Unlocking the Complexities of Whiplash: An Orthopedic Perspective
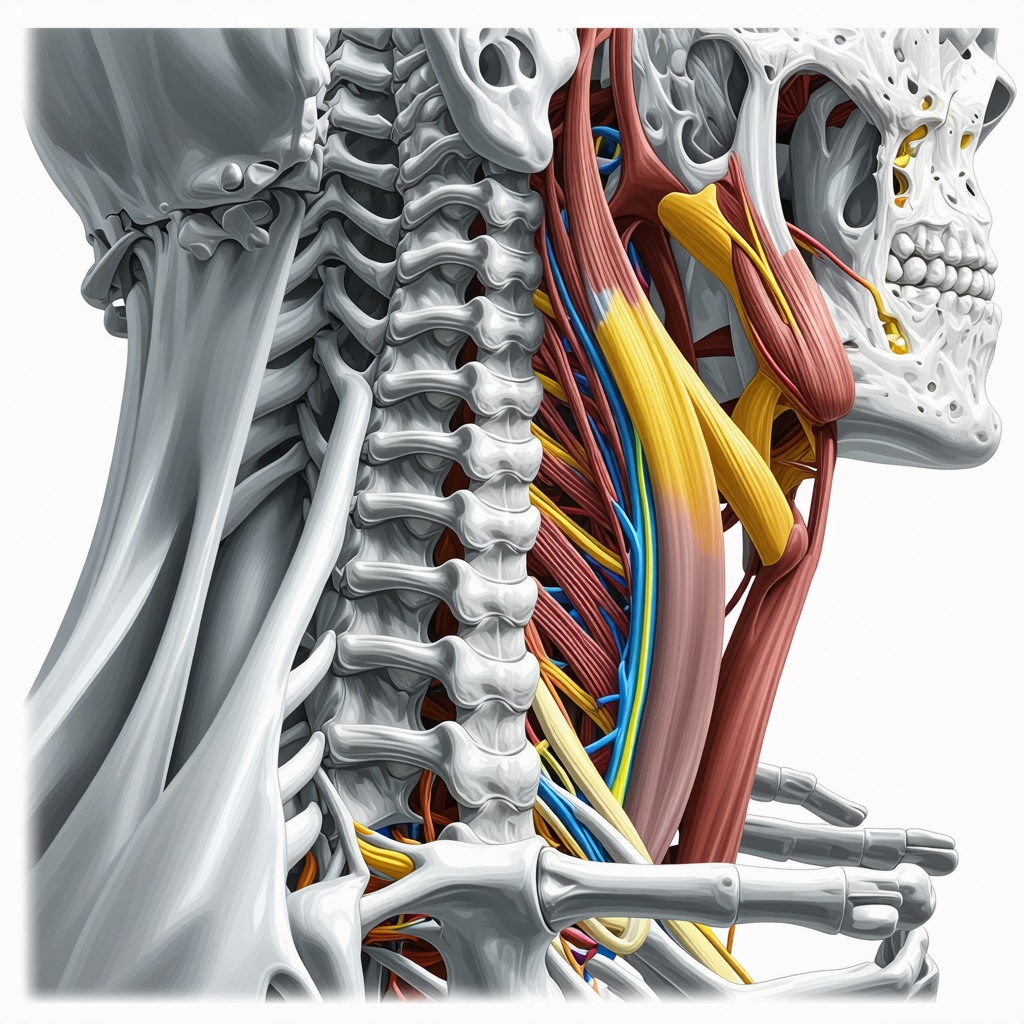
Whiplash injuries, often resulting from sudden acceleration-deceleration forces like car accidents, represent a multifaceted challenge in orthopedic medicine. Beyond the immediate neck pain, these injuries can disrupt soft tissues, cervical spine alignment, and nerve function, demanding a nuanced, expert-driven treatment approach. Understanding effective orthopedic treatment for whiplash injuries is crucial not only for symptom relief but also for preventing chronic complications.
