Unlocking the Language of Orthopedics: Why Diagnosis Codes Matter
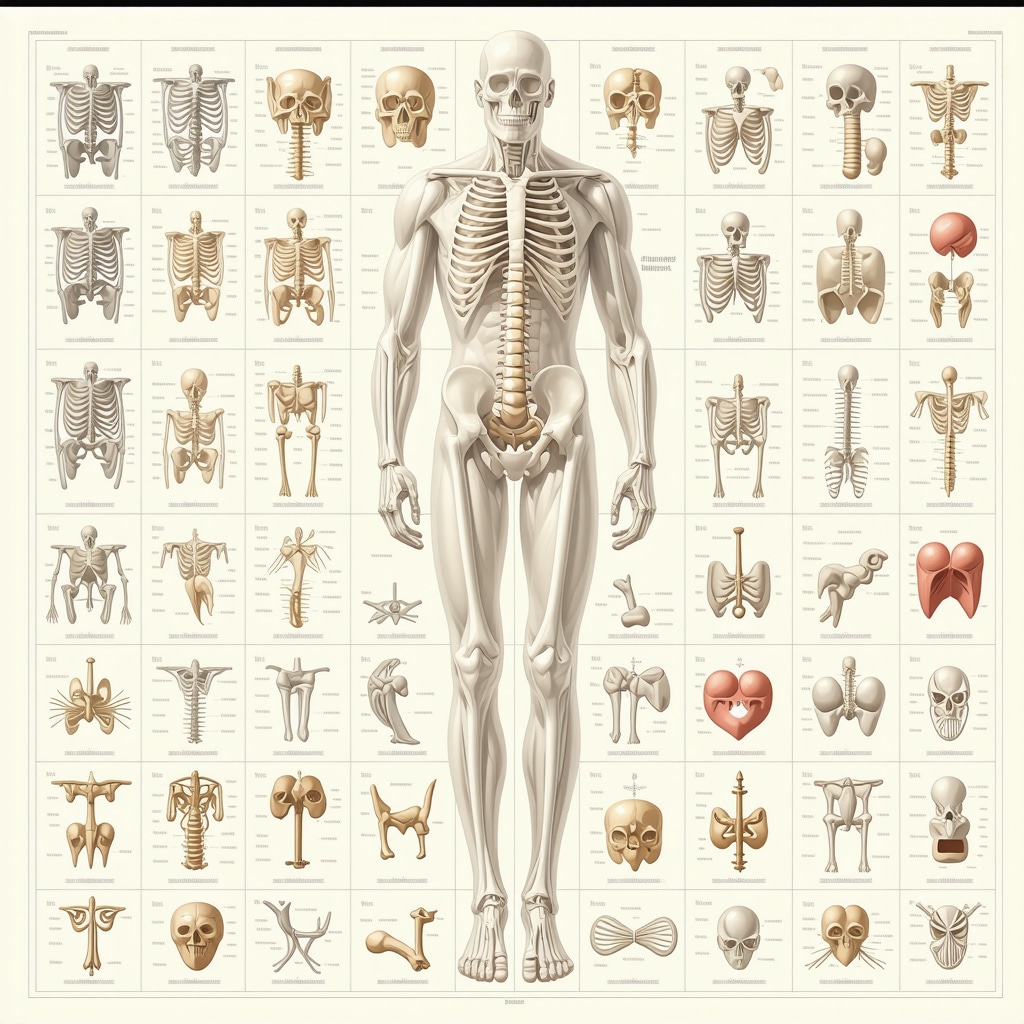
In the complex world of orthopedic medicine, diagnosis codes are the linchpin that connects patient symptoms, clinical findings, and treatment pathways. These codes, primarily from the ICD-10 system, enable healthcare professionals to accurately document and communicate specific musculoskeletal conditions across clinical, billing, and research settings. For practitioners and patients alike, understanding these codes offers a window into the precise nature of orthopedic diagnoses, facilitating better care coordination and insurance processing.
Decoding the Orthopedic Alphabet: A Comprehensive List of Common Diagnosis Codes
Orthopedic diagnosis codes span a vast array of conditions affecting bones, joints, ligaments, muscles, and nerves. Here are some essential ICD-10 codes frequently encountered in orthopedic practice:
- M16.0 – Primary osteoarthritis of the hip
- M17.0 – Primary osteoarthritis of the knee
- S43.4XXA – Sprain of shoulder joint, initial encounter
- M75.1 – Rotator cuff tear or rupture, not specified as traumatic
- M54.5 – Low back pain
- M50.20 – Cervical disc disorder, unspecified cervical region
- S83.2XXA – Tear of meniscus, current injury
Each code encapsulates a distinct orthopedic condition and its clinical context, guiding treatment decisions and insurance claims. These codes are intricately linked to procedural codes that define specific interventions, underscoring the importance of precise coding.
