Decoding Steroid Injections: A Powerful Ally in Orthopedic Care
In the realm of orthopedic treatment, steroid injections stand out as a potent therapeutic option, offering rapid relief for inflammation and pain in joints, tendons, and soft tissues. These injections, primarily consisting of corticosteroids, target inflammatory responses that underpin conditions such as arthritis, bursitis, and tendonitis. Yet, while their benefits are well-documented, understanding the nuanced pros and cons of steroid injections is essential for patients and clinicians alike to make informed decisions tailored to individual needs.
When Inflammation Meets Precision: How Steroid Injections Work Wonders
Orthopedic steroid injections function by delivering corticosteroids directly into the affected site, effectively damping the immune response that causes swelling and pain. This localized approach means patients often experience quicker pain relief compared to systemic medications. For instance, a middle-aged patient suffering from rotator cuff bursitis might find significant improvement within days after an injection, enabling earlier rehabilitation and functional recovery.
Balancing Relief and Risks: The Delicate Pros and Cons of Steroid Use
Pros: Steroid injections can provide rapid, targeted relief, reduce the need for oral pain medications, and improve quality of life by facilitating physical therapy participation. They are minimally invasive and can be repeated cautiously to manage chronic conditions.
Cons: However, repeated injections carry risks such as tissue weakening, potential joint cartilage damage, and systemic side effects like elevated blood sugar levels. Moreover, injections are not a cure but a component of comprehensive orthopedic care, requiring judicious use.
Can Steroid Injections Cause Long-Term Damage to Joints?
This common concern merits expert attention. While occasional injections are generally safe, studies indicate that frequent steroid use may accelerate cartilage degeneration or tendon weakening, especially if administered improperly or too frequently. Orthopedic specialists recommend spacing injections adequately and combining them with rehabilitative strategies to mitigate these risks. For example, integrating physical therapy post-injection can optimize outcomes and protect joint health.
Practical Wisdom: Case Scenario Illuminating Steroid Injection Decision-Making
Consider a patient with knee osteoarthritis experiencing flare-ups despite conservative measures. A well-timed steroid injection can quell inflammation and enable engagement in strengthening exercises. Yet, the orthopedic team carefully monitors injection frequency and evaluates alternative treatments like non-surgical care options to ensure balanced management.
Empowering Your Orthopedic Journey: When and How to Seek Expert Guidance
Deciding on steroid injections involves weighing immediate symptom relief against potential long-term effects. Patients are encouraged to discuss their full medical history and treatment goals with an orthopedic specialist. For residents seeking trusted expert care, exploring resources such as how to choose the right orthopedic surgeon can be invaluable.
For further nuanced insights on pain management techniques complementing injections, explore our detailed guide on trigger point injection techniques.
Curious about how steroid injections could fit into your personalized orthopedic care plan? Share your questions and experiences in the comments below to connect with our community of experts and patients.
For authoritative clinical perspectives on corticosteroid injections in musculoskeletal disorders, the American Academy of Orthopaedic Surgeons provides comprehensive guidelines and evidence-based recommendations, accessible at aaos.org.
Integrating Steroid Injections Into a Holistic Orthopedic Treatment Plan
Reflecting on my own journey with orthopedic care, I’ve found that steroid injections are most effective when they’re part of a broader, personalized approach. For example, after receiving a corticosteroid injection for tennis elbow, I noticed the relief was temporary unless complemented by targeted physical therapy. This combination helped rebuild strength and prevent recurrence. This experience underscores how steroid injections act as a bridge — offering a window of opportunity to engage more actively in rehabilitation exercises and lifestyle adjustments.
It’s important to remember that orthopedic care isn’t just about treating symptoms but also addressing underlying causes. Learning from trusted sources like the non-surgical care options for herniated discs has expanded my understanding of how conservative treatments can reduce dependency on injections and surgery.