Tailoring Orthopedic Strategies to Whiplash’s Hidden Layers
Orthopedic treatment for whiplash transcends simple pain management; it encompasses restoring biomechanical integrity and facilitating tissue healing. Early intervention often involves immobilization with cervical collars to reduce movement-induced exacerbation, complemented by targeted anti-inflammatory medications. However, the cornerstone of recovery lies in controlled, progressive physical therapy that addresses muscle stiffness, joint mobility, and proprioception deficits.
Advanced therapeutic modalities include manual therapy techniques and specialized orthopedic exercises designed to recalibrate cervical musculature and improve neuromuscular coordination. For more detailed rehabilitation techniques, explore essential orthopedic physical therapy techniques for faster recovery.
How do orthopedic specialists determine the best treatment plan for whiplash injuries?
Orthopedic specialists begin with comprehensive clinical assessments that integrate patient history, symptomatology, and diagnostic imaging such as MRI or X-rays to evaluate soft tissue damage and cervical spine alignment. This evaluation is critical because whiplash symptoms may mask underlying issues like disc herniations or nerve compression. The treatment plan is then individualized—balancing conservative care with advanced interventions as needed. For instance, if nerve involvement is detected, options like orthopedic injections might be considered to provide targeted pain relief and reduce inflammation, as discussed in orthopedic injections for back pain effective relief options.
Integrating Evidence-Based Practices and Patient Experience
Orthopedic care for whiplash injuries is continually refined through clinical research and patient feedback. Studies published in journals like The Journal of Orthopaedic & Sports Physical Therapy emphasize multimodal approaches combining manual therapy, exercise, and patient education to optimize outcomes. Moreover, patient adherence to rehabilitation protocols profoundly influences recovery trajectories, highlighting the role of tailored communication and support.
Exploring Cutting-Edge Orthopedic Innovations in Whiplash Care
Emerging technologies such as biomechanical analysis tools and regenerative medicine techniques are beginning to shape whiplash treatment paradigms. For example, platelet-rich plasma (PRP) injections are investigated for their potential to accelerate soft tissue healing. While not yet standard, these innovations reflect the orthopedic field’s commitment to evolving evidence-based, patient-centered care.
For those interested in comprehensive orthopedic management after injuries, resources like auto accident orthopedic doctor tailored treatment plans provide valuable insights.
Engage with us: If you’ve experienced whiplash or are exploring treatment options, share your questions or experiences in the comments below. Your story could help others navigate their recovery journey.
For further reading on the science behind whiplash and orthopedic interventions, the National Center for Biotechnology Information (NCBI) provides an authoritative and in-depth resource.
Reflecting on the Emotional Journey of Whiplash Recovery
When I first experienced whiplash, the physical pain was matched by a surprising emotional toll. It’s not just about the neck stiffness or headaches but the uncertainty of when, or if, full recovery will come. I found that acknowledging this emotional aspect was as important as the physical rehabilitation. Sharing this with my orthopedic specialist helped us tailor a treatment plan that included not only physical therapy but also coping strategies to manage stress related to chronic pain.
Personalizing Treatment: Why One Size Doesn’t Fit All
Everyone’s body responds differently to injuries like whiplash. In my case, the initial use of a cervical collar was helpful to limit movement and reduce inflammation, but prolonged immobilization risked muscle weakening. My orthopedic team emphasized a gradual transition to active therapy, including exercises to rebuild strength and improve flexibility. This balance was crucial and highlights why consulting with a specialist who understands these nuances can make all the difference. If you’re curious about how physical therapy can be optimized post-whiplash, check out essential orthopedic physical therapy techniques for faster recovery.
What role does patient feedback play in refining orthopedic care?
From my experience and supported by research from the National Center for Biotechnology Information (NCBI), patient feedback is invaluable. It informs orthopedic specialists about what’s working and what needs adjustment. For instance, I communicated when certain exercises caused discomfort, allowing my therapist to modify the regimen. This two-way communication ensured that my treatment was both effective and tolerable, ultimately speeding up recovery.
