My Personal Experience with Nerve Compression and the Search for Effective Treatment
Hi everyone! I want to share a story close to my heart — my journey through nerve compression pain and the different orthopedic treatment options I explored. It all started during a busy week when I suddenly felt a sharp tingling sensation radiating down my leg. At first, I dismissed it as a minor strain, but as days passed, the discomfort grew worse, affecting my daily life. After consulting with an orthopedic specialist, I learned that nerve compression could be a culprit, and my journey towards relief began.
Understanding Nerve Compression and Its Impact
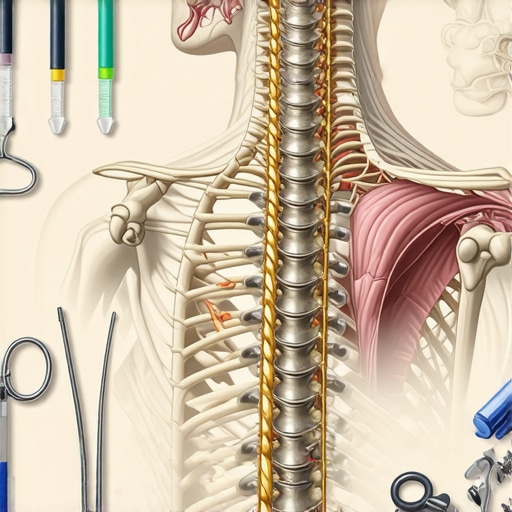
Nerve compression occurs when surrounding tissues, such as bones, muscles, or ligaments, put pressure on a nerve, leading to pain, numbness, or weakness. I found it fascinating how interconnected our musculoskeletal system is, and how even minor misalignments can cause significant discomfort. According to the American Association of Neurological Surgeons, proper diagnosis is crucial for choosing effective treatment.
My Exploration of Non-Surgical and Surgical Options
Initially, I was hesitant about surgery, so I explored non-invasive treatments like physical therapy and epidural injections. These approaches, especially physical therapy, helped me strengthen supporting muscles and improve flexibility. I also read about minimally invasive procedures, like laser spine surgery, which can be effective for certain cases. A reputable source, NJ Orthopedic, details how such treatments can reduce recovery time and risks.
What Are Your Options for Nerve Compression? A Personal Reflection
Looking back, I realize that understanding the full spectrum of treatment options is vital. From conservative care to advanced surgical interventions, each has its place depending on the severity of compression. For my case, a combination of physical therapy and guided injections proved effective. However, if symptoms persist, consulting a spine specialist for possible surgical options, like lumbar fusion or decompression, might be necessary. I encourage everyone to seek personalized advice from trusted orthopedic professionals. Want to learn more about selecting the right specialist? Check out this guide.
How Do I Know When It’s Time to Consider Surgery?
Deciding between continued conservative care or surgery can be daunting. I found that persistent pain, weakness, or loss of function are signals that it might be time to explore surgical options. Discussing these symptoms with your orthopedic surgeon can provide clarity. Remember, each case is unique, and a tailored plan is best. For further insights, I recommend visiting this resource.
If you’re experiencing nerve compression symptoms, don’t hesitate to reach out. I invite you to share your experiences or ask questions in the comments — we’re all in this journey together! For personalized care, consider contacting a local orthopedic specialist through this contact page.
Exploring Cutting-Edge Solutions for Nerve Compression: An Expert’s Perspective
Nerve compression is a complex condition that demands a nuanced understanding of both its underlying causes and the latest treatment innovations. As an orthopedic specialist deeply engaged in this field, I often encounter patients asking about the most effective options beyond conventional therapies. The evolution of minimally invasive procedures and personalized treatment plans continues to transform patient outcomes, making it essential to stay informed about emerging solutions.
How Do Innovative Orthopedic Interventions Enhance Patient Outcomes?
Recent advancements in orthopedic care have introduced a variety of less invasive yet highly effective treatments. For instance, minimally invasive spine procedures such as endoscopic decompression or laser disc surgery can significantly reduce recovery times and associated risks. These techniques utilize smaller incisions, which means less tissue damage and quicker return to daily activities. When considering options, it’s vital to evaluate the specific nature of nerve compression, such as whether it stems from herniated discs, spinal stenosis, or other structural abnormalities.
What Factors Influence the Choice Between Non-Surgical and Surgical Treatments?
Choosing the appropriate intervention hinges on multiple factors: severity of symptoms, duration of nerve compression, patient health status, and response to initial therapies. Non-surgical approaches, including physical therapy, epidural injections, or nerve blocks, often serve as first-line treatments. However, persistent symptoms or progressive neurological deficits may necessitate surgical intervention. Advanced procedures like lumbar fusion or microdecompression can provide definitive relief, especially in cases where conservative methods fail. For more personalized guidance, consult with a specialist experienced in spinal surgery selection.
Are There Risks or Limitations to These Advanced Treatments?