Listening to Your Body: Signs When Steroid Injections May or May Not Be Right
One aspect that often surprises patients is how vital self-awareness is in managing orthopedic conditions. Early in my treatment, I wondered if every flare-up warranted an injection. Over time, I realized that minor discomfort sometimes signals the need for rest or modification of activity rather than immediate intervention. Conversely, persistent or worsening pain may indicate that a well-timed steroid injection could jumpstart healing and improve function.
Consulting with an orthopedic specialist can provide clarity. They help differentiate between pain that benefits from injections and pain better managed by other methods. Exploring resources like choosing the right orthopedic surgeon helped me find a provider whose approach aligned with my goals and values.
How Do You Know When It’s Time to Consider a Steroid Injection?
This question often comes up in conversations with fellow patients and readers. My personal takeaway is that steroid injections are best viewed as a tool—effective but not a panacea. If inflammation severely limits daily activities or physical therapy progress, an injection might be beneficial. However, it’s crucial to weigh this against potential risks and to avoid overuse.
According to recent clinical guidance from the American Academy of Orthopaedic Surgeons, steroid injections should be carefully timed and combined with rehabilitative care to maximize benefits and minimize adverse effects (aaos.org).
The Role of Patient Education and Communication in Orthopedic Care
Being proactive in understanding your treatment options empowers you to partner effectively with your healthcare team. When I first faced the decision about steroid injections, having open discussions about my lifestyle, pain levels, and treatment preferences made a significant difference. It’s also helped me appreciate the importance of follow-up care and adherence to rehabilitation protocols.
For anyone navigating similar decisions, I encourage you to share your experiences or questions in the comments below. Engaging with a community who understands the ups and downs of orthopedic challenges can provide support and practical insights. If you’re interested in exploring complementary therapies, check out our article on trigger point injection techniques for effective pain management.
Maximizing Therapeutic Efficacy: Precision Timing and Dosage Strategies for Steroid Injections
Optimizing the benefits of orthopedic steroid injections hinges on understanding the intricate balance of timing, dosage, and patient-specific factors. Emerging research emphasizes that the pharmacokinetics of corticosteroids vary depending on the agent used, injection site, and the inflammatory milieu. For instance, triamcinolone acetonide, a commonly used corticosteroid, exhibits a prolonged local effect but requires careful dose titration to avoid tissue atrophy. Moreover, current expert consensus advocates for spacing injections at least 3 to 4 months apart, mitigating risks of cartilage degradation and systemic side effects while sustaining anti-inflammatory benefits.
Individualized injection intervals should consider disease severity, comorbidities like diabetes mellitus, and concomitant therapies. For example, in patients with diabetes, steroid injections may transiently elevate blood glucose; thus, endocrinological coordination is vital to adjust antidiabetic regimens during the post-injection window.
Integrative Approaches: Combining Steroid Injections with Regenerative Orthopedic Modalities
Beyond conventional corticosteroids, the frontier of orthopedic care is rapidly evolving with integrative treatments that synergize with steroid injections to enhance healing. Platelet-rich plasma (PRP) and stem cell therapies have garnered attention for their regenerative potential. When judiciously combined, steroid injections can reduce acute inflammation and pain, creating an optimal environment for regenerative therapies to facilitate tissue repair.
Clinical protocols increasingly explore sequential administration, where corticosteroid injections precede PRP by a predefined interval to leverage anti-inflammatory effects without compromising the bioactivity of regenerative agents. This nuanced approach requires sophisticated understanding to avoid antagonistic interactions and maximize patient outcomes.
What Are the Latest Evidence-Based Guidelines on Combining Steroid Injections with Regenerative Therapies in Orthopedics?
Recent systematic reviews and meta-analyses highlight that while corticosteroid injections provide rapid symptom relief, their anti-inflammatory action may transiently suppress cellular proliferation necessary for regeneration. Therefore, leading orthopedic societies, including the American Academy of Orthopaedic Surgeons (aaos.org), recommend a tailored interval—often 2 to 4 weeks—between corticosteroid and biological injections. This interval balances inflammation control with regenerative capacity. However, ongoing clinical trials continue to refine these protocols, underscoring the importance of personalized treatment planning and close monitoring.