Exploring Non-Surgical Options and When to Seek More Intensive Care
While many whiplash cases resolve with conservative care, there are times when more advanced interventions are necessary. In my journey, persistent nerve pain required consideration of orthopedic injections to reduce inflammation and manage pain effectively. Learning about these options gave me peace of mind that surgery was not the only path. For those interested, orthopedic injections for back pain effective relief options provide a great overview of these treatments.
Moreover, recognizing when to escalate care to a spine surgeon is crucial. Persistent neurological symptoms or structural damage might require surgical consultation. Resources like when to escalate to a spine surgeon critical warning signs can guide patients in making informed decisions.
How Can We Empower Each Other Through Shared Experiences?
Recovery from whiplash can be isolating, but sharing our stories creates community and offers practical insights. I invite you to share your experiences or questions in the comments below. Perhaps you’ve discovered a particular therapy or lifestyle adjustment that made a difference. Your contribution might be the encouragement someone else needs.
For anyone navigating the complexities of whiplash or related orthopedic injuries, exploring tailored treatment plans like those detailed in auto accident orthopedic doctor tailored treatment plans can be enlightening and reassuring.
Decoding Chronic Whiplash: When Standard Orthopedic Treatments Fall Short
While many whiplash injuries heal with timely and appropriate orthopedic care, a subset of patients experience persistent symptoms that evolve into chronic whiplash-associated disorders (WAD). These cases demand a sophisticated, multifactorial approach beyond initial conservative management. Chronic WAD often involves not only ongoing musculoskeletal pain but also neuropathic components, psychological distress, and altered central pain processing mechanisms. As orthopedic specialists, recognizing the transition from acute to chronic stages is paramount to optimizing intervention strategies.
Advanced diagnostic tools such as high-resolution ultrasound and functional MRI can reveal subtle soft tissue changes and neuroplastic alterations that traditional imaging might miss. Incorporating these insights allows for targeted therapies addressing both peripheral and central contributors to pain and dysfunction.
How can orthopedic care integrate biopsychosocial factors to enhance chronic whiplash recovery?
Modern orthopedic management of chronic whiplash emphasizes a biopsychosocial paradigm, acknowledging that psychological stress, anxiety, and patient beliefs significantly influence outcomes. Interdisciplinary collaboration involving physical therapists, psychologists, and pain specialists fosters comprehensive rehabilitation. Cognitive-behavioral therapy (CBT) integrated with graded physical activity programs has been shown to improve functional capacity and reduce pain catastrophizing, as highlighted in research published by the National Institutes of Health (NIH).
Orthopedic clinicians must also tailor communication to validate the patient’s experience and dispel misconceptions about chronic pain, facilitating adherence and engagement with complex treatment regimens.
Harnessing Regenerative Medicine: The Frontier of Whiplash Treatment Innovation
Regenerative therapies represent a cutting-edge frontier in orthopedic whiplash management, aiming to biologically restore damaged cervical tissues and modulate inflammation. Platelet-rich plasma (PRP) and stem cell injections have garnered increasing interest for their potential to accelerate healing of ligamentous and muscular injuries that traditional modalities cannot fully resolve.
Emerging clinical trials suggest that PRP injections may reduce pain and improve function in chronic soft tissue injuries associated with whiplash, although standardized protocols and long-term efficacy data remain under active investigation. These therapies require meticulous patient selection and should be integrated within a comprehensive rehabilitation framework rather than as standalone solutions.
Precision Orthopedics: Customizing Bracing and Neuromuscular Retraining for Optimal Cervical Stability
Beyond pharmacological and injection-based interventions, advanced orthopedic care increasingly leverages precision bracing coupled with neuromuscular retraining to restore mechanical stability and sensorimotor control disrupted by whiplash. Innovative cervical orthoses now incorporate dynamic support systems that allow graduated movement, minimizing muscle atrophy while protecting healing tissues.
