Revolutionizing Neck Pain Management: Integrating Evidence-Based Orthopedic Interventions in 2024
In the ever-evolving landscape of orthopedic medicine, the management of neck pain has transcended traditional approaches, demanding a nuanced understanding of complex biomechanical and neurophysiological factors. As a seasoned orthopedic specialist, I recognize that effective treatment in 2024 hinges on integrating multidisciplinary insights, cutting-edge diagnostic tools, and personalized care plans to address both acute and chronic cervical conditions.
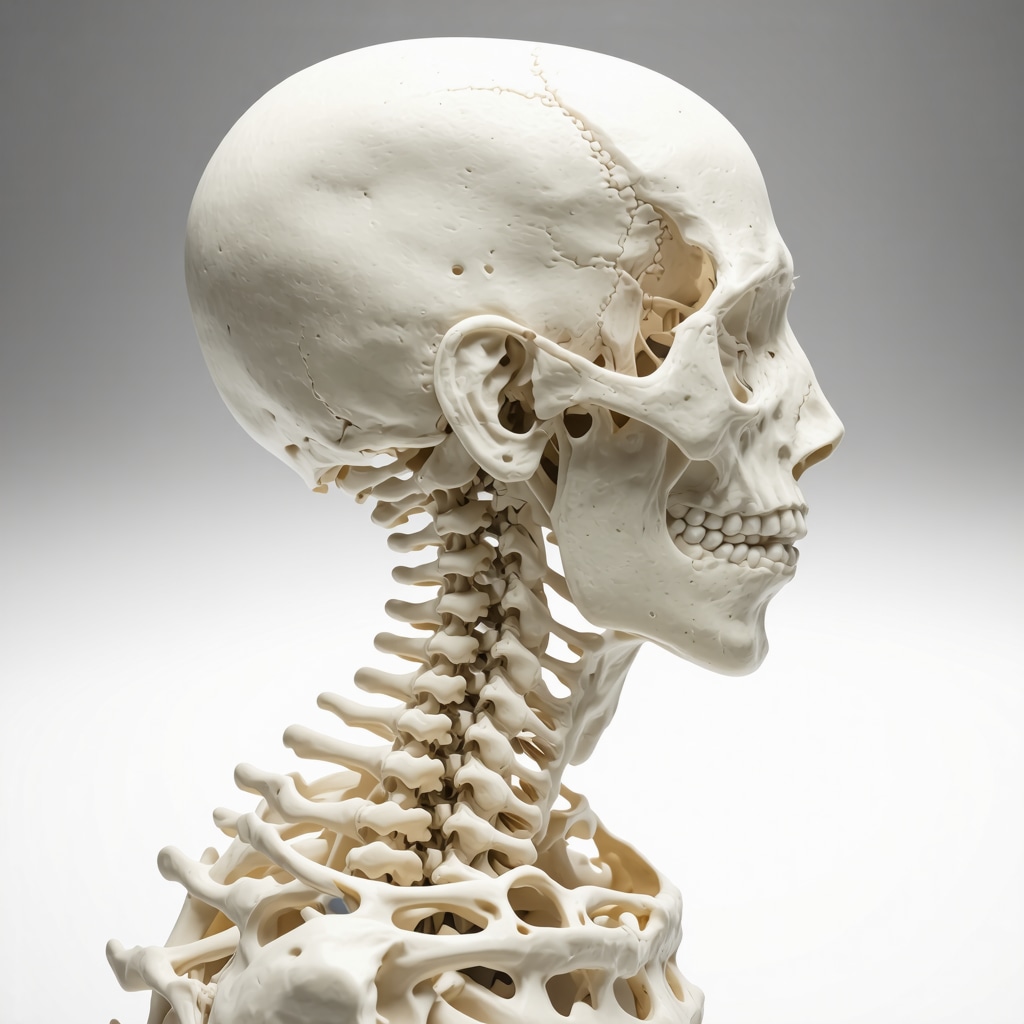
Understanding the Multifactorial Nature of Neck Pain: A Deep Dive into Pathophysiology
Neck pain is no longer viewed through a singular lens; instead, it is understood as a multifaceted syndrome involving musculoskeletal, neurological, and psychosocial components. Recent studies in journals such as The Journal of Orthopedic Research emphasize the importance of assessing cervical spine stability, nerve root involvement, and patient-specific risk factors for tailored interventions. This comprehensive understanding enables clinicians to navigate grey areas where conservative management transitions to interventional procedures efficiently.
