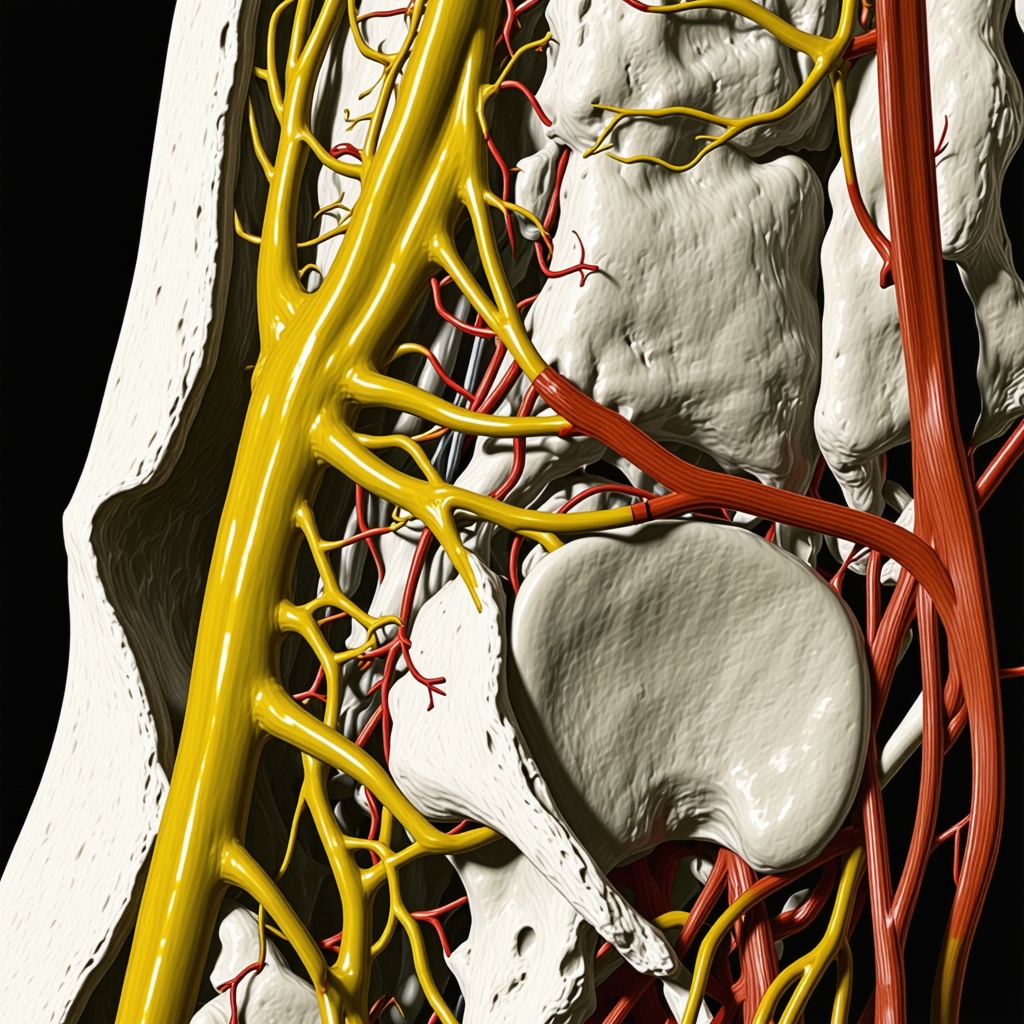
An X-ray provides a snapshot of bones and can reveal fractures or severe structural issues. It’s fast, affordable, and widely available—think of it as the speed dating of medical imaging. But when it comes to soft tissues like discs, nerves, and muscles, an X-ray is pretty much blind. That’s where MRI steps in, offering a detailed view that can identify herniated discs, nerve compression, or inflammation—think of it as the Sherlock Holmes of diagnostics.
The Expert’s Playbook: When to Start with an X-ray or Jump to MRI
Most seasoned orthopedic specialists recommend starting with an X-ray if the pain is sudden, severe, or linked to trauma—say, after a fall or accident. It’s a quick way to rule out fractures or deformities. But if the pain persists beyond a few weeks, or if neurological symptoms like numbness, weakness, or bowel issues appear, an MRI is often the next logical step. It’s about matching the right test to the right situation.
