Why Every Orthopedic Note Should Be a Masterpiece, Not a Muddled Mess
Ever tried to piece together a jigsaw puzzle with missing pieces? That’s what it feels like for insurance adjusters and legal teams when orthopedic notes are vague or inconsistent. As a seasoned columnist in the world of medical documentation, I’ve seen firsthand how a well-crafted note can turn the tide in a workers’ compensation claim. Today, let’s dive into the art and science of documenting work injuries effectively, with some tips that even the most seasoned clinicians will find enlightening.
Cracking the Code: The Language of Orthopedic Notes
When it comes to orthopedic note language, clarity is king. Think of your notes as a story—one that accurately captures the injury, its impact, and the path to recovery. Use precise descriptions like “acute lumbar strain with restricted range of motion” instead of vague phrases like “back pain”. This specificity not only helps your colleagues but also ensures that insurance claims reflect the true extent of the injury.
Is Your Documentation Giving the Right Signals?
Ever wonder if your notes are sending the right message? Consider this: every detail, from the mechanism of injury to the patient’s functional limitations, should be clearly articulated. For example, documenting that a worker cannot lift more than 10 pounds or perform overhead activities provides concrete evidence of disability. Remember, insurance companies and legal entities trust detailed, factual descriptions over vague generalities.
How Can You Turn Standard Notes Into a Gold Standard?
Great question! The secret lies in consistency and accuracy. Use standardized orthopedic terminology, incorporate objective findings like range of motion tests, and document patient-reported symptoms meticulously. Also, don’t forget to include the impact on daily activities—this makes your notes not just reports but compelling narratives of real-world disability.
Moreover, linking your notes to relevant diagnostic codes (like those from the ICD-10 system) can streamline claims processing and reinforce the validity of your documentation. Remember, every word counts when it’s about advocating for your patient’s rightful compensation.
Sources That Speak Volumes
For a comprehensive guide on orthopedic note language, consult authoritative sources such as the American Academy of Orthopaedic Surgeons, which emphasizes clarity and precision in medical documentation (AAOS documentation guidelines). These standards are not just bureaucratic hoops—they’re essential tools for ensuring your notes serve their purpose effectively.
So, fellow clinicians, are your notes the silent advocates for your patients or just another checkbox? Share your thoughts below—let’s elevate our documentation game together!
The Nuanced Power of Precise Orthopedic Notes
Ever wondered how a single well-phrased sentence can influence the trajectory of a workers’ compensation claim? As a seasoned healthcare professional, I can attest that meticulous documentation is both an art and a science. Every detail you record—whether it’s the specific range of motion limitations or the precise mechanism of injury—serves as a cornerstone for advocacy and recovery.
Deciphering the Language of Effective Notes
Orthopedic notes are more than just clinical records; they are strategic tools. Using exact terminology like “rotator cuff tear with limited abduction” instead of vague descriptions ensures clarity and strengthens your case. Incorporate objective findings, such as joint stability tests or muscle strength grades, to substantiate your assessments. Remember, clarity and specificity forge trust with insurers and legal teams, facilitating smoother claims processing.
Is Your Documentation Sending the Right Message?
Consider this: every phrase in your note should reinforce the severity and impact of the injury. Documenting that a patient struggles with activities like lifting more than 5 pounds or performing overhead tasks provides tangible evidence of disability. Such detailed records are invaluable, especially when dealing with complex cases that require nuanced understanding beyond surface-level symptoms.
How Can We Transform Routine Notes Into Gold-Standard Documentation?
Transforming standard notes into authoritative documents hinges on consistency, precision, and strategic detail. Leverage standardized orthopedic terminology, include measurable objective data, and articulate the daily functional limitations faced by the patient. Connecting your notes with relevant diagnostic codes, such as ICD-10 classifications, further streamlines claims and enhances credibility (Learn more about ICD-10 coding here). The goal is to craft a compelling narrative that captures the injury’s real-world impact, championing your patient’s rightful compensation and recovery.