Concurrently, neuromuscular retraining focuses on recalibrating proprioceptive feedback loops and cervical muscle coordination through tailored exercises and biofeedback technologies. These approaches aim to prevent maladaptive movement patterns that contribute to chronic pain and dysfunction. For patients interested in integrating these advanced modalities, consulting with an orthopedic specialist experienced in complex whiplash rehabilitation is essential.
Exploring the Role of Advanced Imaging and Biomarkers in Predicting Whiplash Recovery Trajectories
Recent advances in imaging techniques and biomarker research are transforming prognostication in whiplash injuries. Quantitative MRI metrics assessing muscle fatty infiltration and ligament integrity, alongside inflammatory and neurochemical biomarkers detected in blood or cerebrospinal fluid, hold promise for identifying patients at risk of poor recovery.
Such predictive capability enables early, aggressive interventions tailored to individual risk profiles, potentially mitigating progression to chronicity. Ongoing studies aim to validate these tools for routine clinical implementation, marking a shift towards precision medicine in orthopedic trauma care.
What emerging technologies are revolutionizing diagnosis and treatment personalization in whiplash orthopedic care?
Emerging technologies such as wearable motion sensors and machine learning algorithms are revolutionizing orthopedic whiplash care by providing objective assessments of cervical spine biomechanics and patient-specific response patterns. Wearable devices track fine-grained movement data during daily activities, enabling real-time monitoring and adjustment of rehabilitation protocols.
Machine learning models analyze large datasets integrating clinical, imaging, and biomechanical variables to predict treatment outcomes and optimize individualized plans. This convergence of technology and clinical expertise heralds a new era of personalized, data-driven orthopedic management for whiplash injuries.
Engage With Our Expert Community: Are you interested in how these advanced approaches can be integrated into your whiplash recovery plan? Connect with our specialists for personalized guidance or share your experiences in the comments below to enrich our collective knowledge.
Decoding the Neuromechanical Interface: A New Frontier in Whiplash Rehabilitation
Recent advancements in understanding the neuromechanical interplay after whiplash injury are redefining rehabilitation paradigms. This interface encompasses the dynamic communication between cervical biomechanics and central nervous system adaptations, which can perpetuate pain and motor dysfunction if not properly addressed. Cutting-edge protocols now integrate sensorimotor training that targets both peripheral joint stability and cortical reorganization, aiming to restore coordinated movement patterns disrupted by trauma.
Integrative Orthopedic Approaches: Synergizing Regenerative Therapies with Functional Rehabilitation
Combining regenerative medicine with functional orthopedic rehabilitation offers a synergistic path to recovery. For instance, following biologic interventions such as platelet-rich plasma (PRP) injections, tailored neuromuscular exercises enhance the integration of tissue repair within physiological movement contexts. This dual approach not only accelerates healing but also reduces the risk of re-injury by improving muscular support and proprioceptive acuity.
How can orthopedic clinicians effectively balance regenerative treatments with traditional rehabilitation to maximize whiplash recovery?
Orthopedic specialists must adopt a phased treatment algorithm where regenerative therapies precede or coincide with graduated physical therapy. Timing is critical; initiating active rehabilitation too early may compromise biologic healing, whereas delayed therapy can foster stiffness and neuromuscular deficits. Collaborative care teams utilize biomarkers and imaging to monitor tissue response, adjusting protocols dynamically. Such precision ensures that each patient’s unique healing trajectory guides intervention sequencing, optimizing functional outcomes and minimizing chronicity risks.
Leveraging Artificial Intelligence to Personalize Whiplash Rehabilitation Protocols
Artificial intelligence (AI) is increasingly instrumental in distilling complex clinical and biomechanical datasets into actionable insights. Machine learning algorithms analyze patient-specific variables—including injury biomechanics, imaging findings, and response to therapy—to generate predictive models for recovery trajectories. These models empower clinicians to customize rehabilitation intensity, modality selection, and progression rates, thereby enhancing efficacy and patient adherence.