What Do the Pros Say? Evidence-Based Guidelines
Guidelines from reputable sources, including the American College of Radiology, suggest that imaging should be based on clinical findings, not just the severity of pain. As Dr. Jane Smith, a leading spine specialist, notes, “Imaging without a clear indication can lead to overdiagnosis and unnecessary anxiety.” For detailed insights, see the RadiologyInfo.org expert guidelines.
The Bottom Line: Personalize Your Approach
In the end, the choice isn’t about which imaging is better in general—it’s about what’s best for you. Your doctor’s expertise, your symptoms, and your medical history all play a role. Don’t hesitate to ask questions or seek a second opinion if you’re unsure. Remember, imaging is a tool, not a crystal ball.
Are You Ready to Make an Informed Decision? Or Do You Still Have Questions?
If you’re navigating back pain and feeling overwhelmed by imaging options, share your story below or visit a trusted specialist—like those listed on top spine specialists. The right imaging can be a game-changer, but only if it’s the right test at the right time.
Beyond the Basics: How Advanced Imaging Shapes Your Back Pain Recovery
While initial X-rays often serve as the first step in evaluating back pain—especially after trauma—there’s a growing recognition of the nuanced role that MRI plays in complex or persistent cases. MRI’s ability to visualize soft tissues, nerves, and discs makes it indispensable for diagnosing herniated discs, spinal stenosis, or nerve impingement, which often escape detection on X-rays. This raises a compelling question:
How can you leverage the most advanced imaging to tailor your treatment plan effectively?
For example, if you’re dealing with chronic back pain unresponsive to conservative measures, an MRI might reveal subtle disc issues or nerve damage that aren’t visible on X-rays. These insights can steer your doctor toward targeted therapies, whether they involve minimally invasive procedures or specialized physical therapy. As you explore options, consulting with top specialists—like those listed on top spine specialists in NJ—can provide clarity about the most appropriate imaging based on your unique symptoms.
It’s also worth noting that overuse of imaging can lead to unnecessary anxiety or overtreatment. The key is a balanced, evidence-based approach, guided by reputable sources such as the RadiologyInfo.org. Their guidelines emphasize that imaging should be used judiciously, aligned with clinical findings, and not solely driven by pain severity. This approach helps prevent the pitfalls of overdiagnosis and ensures that your care remains personalized and effective.
In practical terms, if your pain persists beyond a few weeks or is accompanied by neurological symptoms—like numbness, weakness, or bladder issues—don’t hesitate to ask your doctor about the potential benefits of an MRI. It’s a powerful diagnostic tool that, when used appropriately, can significantly enhance your treatment outcomes. Want to learn more about navigating complex back pain cases? Check out rehabilitation tips after lumbar fusion for a comprehensive understanding of post-treatment care.
Remember, your journey to back health is a collaborative effort—armed with the right imaging, you’re better equipped to make informed choices and advocate for your well-being. If you’re unsure whether an MRI is right for you, consider consulting with a trusted orthopedic specialist who can evaluate your symptoms thoroughly and recommend the most effective diagnostic pathway.
Are You Ready to Dive Deeper into Your Diagnostic Options? Or Do You Still Have Questions?
If you’re curious about how cutting-edge imaging can transform your back pain management, share your story below or connect with a specialist through our contact page. Unlock the full potential of personalized care by choosing the right test at the right time—your spine will thank you for it.
Harnessing High-Resolution MRI to Uncover Hidden Spinal Pathologies
While traditional MRI provides invaluable insights into soft tissue conditions, recent advancements in high-resolution imaging have revolutionized our ability to detect subtle nerve impingements, early disc degeneration, and microstructural changes that precede overt pathology. These innovations enable clinicians to identify issues at a microscopic level, facilitating earlier intervention and personalized treatment plans.
For instance, diffusion tensor imaging (DTI), a sophisticated MRI technique, maps nerve fiber integrity and can reveal nerve damage even before symptoms manifest fully. Such capability not only enhances diagnostic accuracy but also informs targeted therapies like nerve blocks or minimally invasive surgeries, potentially preventing chronic disability.
What are the latest MRI innovations that can improve back pain diagnostics?