Furthermore, patient education about the rationale and timing of these combined therapies is critical to ensure adherence and set realistic expectations. Orthopedic specialists with expertise in both corticosteroid and regenerative injections are best equipped to navigate these complex decisions.
The Science of Injection Techniques: Ultrasound Guidance Enhancing Precision and Safety
The advent of ultrasound-guided steroid injections represents a paradigm shift in orthopedic interventions, dramatically improving accuracy and minimizing complications. This imaging modality allows real-time visualization of anatomical structures, ensuring precise delivery of corticosteroids into targeted tissues while avoiding neurovascular bundles.
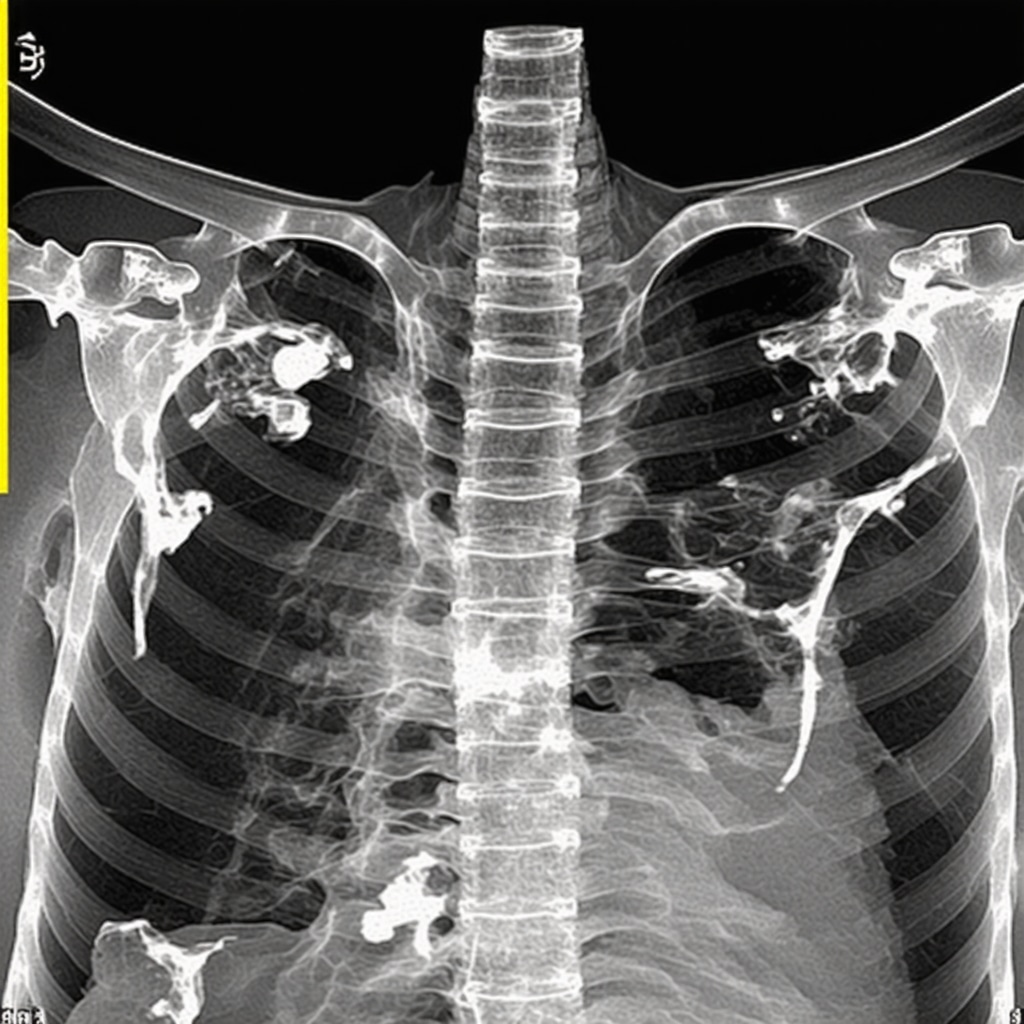
Studies demonstrate that ultrasound guidance not only enhances clinical outcomes by increasing injection efficacy but also reduces the incidence of adverse effects such as inadvertent tendon injections or intravascular administration. For example, in treating adhesive capsulitis of the shoulder, ultrasound-guided injections enable exact placement into the glenohumeral joint capsule, maximizing therapeutic impact.