While minimally invasive techniques offer substantial benefits, they are not without limitations. Factors such as the precise location of nerve impingement, the presence of spinal instability, or previous surgeries can influence outcomes. It’s important to recognize that no procedure guarantees complete symptom resolution. Potential risks include nerve injury, infection, or incomplete decompression, which underscores the importance of thorough preoperative assessment and surgeon expertise. For a detailed discussion on the risks and benefits, review laser spine surgery considerations.
What Are the Practical Steps to Ensure You Receive the Best Care?
To optimize your treatment journey, start with a comprehensive evaluation by a qualified orthopedic specialist. Ask about the latest minimally invasive options, their success rates, and how they compare to traditional surgery. Ensure your surgeon has extensive experience with the specific procedure recommended. Additionally, consider seeking a second opinion if your case is complex or if you’re unsure about the proposed treatment plan. Deepening your understanding of your condition and available options empowers you to make informed decisions and advocate effectively for your health.
If you’re navigating treatment options for nerve compression, I encourage you to share your questions or experiences in the comments. For tailored advice and to explore the best options suited to your needs, contact a trusted orthopedic professional through this contact page.
Unraveling the Intricacies of Nerve Compression: Personal Wisdom and Cutting-Edge Advances
As I continue to navigate the complex landscape of nerve compression, I realize that each patient’s journey is uniquely nuanced, shaped by individual anatomy, lifestyle, and response to treatments. This understanding has deepened my appreciation for personalized care—something I emphasize when consulting with patients. For example, I often see how a slight variation in spinal structure can influence whether conservative therapies suffice or if surgical intervention becomes necessary. The importance of a comprehensive assessment cannot be overstated, especially considering emerging diagnostic tools like advanced MRI techniques that offer unparalleled clarity in visualizing nerve impingements.
What Are the Hidden Factors That Influence Surgical Outcomes?
Delving into my experience, I’ve observed that factors such as spinal stability, patient age, and comorbidities play crucial roles in surgical success. Recent studies, such as those published in the Spine Journal, highlight how preoperative planning that accounts for these variables significantly enhances recovery rates. Understanding these nuances has helped me guide patients more effectively, combining evidence-based practices with individual circumstances.
Moreover, technological innovations like intraoperative neuromonitoring have increased safety margins during decompression procedures. This technology, coupled with minimally invasive techniques, offers promising prospects for high-risk patients who previously faced substantial surgical risks. I encourage fellow practitioners to stay abreast of these developments, as they continually redefine what is possible in nerve compression treatment.
Reflecting on My Personal Path and the Broader Implications for Patients
My journey has reinforced the importance of patient education—empowering individuals to understand their condition beyond the standard explanations. Sharing my own experiences of trial, error, and eventual relief has fostered trust and patience among my patients. I often emphasize that navigating nerve compression is not merely about choosing a procedure but about understanding the interplay of anatomy, pathology, and lifestyle factors that influence outcomes.
If you’re contemplating your options, I recommend exploring comprehensive resources like non-surgical care strategies or consulting specialized spine centers to tailor interventions specifically for your case. Remember, the journey toward relief is often a collaborative effort, blending cutting-edge science with personalized care plans.
How Can Patients Advocate for Themselves in an Evolving Treatment Landscape?
Empowerment begins with knowledge. Staying informed about the latest minimally invasive procedures, understanding potential risks, and asking targeted questions during consultations can significantly influence treatment success. For instance, knowing that techniques like endoscopic decompression have improved outcomes for certain patients can help you advocate for options aligned with your health goals. I also recommend seeking second opinions when unsure, as this can uncover alternative approaches and instill confidence in your decisions.
In the end, embracing both the scientific advancements and the personalized nuances of nerve compression treatment allows us to forge a path toward better health and restored function. I invite you to share your experiences or ask questions—every story adds to our collective understanding. For tailored guidance, don’t hesitate to contact a trusted orthopedic specialist through this contact page.
Unveiling Hidden Factors That Influence Surgical Success in Nerve Compression Cases
Throughout my clinical journey, I’ve observed that patient-specific variables such as spinal biomechanics, age-related degenerative changes, and comorbidities like diabetes or osteoporosis significantly impact surgical outcomes. Recent research published in the Spine Journal emphasizes that meticulous preoperative planning, including advanced imaging techniques like functional MRI, enhances the precision of decompression procedures. These insights underscore the necessity of a tailored approach, recognizing that a one-size-fits-all strategy rarely suffices in complex nerve compression cases.
The Role of Cutting-Edge Intraoperative Technologies in Elevating Patient Safety
Technologies such as intraoperative neuromonitoring and 3D navigation systems have revolutionized the surgical landscape. These tools enable real-time feedback on nerve integrity, significantly reducing the risk of iatrogenic injury. My experience with intraoperative neuromonitoring has demonstrated its value, especially in high-risk patients with multilevel degenerative disease. Embracing these innovations not only enhances safety but also improves the likelihood of achieving durable symptom relief, which is critical in complex cases where standard decompression might be insufficient.
How Can Patients Advocate Effectively for Advanced, Personalized Care?