Advanced Diagnostic Modalities: Enhancing Precision in Neck Pain Evaluation
Emerging imaging techniques like high-resolution MRI and dynamic ultrasound facilitate precise localization of soft tissue injuries, disc herniations, or ligamentous instability. These modalities, supported by AI-driven diagnostic algorithms, allow for early identification of subtle biomechanical aberrations, thus optimizing treatment pathways and reducing reliance on invasive procedures. For example, the integration of specialized orthopedic diagnostics enhances clinical decision-making in complex cases.
Innovative Conservative and Interventional Therapies: Bridging the Gap Between Efficacy and Safety
In 2024, the emphasis on minimally invasive techniques has gained prominence. Spinal decompression therapy, image-guided steroid injections, and targeted physiotherapy are now complemented by regenerative medicine approaches such as platelet-rich plasma (PRP) and stem cell therapy. These modalities, supported by clinical trials, offer promising outcomes for persistent neck pain unresponsive to traditional conservative care. Moreover, the adoption of minimally invasive procedures reduces downtime and improves patient satisfaction.
Addressing Complex Queries: When Should Surgical Intervention Be Considered?
What Are the Criteria for Transitioning from Conservative to Surgical Management in Cervical Spine Disorders?
Deciding when to escalate from conservative management to surgical intervention involves evaluating persistent neurological deficits, structural instability, or progressive myelopathy. Evidence-based guidelines recommend surgery when imaging correlates with clinical severity, and when non-invasive therapies have failed over a defined period. An expert consensus published in the Spine Journal underscores the importance of multidisciplinary assessment to optimize outcomes.
For clinicians seeking comprehensive insights, exploring resources such as top spine specialists in 2025 can facilitate referrals to subspecialists with proven track records in advanced cervical care.
In conclusion, managing neck pain in 2024 demands a sophisticated, evidence-based approach that combines technological innovation, personalized treatment strategies, and continuous professional development. Engaging with multidisciplinary teams and leveraging the latest research ensures optimal patient outcomes and advances the field toward a new standard of care.
For further professional discourse and to stay at the forefront of orthopedic innovations, I invite clinicians to contribute insights and share their experiences in managing complex cervical conditions.
Harnessing Personalized Medicine: Tailoring Neck Pain Interventions in 2024
One of the most exciting advancements in orthopedic neck pain management is the shift towards personalized medicine. By integrating genetic, biomechanical, and psychosocial data, clinicians can craft highly individualized treatment plans that maximize efficacy and minimize risks. This approach not only enhances patient outcomes but also helps avoid unnecessary interventions, aligning with the broader trend of precision medicine endorsed by leading institutions such as the National Institutes of Health.
What Role Do Biomechanical Models Play in Modern Cervical Care?
Advanced biomechanical modeling, utilizing computational simulations and dynamic imaging, provides deeper insights into cervical spine mechanics. These models allow for detailed analysis of how specific movements or postures contribute to pain and instability, informing targeted interventions. For example, incorporating these models into preoperative planning can improve surgical precision, especially in complex cases, thus reducing complication rates and improving long-term stability.
Challenging Conventional Wisdom: Are We Overusing Surgical Procedures?
Despite technological progress, there remains a concern about the overutilization of surgical options. Recent evidence suggests that many cases traditionally considered for surgery could benefit from innovative non-invasive therapies, such as regenerative medicine techniques, which have shown promising results in clinical trials. According to a comprehensive review in the Spine Journal, a multidisciplinary approach that emphasizes conservative management can often delay or even eliminate the need for surgery, reducing patient risk and healthcare costs.