The Authority Behind the Standards
For a comprehensive understanding of documentation best practices, consult authoritative resources like the American Academy of Orthopaedic Surgeons, which underscores the importance of clarity, precision, and completeness in medical records (AAOS Guidelines). These standards serve as the backbone for effective advocacy and legal defensibility—ensuring your notes are not just routine entries but powerful tools for patient advocacy.
So, fellow clinicians, are your notes truly working for your patients? Or are they just mundane entries that fail to capture the full story? Share your insights below—let’s elevate our documentation game and make every word count!
Harnessing the Power of Digital Tools to Elevate Orthopedic Note Precision
In the digital age, leveraging advanced electronic health record (EHR) systems can significantly enhance the quality and consistency of orthopedic documentation. These platforms often come equipped with customizable templates, decision-support tools, and integrated coding systems that streamline the process of capturing detailed, standardized notes. For example, utilizing templates aligned with ICD-10 coding standards not only reduces variability but also ensures comprehensive coverage of injury specifics, aiding in faster claims processing and stronger legal defensibility.
The Critical Role of Objective Measurements in Litigation-Ready Notes
Objective data—such as goniometric measurements, muscle strength grades, and joint stability tests—serve as the backbone of compelling, evidence-based documentation. When meticulously recorded, these metrics transcend subjective impressions, providing quantifiable proof of impairment. Incorporating video recordings of physical examinations, when permissible, can further substantiate findings and demonstrate reproducibility—an invaluable asset in contentious legal scenarios. As noted by the American Medical Association, objective measurement standardization is essential for credible documentation (AMA Guidelines on Objective Measurements).
What Are the Nuances of Documenting Complex Injury Mechanisms?
When injuries involve multifaceted mechanisms—such as combined rotational and axial trauma—detailing the sequence, force vectors, and resultant biomechanical impacts becomes crucial. Precise descriptions help differentiate between acute injuries and pre-existing conditions, which can influence compensation outcomes. For instance, documenting that a worker experienced a fall from a height resulting in axial loading combined with twisting forces provides a nuanced understanding of injury causation, reinforcing the claim’s legitimacy. Mastery over such detailed narratives requires a deep understanding of biomechanics, often necessitating collaboration with specialists or biomechanical engineers.
Integrating Multidisciplinary Assessments for Holistic Documentation
In complex cases, incorporating insights from physical therapists, radiologists, and occupational therapists can create a multi-layered documentation approach. Cross-referenced reports—such as MRI findings indicating soft tissue damage coupled with functional assessments—offer a comprehensive picture of injury severity and impact. This multidisciplinary synthesis not only strengthens the medical narrative but also aligns with legal expectations for thorough, corroborated evidence, ultimately making your documentation a formidable tool for advocacy.
How Can You Future-Proof Your Orthopedic Notes Against Evolving Legal Standards?
Staying ahead in documentation quality involves continuous education on evolving legal standards, emerging injury patterns, and technological advancements. Regular training sessions, participation in professional forums, and engagement with authoritative guidelines—like those from the American Academy of Orthopaedic Surgeons—are vital. Moreover, embracing artificial intelligence-driven analysis tools can assist in identifying inconsistencies or omissions in notes, ensuring your documentation remains robust and defensible in a rapidly changing legal landscape (AAOS Advocacy Resources).

Are you ready to elevate your orthopedic documentation to expert level? Dive deeper into specialized training or consult with legal and coding professionals to refine your approach. Remember, every meticulously documented detail not only advocates for your patient but also fortifies your legal and professional credibility. For tailored advice or to discuss complex cases, consider reaching out to our expert team who can guide you through advanced documentation strategies.
Unlocking the Nuances of Expert-Level Orthopedic Documentation
Beyond the fundamental principles of clarity and precision, mastering the art of orthopedic note-taking involves understanding the subtle nuances that can sway legal and insurance outcomes. For instance, incorporating detailed biomechanical analyses when describing complex injury mechanisms can provide a compelling narrative that underscores causality. Think of your notes as a legal affidavit—each sentence should withstand scrutiny and contribute to a cohesive story of injury and impairment.