Exploring the Role of Neuroplasticity in Chronic Whiplash Pain Modulation
Neuroplastic changes following whiplash injury contribute substantially to chronic pain syndromes. Interventions targeting cortical reorganization—such as graded motor imagery and sensorimotor retraining—promote adaptive neural remodeling. This neuroorthopedic approach synergizes with peripheral treatments to address pain at its multifactorial origins, highlighting the necessity for interdisciplinary collaboration.
Engage With Cutting-Edge Orthopedic Expertise and Transform Your Recovery Journey
Embracing these advanced orthopedic methodologies can profoundly influence whiplash outcomes. We invite you to connect with our specialists to explore personalized treatment strategies that integrate regenerative medicine, precision rehabilitation, and AI-driven insights. Share your experiences or questions in the comments below to foster a community dedicated to innovative recovery solutions.
For an authoritative overview of integrating regenerative therapies in musculoskeletal injuries, refer to the National Center for Biotechnology Information (NCBI) article on regenerative medicine in orthopedics.

Frequently Asked Questions (FAQ)
What exactly causes a whiplash injury and which structures are most affected?
Whiplash is caused by a rapid back-and-forth movement of the neck, typically from events like car collisions. This sudden acceleration-deceleration can strain or injure cervical muscles, ligaments, intervertebral discs, and nerve roots. The soft tissues and cervical spine alignment are particularly vulnerable, which can lead to pain, stiffness, and neurological symptoms.
How do orthopedic specialists customize treatment plans for whiplash patients?
Orthopedic specialists perform thorough clinical evaluations including patient history, physical examination, and imaging (MRI, X-rays) to determine injury severity and identify complications such as nerve involvement. Treatment plans are individualized based on these findings, balancing conservative approaches like immobilization and physical therapy with advanced interventions such as orthopedic injections or regenerative techniques when necessary.
Why is early physical therapy important in whiplash recovery?
Early, controlled physical therapy helps restore cervical mobility, reduce muscle stiffness, and retrain neuromuscular coordination. It prevents complications like chronic pain and muscle atrophy. Progressive exercises tailored to the patient’s tolerance promote tissue healing and functional restoration, significantly improving recovery outcomes.
When should a patient consider regenerative medicine options like PRP for whiplash?
Regenerative therapies such as platelet-rich plasma (PRP) injections may be considered in cases where soft tissue injuries persist despite conventional treatment. These options aim to biologically enhance tissue repair and modulate inflammation. However, they are currently adjuncts to comprehensive rehabilitation and require careful patient selection and timing within the treatment course.
What role do biopsychosocial factors play in chronic whiplash-associated disorders?
Chronic whiplash often involves physical pain intertwined with psychological stress, anxiety, and altered central nervous system processing. Addressing these factors through interdisciplinary care—including cognitive-behavioral therapy and patient education—is essential. This holistic approach supports pain modulation, improves adherence, and optimizes long-term functional recovery.
How are emerging technologies like AI and wearable sensors enhancing whiplash treatment?
Wearable motion sensors provide objective data on cervical biomechanics during daily activities, allowing clinicians to monitor progress and modify therapy in real time. Artificial intelligence analyzes complex datasets to predict recovery trajectories and personalize rehabilitation protocols, enhancing treatment precision and patient engagement.
What are the signs that indicate the need to escalate orthopedic care to surgical consultation?
Persistent neurological deficits, severe structural damage evident on imaging, or failure of conservative and minimally invasive treatments to improve symptoms warrant surgical evaluation. Recognizing these warning signs early facilitates timely intervention to prevent further disability.
How can neuromechanical retraining improve outcomes in whiplash rehabilitation?
Neuromechanical retraining targets the sensorimotor system by restoring proprioceptive feedback and coordinated cervical muscle function. This helps correct maladaptive movement patterns and cortical reorganization that contribute to chronic pain and dysfunction, ultimately improving mechanical stability and reducing symptom persistence.
Are cervical collars beneficial throughout the entire whiplash recovery process?