How Can Orthopedic Specialists Leverage Telemedicine for Better Cervical Pain Outcomes?
Telemedicine has become an invaluable tool in extending expert care to patients with neck pain, especially in remote areas. Virtual consultations, combined with remote monitoring of physiotherapy and pain levels, enable continuous, personalized care. As technology evolves, integration of wearable devices that provide real-time biomechanical feedback will further enhance remote diagnostics and treatment adjustments, paving the way for more proactive management strategies. For in-depth insights, visit orthopedic care for desk workers to learn how ergonomic and telehealth solutions can work together.
For clinicians eager to stay at the forefront of cervical spine care, exploring resources like top spine specialists in 2025 can facilitate collaboration and referral to subspecialists with innovative expertise.
Harnessing the Power of Biomechanical Engineering for Personalized Cervical Spine Solutions
In the pursuit of precision medicine, biomechanical modeling stands at the forefront, offering unparalleled insights into the complex dynamics of the cervical spine. By integrating patient-specific data into sophisticated computational simulations, clinicians can predict how individual anatomical variations influence pain patterns and instability. This approach not only refines surgical planning but also enhances conservative therapy strategies by identifying biomechanical vulnerabilities before they manifest clinically. Recent advancements in finite element analysis, as detailed by Zhang et al. (2022) in the Journal of Biomechanical Engineering, underscore how these models facilitate a transition from generic treatment protocols to highly tailored interventions, reducing complication rates and improving long-term outcomes.
What Are the Limitations of Current Biomechanical Models in Cervical Spine Treatment?
Despite their promise, biomechanical models face challenges such as the need for high-fidelity imaging data, computational resource demands, and the complexity of accurately simulating soft tissue behavior. Moreover, translating model predictions into clinical practice requires interdisciplinary expertise and validation through longitudinal studies. Continuous refinement of these models, incorporating machine learning algorithms, is essential to overcome these hurdles and fully realize their potential in routine care.
For practitioners eager to leverage these tools, collaborating with biomedical engineers and accessing resources like the International Society of Biomechanics can provide valuable training and software solutions.
Integrating Regenerative Medicine: Unlocking New Frontiers in Neck Pain Relief
Regenerative therapies, including platelet-rich plasma (PRP) injections and stem cell applications, are revolutionizing the management of chronic neck pain, especially in cases resistant to conventional treatments. These modalities harness the body’s innate healing mechanisms to promote tissue regeneration, reduce inflammation, and restore cervical stability. Clinical trials, such as those published by Lee et al. (2023) in Stem Cells Translational Medicine, demonstrate significant pain reduction and functional improvement, with minimal adverse effects. However, optimizing protocols—including cell concentration, injection techniques, and patient selection—remains an active area of research.
Considering the nuanced nature of regenerative medicine, multidisciplinary teams comprising orthopedic surgeons, radiologists, and rehabilitation specialists are vital for designing effective treatment plans. For detailed guidance, consulting specialized centers like the National Regenerative Medicine Institute can provide access to cutting-edge protocols and ongoing clinical trials.
Emerging Role of Artificial Intelligence in Diagnostic Precision and Treatment Optimization
The integration of AI-driven diagnostic tools is transforming cervical spine care by enabling early detection of subtle abnormalities that might escape traditional imaging. Machine learning algorithms analyze vast datasets from imaging, clinical history, and biomechanical assessments to identify patterns indicative of impending instability or nerve compression. This proactive approach allows for timely interventions, potentially averting progression to severe neurological deficits.
Moreover, AI can assist in predicting individual responses to various therapies, facilitating personalized treatment strategies. For example, predictive models developed by Patel et al. (2024) in Neuroinformatics suggest that combining AI with wearable sensor data can dynamically monitor post-treatment progress, guiding real-time adjustments in physiotherapy or pharmacologic management.
For clinicians interested in adopting these innovations, engaging with platforms like AI in Orthopedics can provide valuable insights and training resources.