How Can Integrating Biomechanical Insights Enhance Your Documentation?
Integrating biomechanical insights into your notes involves detailed descriptions of injury mechanisms, such as specifying the force vectors and motion sequences involved during a fall or accident. This level of detail not only clarifies the injury’s origin but also differentiates acute trauma from pre-existing conditions, which is crucial in workers’ compensation cases. Collaborating with biomechanical engineers or utilizing specialized software can support these detailed narratives, elevating your documentation to an expert standard. For more on injury causation, consider reviewing resources like the AAOS legislative resources.
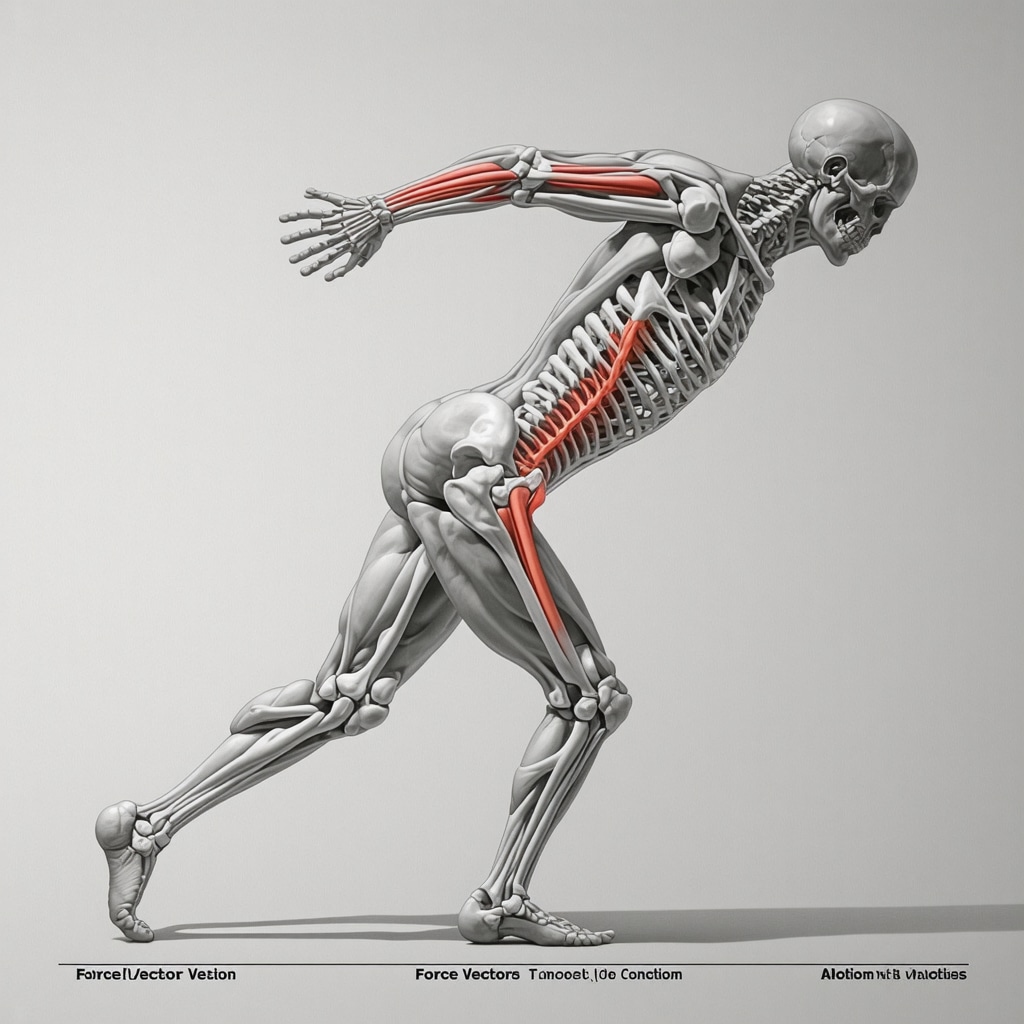
Incorporate detailed biomechanical diagrams or images demonstrating injury mechanisms to further strengthen your notes and provide visual clarity for legal review.