Cervical collars can be useful initially to limit harmful neck movements and reduce inflammation. However, prolonged immobilization may lead to muscle weakness and stiffness. Orthopedic experts recommend transitioning to active therapy as soon as safely possible to promote muscle strength and joint mobility.
How important is patient feedback during whiplash treatment?
Patient feedback is critical for adjusting treatment intensity and modalities to individual tolerance and progress. It ensures therapies are effective and comfortable, helps prevent setbacks, and fosters a collaborative care environment that supports optimal recovery.
Trusted External Sources
- The Journal of Orthopaedic & Sports Physical Therapy (JOSPT): Provides peer-reviewed clinical research on manual therapy, biomechanics, and rehabilitation strategies directly relevant to whiplash management.
- National Center for Biotechnology Information (NCBI): Offers comprehensive access to biomedical literature including studies on whiplash pathophysiology, regenerative medicine, and biopsychosocial models in orthopedic care.
- National Institutes of Health (NIH): Publishes clinical trial data and guidelines emphasizing multidisciplinary approaches and psychological interventions for chronic whiplash-associated disorders.
- American Academy of Orthopaedic Surgeons (AAOS): Authoritative resource on orthopedic best practices, surgical indications, and emerging technologies in cervical spine injury treatment.
- Spine Journal: Specialized publication focusing on spinal injury diagnostics, advanced imaging techniques, and innovations in spine-related orthopedic treatments.
Conclusion
Whiplash injuries comprise a complex interplay of biomechanical, neurological, and psychosocial factors that require expert orthopedic evaluation and individualized care. From initial immobilization and targeted physical therapy to innovative regenerative treatments and AI-driven personalized rehabilitation, modern orthopedic approaches continuously evolve to optimize recovery and prevent chronic disability. Emphasizing early intervention, patient-centered communication, and integration of cutting-edge diagnostics and therapies ensures that each patient’s unique healing journey is supported comprehensively.
Understanding these nuanced treatment strategies empowers patients and clinicians alike to navigate whiplash with confidence and precision. We encourage you to share your experiences, ask questions, and explore further expert content to enrich your recovery and support others facing similar challenges.

The detailed explanation of how orthopedic specialists tailor treatment plans for whiplash injuries really stood out to me. The emphasis on comprehensive clinical assessment, including imaging like MRIs and X-rays, highlights how important it is to identify not just the obvious symptoms but any hidden complications like nerve involvement or disc herniation. I particularly appreciate the discussion around the balance between initial immobilization with cervical collars and the gradual shift towards active, progressive physical therapy. From my own recovery experience, early mobilization exercises coupled with pain management made a significant difference in regaining neck mobility without exacerbating symptoms.
Also, the integration of emerging therapies such as PRP injections and the use of wearable sensor technology for biomechanical monitoring sounds promising for the future of personalized treatment. However, it raises the question of accessibility and cost for many patients—how widely available are these advanced techniques currently, and what can be done to make them more accessible?
I’m curious, has anyone experienced or heard about using a combination of regenerative medicine and traditional physical therapy in their whiplash recovery? How do you balance the timing and intensity of these different approaches to avoid setbacks or accelerate healing? Sharing practical insights could benefit many navigating this complex journey.
Reading through this comprehensive overview has really reinforced how multifaceted whiplash recovery can be. I’ve seen firsthand how early appropriate intervention, combining immobilization with gradual, targeted physical therapy, can make a huge difference. One thing I’ve noticed in my own recovery—and from others’ stories—is that psychological support and managing stress related to injury play a crucial role alongside physical healing. Chronic pain isn’t purely physical; it affects mental health and motivation.
I’m particularly interested in the emerging regenerative therapies like PRP and stem cells. They sound promising, but I wonder about their availability in different regions and among various healthcare systems. Has anyone here had experience with these treatments, and how did they fit into a comprehensive rehab plan?
Finally, with all these cutting-edge innovations, what do you think is the best way for patients to stay informed about the latest options and advocate for their own recovery? Sharing insights on navigating this evolving landscape would be really valuable.