Integrating ultrasound into routine practice requires specialized training and proficiency. As orthopedic care evolves, mastery of image-guided injection techniques is becoming an indispensable skill for practitioners aiming to deliver state-of-the-art patient care.
Advanced Patient Selection: Biomarkers and Imaging to Predict Steroid Injection Responsiveness
Emerging evidence suggests that pre-injection evaluation using biomarkers and advanced imaging modalities can stratify patients likely to benefit most from steroid injections. For instance, quantitative MRI assessments of cartilage integrity or inflammatory markers in synovial fluid may predict therapeutic responsiveness and risk profiles.
Such precision medicine approaches promise to tailor interventions more effectively, reducing unnecessary injections and optimizing resource utilization. Although these technologies are still under investigation, their integration into clinical practice could revolutionize orthopedic care pathways in the near future.
For orthopedic practitioners and patients eager to delve deeper into these advanced strategies and personalized protocols, I encourage engagement with specialized continuing medical education resources and consultation with multidisciplinary teams specializing in musculoskeletal medicine.
Emerging Frontiers: Leveraging Pharmacogenomics to Personalize Steroid Injection Therapy
Recent advances in pharmacogenomics are unveiling how genetic variations influence individual responses to corticosteroid injections. Polymorphisms in glucocorticoid receptor genes and metabolic enzymes can modulate both efficacy and risk profiles, prompting a paradigm shift toward truly personalized orthopedic interventions. By integrating genetic screening into pre-injection assessments, clinicians can optimize corticosteroid selection and dosing, minimizing adverse effects while maximizing therapeutic gains.
Synergistic Pain Modulation: Combining Steroid Injections with Neuromodulatory Techniques
Beyond conventional anti-inflammatory effects, steroid injections can be strategically paired with neuromodulation modalities such as peripheral nerve stimulation (PNS) or transcutaneous electrical nerve stimulation (TENS) to enhance analgesic outcomes. This multimodal approach targets both inflammatory and neurogenic pain pathways, offering patients superior symptom control especially in complex chronic pain syndromes. Clinical protocols increasingly incorporate timing and sequencing of these interventions to harness their complementary mechanisms.
How Can Advanced Imaging Biomarkers Guide Tailored Injection Protocols for Complex Joint Pathologies?
High-resolution imaging technologies, including quantitative MRI and PET scans, now enable visualization of inflammatory activity and tissue degeneration at a molecular level. These biomarkers facilitate stratification of patients by disease stage and inflammatory burden, allowing clinicians to tailor corticosteroid dosage and injection frequency accordingly. Furthermore, dynamic contrast-enhanced imaging can monitor treatment response in real time, refining therapeutic strategies for refractory cases. This approach exemplifies precision medicine’s role in optimizing orthopedic injection therapy.
Authoritative Insights: Navigating Updated Clinical Guidelines from the American College of Rheumatology
According to the American College of Rheumatology’s latest position statement, optimal use of steroid injections requires a nuanced balance between symptom management and long-term joint preservation. Their evidence-based recommendations emphasize individualized treatment plans incorporating risk stratification, monitoring protocols, and integration with disease-modifying therapies. The guidelines also advocate for interdisciplinary collaboration among rheumatologists, orthopedic surgeons, and rehabilitation specialists to ensure comprehensive patient-centered care (rheumatology.org).