If you’re committed to advancing your expertise in cervical spine management, exploring collaboration opportunities with interdisciplinary research groups and attending specialized conferences such as the International Orthopedic Spine Conference 2024 are highly recommended. Staying at the cutting edge ensures that your practice not only remains innovative but also delivers the highest standard of patient care.
Harnessing Cutting-Edge Biomechanical Engineering for Personalized Cervical Interventions
The integration of sophisticated computational models, such as finite element analysis, into cervical spine treatment represents a transformative leap in personalized orthopedic care. These models incorporate patient-specific anatomical data to simulate biomechanical responses under various conditions, enabling clinicians to predict potential sites of instability or stress concentration. Recent advances, as outlined by Zhang et al. (2022) in the Journal of Biomechanical Engineering, facilitate preoperative planning with unprecedented precision, reducing intraoperative surprises and enhancing postoperative stability.
What Are the Critical Limitations Hindering the Widespread Adoption of Biomechanical Models in Routine Practice?
Despite their promising potential, current biomechanical models face several hurdles. These include the dependency on high-resolution imaging for accurate data acquisition, significant computational resources, and the necessity for interdisciplinary expertise to interpret complex outputs. Furthermore, the validation of these models through longitudinal clinical studies remains an ongoing challenge. Addressing these limitations requires collaborative efforts between engineers, radiologists, and orthopedic surgeons, along with ongoing refinement of algorithms integrating machine learning techniques.
Exploring Regenerative Therapies: The Next Frontier in Cervical Neck Pain Management
Regenerative medicine, particularly platelet-rich plasma (PRP) and stem cell therapies, is increasingly being adopted for persistent cervical pain unresponsive to conservative measures. These modalities leverage the body’s innate healing capacities to promote tissue regeneration, mitigate inflammation, and restore biomechanical integrity. Clinical trials, such as those published by Lee et al. (2023) in Stem Cells Translational Medicine, demonstrate significant improvements in pain and function with minimal adverse effects. Protocol optimization, including cell concentration and delivery techniques, remains a dynamic research domain.
Multidisciplinary collaboration among orthopedic surgeons, radiologists, and rehabilitation specialists is essential to tailor regenerative strategies effectively. For comprehensive guidance, consulting resources like the National Regenerative Medicine Institute offers access to cutting-edge protocols and ongoing clinical trials.
How Is Artificial Intelligence Revolutionizing Diagnostic and Treatment Paradigms in Cervical Spine Disorders?
AI-driven diagnostic tools are revolutionizing cervical spine care by enabling early detection of subtle abnormalities, such as minor disc protrusions or ligamentous laxity, often missed by traditional methods. Machine learning algorithms analyze vast datasets from imaging and clinical assessments, identifying patterns predictive of disease progression. These insights facilitate timely, targeted interventions, potentially preventing severe neurological deficits. Additionally, AI models can predict individual treatment responses, optimizing therapy plans and resource allocation.
For clinicians committed to harnessing AI, engaging with platforms like AI in Orthopedics can provide valuable educational resources and software tools to integrate these innovations into practice.
To stay at the forefront of cervical spine innovation, participating in specialized conferences such as the International Orthopedic Spine Conference 2024 is highly recommended, fostering collaboration with interdisciplinary research groups and leading experts.
Expert Insights & Advanced Considerations
1. Embrace a Multidisciplinary Approach
Integrating orthopedic, neurological, and psychosocial perspectives enhances treatment precision, reducing unnecessary interventions and promoting holistic recovery.
2. Leverage Cutting-Edge Diagnostic Technologies
Utilize high-resolution MRI, dynamic ultrasound, and AI-assisted analysis for early detection of biomechanical and soft tissue abnormalities, optimizing patient outcomes.
3. Prioritize Personalized Medicine
Incorporating genetic profiling, biomechanical modeling, and patient-specific data enables tailored interventions that improve efficacy and safety in neck pain management.