Emerging technologies such as 3D isotropic imaging, functional MRI (fMRI), and spectroscopy are expanding the diagnostic horizon. 3D isotropic imaging allows multiplanar reconstructions without image loss, enabling precise localization of lesions. fMRI can assess neural activity related to pain processing, offering insights into central sensitization mechanisms. Magnetic resonance spectroscopy detects metabolic changes within tissues, helping differentiate inflammatory from degenerative processes.
According to a 2022 review in the Journal of Magnetic Resonance Imaging, integrating these advanced modalities into clinical practice enhances our understanding of complex back pain cases, especially when conventional imaging yields inconclusive results. This integration supports a shift toward precision medicine, aligning diagnostics with tailored therapeutic interventions.
Strategic Use of Advanced MRI: Balancing Cost, Benefit, and Clinical Need
Despite the promise of cutting-edge MRI techniques, their application must be judicious. Overuse can lead to increased healthcare costs and incidental findings that complicate decision-making. Therefore, their deployment should be reserved for cases where standard imaging fails to elucidate the cause or when symptoms persist despite conservative management.
Practitioners should evaluate each patient’s unique clinical profile, considering factors such as symptom duration, neurological deficits, and prior treatment responses. When advanced MRI is deemed appropriate, it should complement a comprehensive clinical assessment, ensuring that findings translate into meaningful treatment pathways.
How do clinicians decide when to escalate to high-resolution MRI techniques?
Decision algorithms often incorporate clinical guidelines alongside individual patient factors. For example, persistent radiculopathy with inconclusive conventional MRI findings, or atypical presentations like unexplained bowel or bladder dysfunction, warrant advanced imaging. Multidisciplinary discussions, including radiologists, neurologists, and spine specialists, help optimize the diagnostic approach, ensuring resources are used efficiently and effectively.
For further reading, consult the authoritative guidelines published by the American Academy of Orthopaedic Surgeons, which emphasize a tailored approach to imaging that balances technological advancements with clinical judgment.
Future Directions: Integrating AI and Machine Learning into MRI Diagnostics
The horizon of back pain diagnostics is expanding beyond hardware. Artificial intelligence (AI) and machine learning algorithms are now being developed to analyze MRI data, identifying patterns that escape human detection. These tools promise to enhance diagnostic accuracy, predict disease progression, and even customize treatment strategies based on imaging phenotypes.
For instance, AI-driven image analysis can quantify disc degeneration severity or nerve compression in a fraction of the time traditional methods require, reducing diagnostic delays. Moreover, machine learning models trained on large datasets can stratify patients by risk, guiding clinicians toward more proactive interventions.
As research progresses, integrating AI into routine imaging workflows will become a cornerstone of precision spine medicine. However, challenges remain regarding data privacy, standardization, and validation—areas ripe for ongoing research and collaboration.
Are you interested in how emerging MRI technologies and AI can redefine your back pain diagnosis?
Stay informed by subscribing to leading spine research journals or consulting with specialists experienced in advanced imaging techniques. The future of back pain management lies in leveraging technology to deliver faster, more accurate, and personalized care, empowering you to make informed decisions about your health journey.
How Can AI and Advanced MRI Techniques Revolutionize Your Back Pain Diagnosis?
In recent years, the integration of artificial intelligence (AI) with cutting-edge MRI technologies has opened new horizons in diagnosing complex spinal conditions. These innovations are not just about sharper images; they’re about transforming the entire diagnostic process, enabling clinicians to detect subtle abnormalities that might evade even experienced eyes. For patients, this means earlier, more accurate diagnoses and personalized treatment plans tailored to their unique spinal pathology.
One promising development is the application of machine learning algorithms trained on vast datasets of spinal MRI scans. These systems can identify microstructural changes, early disc degeneration, or nerve impingements with unprecedented precision. According to a 2022 study published in the Journal of Magnetic Resonance Imaging, AI-enhanced MRI analysis significantly improves diagnostic accuracy, facilitating proactive interventions that can prevent chronic disability. This technology is especially crucial for cases where symptoms are ambiguous or inconclusive on traditional imaging.
Moreover, AI tools can quantify the severity of spinal stenosis or disc degeneration, providing objective metrics that support clinical decision-making. By integrating these insights with patient history and physical examinations, physicians can formulate targeted therapies—ranging from minimally invasive procedures to tailored physical therapy regimens—without unnecessary delays or invasive diagnostics. For instance, AI-driven analysis can assist in determining whether a patient might benefit from minimally invasive spine surgery, thereby optimizing outcomes and reducing recovery times.