Advanced Safety Protocols: Monitoring and Mitigating Systemic Effects Post-Injection
Given the systemic absorption potential of corticosteroids, especially in patients with comorbidities such as diabetes or cardiovascular disease, vigilant post-injection monitoring is paramount. Emerging protocols recommend serial assessments of blood glucose, blood pressure, and adrenal function within critical windows following administration. Additionally, prophylactic strategies including pre-injection counseling and tailored pharmacologic adjustments mitigate adverse systemic sequelae, thereby enhancing patient safety without compromising efficacy.
Invitation to Engage: Elevate Your Orthopedic Care with Expert-Guided Steroid Injection Strategies
Harness these advanced insights to refine your understanding and management of corticosteroid injections within orthopedic practice. Whether you are a patient navigating complex treatment decisions or a clinician seeking cutting-edge protocols, collaboration and knowledge exchange are invaluable. Share your experiences, pose challenging questions, or explore personalized approaches with our expert community below. Together, we can advance orthopedic care to new heights.
Frequently Asked Questions (FAQ)
What conditions are most effectively treated with orthopedic steroid injections?
Orthopedic steroid injections are primarily used to manage inflammatory conditions such as osteoarthritis, rheumatoid arthritis, bursitis, tendonitis, and adhesive capsulitis. They provide targeted anti-inflammatory effects that reduce pain and swelling in joints and soft tissues, facilitating improved mobility and function.
How often can steroid injections be safely administered without risking joint damage?
Clinical guidelines typically recommend spacing steroid injections at least 3 to 4 months apart to minimize risks like cartilage degradation and tissue weakening. The exact frequency depends on individual patient factors including disease severity, comorbidities, and response to treatment. Overuse can accelerate joint damage, so judicious timing combined with rehabilitative care is essential.
Are there specific risks for diabetic patients receiving steroid injections?
Yes. Corticosteroids can transiently elevate blood glucose levels, which may complicate diabetes management. Diabetic patients require close monitoring of blood sugar following injections and may need adjustments to their medication regimen. Coordination with endocrinologists is advisable to ensure safe and effective treatment.
How do ultrasound-guided injections improve outcomes compared to blind injections?
Ultrasound guidance enhances precision by allowing real-time visualization of anatomical structures, ensuring accurate corticosteroid delivery to the targeted site while avoiding nearby nerves and vessels. This improves therapeutic efficacy and reduces complications such as inadvertent tendon injury or intravascular injection.
Can steroid injections be combined with regenerative therapies like PRP or stem cells?
Yes, but timing is critical. Steroid injections reduce inflammation but may transiently suppress cellular proliferation needed for regeneration. Current evidence suggests waiting 2 to 4 weeks after a corticosteroid injection before administering regenerative therapies to maximize healing potential. Personalized protocols guided by specialists optimize this combination.
What role do biomarkers and imaging play in selecting patients for steroid injections?
Emerging research shows that advanced imaging (e.g., quantitative MRI) and inflammatory biomarkers can predict which patients are most likely to benefit from steroid injections. These tools aid in personalized treatment planning by identifying disease severity, inflammation extent, and risk of adverse effects, thus improving outcomes and resource utilization.
How can pharmacogenomics influence corticosteroid injection therapy?
Pharmacogenomics studies genetic variations that affect individual responses to corticosteroids, impacting both efficacy and side effect profiles. Integrating genetic screening could guide personalized corticosteroid choice and dosing, minimizing risks and enhancing therapeutic benefits in orthopedic care.
What systemic side effects should patients be aware of after steroid injections?
Though injections are localized, some systemic absorption occurs. Potential side effects include transient elevation of blood sugar, increased blood pressure, adrenal suppression, and mood changes. Patients with comorbidities require close monitoring and tailored management strategies to mitigate these risks.
How important is patient education and communication in managing steroid injection therapy?