Empowerment through knowledge is vital. Patients should inquire about the surgeon’s experience with minimally invasive and technologically advanced procedures. Asking specific questions about the use of intraoperative monitoring, image-guided navigation, and preoperative planning can reveal the depth of a surgeon’s expertise. Additionally, seeking multiple opinions from top-rated specialists, such as those listed in this trusted resource, ensures that treatment plans are comprehensive and personalized. Remember, advocating for yourself involves understanding that the latest innovations can be pivotal in achieving optimal outcomes.
Integrating Biomechanical and Lifestyle Factors for Long-Term Spinal Health
Beyond immediate surgical considerations, I’ve come to appreciate the importance of addressing biomechanical imbalances and lifestyle factors that influence nerve compression recurrence. For instance, ergonomic modifications, targeted strengthening exercises, and weight management play crucial roles in sustaining surgical benefits. A recent study highlights how comprehensive post-operative rehabilitation, including tailored physical therapy, can drastically reduce the risk of re-herniation or stenosis. For guidance on optimizing your recovery, I recommend exploring these rehab strategies.
What Are the Latest Advances in Minimally Invasive Nerve Decompression Techniques?
Innovations like endoscopic decompression and laser-assisted procedures continue to evolve, offering less invasive options with quicker recovery times. These techniques utilize smaller incisions and often preserve more of the natural anatomy, reducing postoperative pain and hospital stays. Evidence from recent clinical trials indicates that, when appropriately indicated, these procedures can match the efficacy of traditional open surgeries while minimizing drawbacks. As an orthopedic specialist committed to cutting-edge care, I urge patients to discuss the suitability of these options with their surgeons, especially at centers recognized for their expertise in minimally invasive spine surgery.
Understanding Insurance and Access Challenges in Advanced Orthopedic Treatments
While technological progress broadens treatment possibilities, insurance coverage remains a significant hurdle. Navigating prior authorizations and understanding policy limitations require proactive engagement. I advise patients to consult resources like this guide to better advocate for coverage of innovative procedures. Securing comprehensive preoperative documentation and demonstrating the potential for improved quality of life often facilitate approvals, ensuring that patients access the most suitable, advanced treatments available.
In my experience, a combination of technological innovation, personalized care strategies, and proactive patient advocacy forms the cornerstone of successful nerve compression management. If you’re eager to delve deeper into these topics or share your personal journey, I encourage you to engage with this community and reach out through this contact page. Together, we can navigate the complexities of modern orthopedic care to achieve the best possible outcomes.
Things I Wish I Knew Earlier (or You Might Find Surprising)
The Hidden Power of Early Diagnosis
One thing I learned through my journey is that catching nerve compression early can make a world of difference. I used to dismiss that tingling sensation as just a minor nuisance, but waiting too long often led to more complex treatments. Trusting your body and seeking professional advice sooner rather than later can prevent unnecessary complications.
The Myth of One-Size-Fits-All Treatments
Initially, I thought that surgery was the only definitive solution. However, I discovered that personalized approaches, combining physical therapy, minimally invasive procedures, and lifestyle changes, often yield better long-term results. This realization encouraged me to explore all options and consult specialists who tailor treatments to individual needs.
How Lifestyle Factors Influence Recovery
Small adjustments like ergonomic workspace setups and regular stretching can significantly impact nerve health. I noticed that integrating these habits into my daily routine not only helped in recovery but also prevented future issues. It’s a reminder that our daily choices play a crucial role in spinal health.
The Importance of a Trustworthy Medical Team
Finding a compassionate and experienced orthopedic specialist was a turning point for me. A knowledgeable surgeon who listens and explains thoroughly can guide you through complex decisions and set realistic expectations. I recommend researching and seeking second opinions to ensure you’re in good hands.
The Role of Cutting-Edge Technologies
Advancements like intraoperative neuromonitoring and minimally invasive techniques are revolutionizing nerve compression treatments. These innovations reduce risks and recovery times, making surgical options more accessible and appealing. Staying informed about these options can empower patients to advocate for the best care possible.
Resources I’ve Come to Trust Over Time
- American Association of Neurological Surgeons: Their comprehensive guides and research articles helped me understand the medical aspects of nerve compression. I recommend it for anyone seeking credible, peer-reviewed information.
- NJ Orthopedic: Their detailed explanations of minimally invasive spine procedures gave me confidence in exploring advanced treatment options. It’s a reliable resource for patients considering surgery.
- Spine Journal: For those interested in the latest research, this journal offers in-depth studies on surgical outcomes and innovations. It broadened my understanding of what’s possible in modern orthopedic care.
Parting Thoughts from My Perspective
Reflecting on my experience with nerve compression, I realize that awareness, personalized care, and embracing technological advancements are key to effective treatment. If you’re experiencing symptoms, don’t hesitate to seek professional guidance. Every journey is unique, but with the right information and support, relief is possible. If this resonated with you, I’d love to hear your thoughts or experiences. Share it with someone who might find it helpful, and remember to advocate for yourself in this evolving landscape of orthopedic care.