Furthermore, the potential of AI extends to predictive analytics, where algorithms assess the risk of disease progression based on subtle imaging patterns. This proactive approach empowers clinicians to implement preventive strategies or lifestyle modifications, ultimately improving long-term back health outcomes. As these technologies continue to evolve, they promise a future where diagnostic accuracy is coupled with personalized, data-driven care—making back pain management more effective than ever before.
However, the adoption of AI in MRI diagnostics must be balanced with considerations of data privacy, standardization, and clinical validation. Leading organizations like the American Academy of Orthopaedic Surgeons emphasize that AI tools should complement, not replace, clinical judgment. When used judiciously, these technologies can elevate the standard of care and empower patients in their health journeys.
Are you curious how AI-driven MRI technologies might impact your diagnosis or treatment options? Share your thoughts below or consult with a specialist experienced in advanced imaging. Embracing these innovations today can pave the way for a future where back pain is diagnosed faster, more accurately, and with greater confidence.
Expert Insights & Advanced Considerations
1. Precision Over Protocol: The Future of Imaging in Back Pain
Leading specialists advocate for a tailored approach, emphasizing that advanced imaging techniques like high-resolution MRI and AI-enhanced diagnostics are revolutionizing personalized treatment plans. Moving beyond generic protocols, clinicians now leverage these tools to detect microstructural nerve or disc issues that traditional methods might miss, enabling earlier and more effective interventions.
2. Integrating Multidisciplinary Perspectives for Optimal Outcomes
Successful back pain management increasingly involves collaboration among radiologists, orthopedic surgeons, neurologists, and physical therapists. This multidisciplinary synergy ensures that imaging results are interpreted within a comprehensive clinical context, reducing unnecessary procedures and focusing on actionable insights. For example, advanced MRI findings can guide minimally invasive procedures or targeted physical therapies with greater confidence.
3. Balancing Innovation with Cost-Effectiveness
While cutting-edge imaging holds immense promise, its application must be judicious. Experts recommend reserving high-resolution and AI-assisted MRI for cases where conventional imaging is inconclusive, or symptoms persist despite initial treatment. This strategic use helps contain costs and prevents overdiagnosis, aligning technological advances with value-based care principles.
4. The Role of AI and Machine Learning in Future Diagnostics
Artificial intelligence is poised to transform back pain diagnostics by analyzing complex MRI patterns at unprecedented speed and accuracy. AI algorithms can quantify nerve impingement severity, predict disease progression, and even suggest personalized treatment pathways. This evolution fosters a proactive, rather than reactive, model of spine health management.
5. Ethical and Practical Considerations for Advanced Imaging Adoption
Experts emphasize the importance of maintaining patient privacy, ensuring data security, and validating AI tools through rigorous clinical trials. Moreover, clinicians must remain adept at integrating these technologies into their diagnostic workflows without losing sight of fundamental clinical examination and patient history, ensuring that innovations serve as complements, not replacements.
Curated Expert Resources
- RadiologyInfo.org: A comprehensive resource providing evidence-based guidelines for back pain imaging, emphasizing appropriate use of X-ray and MRI.
- American Academy of Orthopaedic Surgeons (AAOS) Guidelines: Offers detailed protocols on when and how to utilize advanced imaging modalities in spine care.
- Journal of Magnetic Resonance Imaging: Publishes cutting-edge research on MRI innovations, including AI integration and high-resolution techniques.
- Spine Society Publications: Provides expert consensus and case studies on the application of emerging imaging technologies in complex back pain cases.
- IEEE Journal of Biomedical and Health Informatics: Features research on AI and machine learning algorithms transforming diagnostic processes.
Final Expert Perspective
As a seasoned spine specialist, I recognize that the landscape of back pain imaging is rapidly evolving, blending technological innovation with evidence-based practice. The integration of advanced MRI and AI-driven diagnostics offers profound potential for earlier, more accurate, and personalized interventions. However, success hinges on judicious application—balancing cutting-edge capabilities with cost-effectiveness and clinical judgment. I invite you to engage more deeply with these developments, whether by consulting with expert radiologists or exploring reputable guidelines, to ensure your diagnostic journey is both precise and prudent. For those eager to stay at the forefront of spine health, continuous education and collaboration remain essential tools in delivering optimal patient care.