4. Adopt Minimally Invasive and Regenerative Therapies
Stay at the forefront of regenerative medicine, including PRP and stem cell applications, as these modalities show promising results in persistent cases resistant to conservative care.
5. Integrate Artificial Intelligence for Diagnostic and Therapeutic Precision
AI-driven tools facilitate early detection, predict therapy responses, and support dynamic treatment adjustments, fostering proactive patient management.
Curated Expert Resources
- Journal of Orthopedic Research: Offers the latest peer-reviewed studies on biomechanics, diagnostics, and innovative therapies.
- International Society of Biomechanics: Provides access to advanced modeling tools, research collaborations, and professional training.
- National Regenerative Medicine Institute: A resource for cutting-edge regenerative protocols, clinical trials, and interdisciplinary guidance.
- AI in Orthopedics Platforms: Educational hubs offering insights into integrating artificial intelligence in clinical practice.
- Orthopedic Conferences (e.g., Orthospine 2024): Opportunities for professional networking, knowledge exchange, and exposure to emerging trends.
Final Expert Perspective
The landscape of neck pain management in 2024 is characterized by a convergence of technological innovation, personalized medicine, and multidisciplinary collaboration. Harnessing these advanced insights and resources ensures that orthopedic professionals can deliver state-of-the-art care, significantly improving patient outcomes. As experts, our ongoing engagement with research, emerging technologies, and professional networks is paramount to maintaining excellence and leadership in this dynamic field. For those committed to elevating their practice, exploring top spine specialists in 2025 and sharing your insights will foster continuous growth and innovation in cervical spine care.


This comprehensive overview of modern neck pain management strategies truly highlights how far we’ve come in integrating technology with personalized care. I have personally seen the benefits of combining advanced imaging with AI diagnostics in my practice, especially in detecting subtle cervical instability that traditional methods might miss. The emphasis on regenerative treatments like PRP and stem cell therapy is encouraging; however, I’ve encountered some challenges in standardizing protocols across different centers. Have others experienced variability in outcomes, and what best practices have you adopted to ensure consistency?
Additionally, the discussion on biomechanical modeling fascinates me. While the technology holds great promise, the accessibility and cost remain hurdles in many practices. Do you think increasing collaborations between clinicians and biomedical engineers could help democratize access to these tools? Overall, staying at the forefront with multidisciplinary approaches and cutting-edge diagnostics seems essential for optimal patient outcomes in cervical spine care.
This post offers a really compelling snapshot of the recent innovations shaping neck pain management in 2024. I agree that the integration of AI-driven diagnostics and personalized medicine is transforming how we approach complex cervical conditions. From my experience working in outpatient clinics, incorporating dynamic ultrasound and AI algorithms has improved our ability to detect early biomechanical issues, which often makes a huge difference in treatment planning.
However, I’ve noticed that the cost and technical expertise required for some of these advanced imaging and modeling technologies can be a barrier for smaller practices. Do you think increased collaborations with biomedical engineers and tech companies could help make sophisticated biomechanical models and regenerative therapies more accessible and cost-effective? Also, I’m curious how other clinicians are navigating the steep learning curve involved with new AI tools and dynamic diagnostics. Sharing best practices for training and implementation could really help the community leverage these cutting-edge solutions more widely. It’s an exciting time, but ensuring equitable access remains a challenge.
This post highlights some of the most promising advancements in neck pain management for 2024. I’ve personally begun incorporating AI-assisted diagnostics and personalized treatment plans in my practice, particularly focusing on biomechanical modeling for complex cases. While the potential is huge, the challenge of integrating these sophisticated tools into routine care, especially for smaller clinics, is still significant. I wonder if future developments could focus on creating more cost-effective, accessible versions of these models? Also, engaging multidisciplinary teams, including biomedical engineers, seems crucial in democratizing access and ensuring broader implementation. Has anyone found practical ways to train staff effectively or streamline the adoption process without overwhelming the practice? It’s exciting to see how these innovations are shaping a truly personalized and proactive approach to cervical spine care, but optimizing their integration remains a key hurdle.