Patient education is vital to set realistic expectations, ensure adherence to rehabilitation, and encourage proactive symptom monitoring. Open communication with orthopedic specialists fosters shared decision-making, balancing benefits with risks and integrating injections into comprehensive treatment plans.
When should a patient consider steroid injections as part of their orthopedic treatment?
Steroid injections are appropriate when inflammation significantly limits function or impedes rehabilitation progress despite conservative measures. They serve as a therapeutic bridge to facilitate physical therapy and symptom control but are not standalone cures. Decisions should be individualized based on clinical assessment and patient preferences.
Trusted External Sources
- American Academy of Orthopaedic Surgeons (AAOS) – aaos.org: Provides comprehensive, evidence-based clinical guidelines on corticosteroid injections, orthopedic best practices, and patient education resources.
- American College of Rheumatology (ACR) – rheumatology.org: Offers updated position statements and consensus guidelines on inflammatory joint diseases and the judicious use of steroid injections in rheumatologic care.
- Journal of Orthopaedic Research: A peer-reviewed journal publishing cutting-edge studies on orthopedic therapies, including pharmacokinetics, injection techniques, and integrative regenerative approaches.
- Arthritis & Rheumatology Journal: Features high-impact research on musculoskeletal inflammation, biomarkers, and personalized medicine strategies relevant to corticosteroid therapy.
- National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) – niams.nih.gov: An authoritative source for patient-centered information and research updates on orthopedic conditions and treatment modalities.
Conclusion
Orthopedic steroid injections represent a powerful, targeted intervention to alleviate inflammation and pain, enabling patients to regain function and engage more effectively in rehabilitation. Their efficacy hinges on precise timing, dosing, and integration with complementary therapies such as physical therapy and emerging regenerative modalities. Advances in imaging, pharmacogenomics, and biomarker profiling are revolutionizing patient selection and personalized treatment protocols, minimizing risks while maximizing therapeutic outcomes.
Ultimately, successful use of corticosteroid injections demands a collaborative approach involving informed patients and experienced specialists, guided by up-to-date clinical evidence and individualized care plans. By embracing these expert insights and combining them with holistic orthopedic management, patients can optimize recovery and quality of life.
We invite you to share your experiences, ask questions, and explore further expert content to deepen your understanding of steroid injections in orthopedic care. Together, we can advance treatment strategies and support informed decisions for healthier joints and better mobility.


This article does a great job laying out the trade-offs between quick symptom control and long-term joint health. I wanted to share a brief experience that echoed many of the points here: I received a steroid injection for knee osteoarthritis last year and noticed meaningful pain relief within a week, which finally let me participate in targeted physical therapy. That combination — injection plus PT — seemed to be the real game-changer for me rather than repeated injections alone.
A few practical takeaways: my specialist used ultrasound guidance, which felt reassuring because the placement was precise; and I’m diabetic, so my endocrinologist and I tracked blood glucose closely for a few days afterwards (I saw a transient spike that normalized with minor med adjustments). I’m not a clinician, but I found coordination between teams important.
Has anyone else combined a steroid injection with PRP or waited a specific interval before regenerative therapy? For readers with diabetes, what monitoring or med tweaks did your team recommend post-injection?
This article provides a comprehensive overview of the role steroid injections play in orthopedic care, which is helpful given how nuanced their use can be. I’ve personally seen how targeted injections can provide rapid relief, especially in cases like rotator cuff tendinitis, allowing patients to advance with physical therapy more comfortably. However, I think it’s important to emphasize that the timing and frequency of these injections are critical—overuse can indeed risk joint cartilage damage, as mentioned.
In my experience, combining injections with structural rehabilitation yields the best outcomes. Has anyone utilized advanced imaging techniques, like MRI biomarkers, to help decide the optimal timing for injections or assess responsiveness? Also, in the case of patients with diabetes, how have practitioners balanced the potential transient hyperglycemia after steroid treatments? Sharing these practical strategies can help patients and clinicians optimize benefits while minimizing risks.