Can Multidisciplinary Collaboration Create a Holistic Medical Narrative?
Yes, fostering a multidisciplinary approach—integrating assessments from physical therapists, radiologists, and occupational therapists—can craft a comprehensive injury profile. When these reports are cross-referenced, it creates a robust, corroborated narrative that leaves little room for dispute. For example, MRI findings indicating soft tissue damage can be paired with functional assessments to highlight the injury’s real-world impact, reinforcing the case’s credibility. This approach aligns with best practices recommended by the American Medical Association.
What Are the Latest Technological Advances in Orthopedic Documentation?
Modern electronic health record (EHR) systems now incorporate AI-driven analytics and customizable templates that facilitate detailed, standardized documentation. These tools can automatically flag inconsistencies, suggest precise terminology, and ensure comprehensive coding adherence, such as with ICD-10 classifications. Utilizing these innovations not only improves accuracy but also future-proofs your documentation against evolving legal standards, as discussed in the AAOS guidelines. Embracing such technology positions clinicians at the forefront of expert documentation practices.
How Do Objective Measurements Fortify Your Legal Position?
Objective data—goniometric readings, muscle strength grades, and joint stability test results—serve as quantifiable evidence that supports your clinical assessments. When meticulously recorded, these measurements transcend subjective impressions, providing undeniable proof of impairment. Incorporating video recordings of physical examinations, where permissible, can further substantiate findings. The AMA emphasizes the importance of standardizing these measurements for legal credibility. This scientific rigor can be decisive in complex claims, ensuring your notes stand up to legal scrutiny.
Expert Insights & Advanced Considerations
1. Embrace Standardized Terminology
Utilize universally accepted orthopedic terms and coding systems like ICD-10 to ensure clarity and legal defensibility. This practice minimizes ambiguity and facilitates seamless insurance processing.
2. Incorporate Quantifiable Objective Data
Record measurable findings such as range of motion, muscle strength grades, and joint stability tests. These objective metrics provide undeniable evidence of impairment and support your clinical assessments.
3. Detail Injury Mechanisms with Biomechanical Precision
Describe the injury causation using biomechanical insights, including force vectors and motion sequences. Such detailed narratives can differentiate acute trauma from pre-existing conditions, strengthening your case.
4. Leverage Digital Tools for Consistency
Implement advanced EHR systems with customizable templates and decision-support features. These tools enhance note accuracy, standardization, and efficiency, safeguarding against omissions.
5. Foster Multidisciplinary Collaboration
Integrate reports from physical therapists, radiologists, and occupational therapists to create a comprehensive injury profile. Cross-referenced documentation offers a robust narrative, reducing disputes.
Curated Expert Resources
- American Academy of Orthopaedic Surgeons (AAOS): Offers authoritative guidelines on orthopedic documentation standards and best practices. (https://orthoinfo.aaos.org/)
- American Medical Association (AMA): Provides standardized physical exam measurement protocols vital for credible evidence. (https://www.ama-assn.org/practice-management/physician-health/standardized-physical-exam-measurements)
- CDC Injury Coding Resources: Essential for accurate injury classification and reporting. (https://www.cdc.gov/nchs/injury/injury_tools.htm)
- Electronic Health Record (EHR) System Guides: Best practices for utilizing digital platforms in orthopedic documentation.
Final Expert Perspective
In the realm of orthopedic work injury documentation, mastery lies in precision, clarity, and strategic detail. By integrating standardized terminology, objective measurements, biomechanical insights, and multidisciplinary inputs, clinicians can craft notes that not only advocate effectively for their patients but also stand resilient against legal scrutiny. Embracing advanced digital tools and authoritative guidelines ensures that your documentation remains future-proof amid evolving standards. Remember, every word in your note is a building block toward fair compensation and optimal recovery. Dive deeper into these strategies, refine your approach, and let your notes speak volumes—becoming your most powerful ally in advocacy and legal defense. Engage with fellow professionals and share your insights to elevate our collective standards in orthopedic documentation.