The Art and Science Behind Accurate Orthopedic Coding
Orthopedic coding is not just about selecting codes; it demands a nuanced understanding of anatomy, pathology, and clinical presentation. For example, a rotator cuff tear (M75.1) might be coded differently based on whether it is acute or chronic, traumatic or degenerative. Misclassification can lead to insurance denials or suboptimal treatment plans. Expert coders collaborate closely with orthopedic specialists to ensure that documentation captures all relevant details, a practice that significantly impacts patient outcomes and reimbursement accuracy.
How Do Orthopedic Diagnosis Codes Influence Patient Care and Insurance Processes?
Diagnosis codes are pivotal in shaping patient care pathways by informing clinical decision-making and eligibility for specific treatments. Insurance companies rely heavily on these codes to determine coverage approvals, reimbursement levels, and medical necessity. For instance, an accurate code for a herniated disc, such as M51.26 – Other intervertebral disc displacement, lumbar region, can unlock access to advanced non-surgical therapies that might otherwise be denied. This interplay underscores the critical role of orthopedic diagnosis codes beyond mere paperwork—they are gatekeepers to optimal care.
Practical Tips for Clinicians: Navigating Orthopedic Coding Challenges
Clinicians often face challenges like overlapping symptoms, comorbidities, and evolving diagnoses that complicate coding. Utilizing comprehensive consultation notes, such as those detailed in orthopedic consultation documentation, can enhance coding precision. Additionally, staying updated with coding guidelines and engaging in continuous education ensures that providers maintain coding excellence essential for both quality care and legal compliance.
For patients and practitioners seeking specialized spine care, understanding diagnosis codes can also facilitate informed decisions when choosing experts, as discussed in selecting the right orthopedic surgeon for your spine.
If this guide helped clarify complex orthopedic diagnosis codes, consider sharing it with colleagues or commenting below with your experiences or questions to foster a knowledgeable community.
For a deeper dive into orthopedic coding and care, exploring resources from the Centers for Disease Control and Prevention on ICD-10-CM offers authoritative insights and updates.
When Orthopedic Diagnosis Codes Meet Real-Life Patient Stories
Reflecting on my own journey in orthopedic care, I realize how much a precise diagnosis code can change everything. I remember a patient who came in with persistent knee pain, initially coded under a generic osteoarthritis label. Only after a thorough review and imaging did we update the code to M17.0 – Primary osteoarthritis of the knee. This nuance not only refined the treatment plan but also ensured insurance coverage for specific interventions, highlighting how these codes translate directly to patient experiences.
The Evolving Landscape: How Coding Changes Reflect Advances in Orthopedics
Orthopedic diagnosis codes are far from static; they evolve as medical understanding deepens. For example, newer codes now differentiate between acute and chronic conditions, helping tailor treatments more effectively. This dynamic nature requires clinicians and coders to stay on top of updates, much like staying current with the latest minimally invasive back pain treatments, which you can explore here. The synergy between updated coding and innovative treatments is vital for advancing patient care.
How Can Patients and Providers Collaborate to Ensure Coding Accuracy?
One question I often ponder is how patients can actively participate in ensuring their diagnosis codes are accurate. From my experience, open communication between patients and providers is key. Encouraging patients to ask questions about their diagnosis and treatment plans fosters transparency. Providers, on the other hand, benefit from detailed documentation and patient histories to capture the full picture. This partnership is essential because, as noted by the CDC on ICD-10-CM coding, accuracy in coding not only impacts care quality but also data used for epidemiological research and healthcare planning.
In practical terms, if you or someone you know is navigating orthopedic care, consider discussing the specific codes your provider is using. This can empower you to understand your condition better and advocate for appropriate treatments, especially when dealing with complex spine issues. For guidance on selecting the right orthopedic specialist, check out this resource that breaks down what to look for.
Challenges and Rewards: The Human Side of Orthopedic Coding
Coding can sometimes feel like a maze — with overlapping symptoms and multiple comorbidities, it’s easy for even seasoned clinicians to stumble. I recall a case involving a patient with both a rotator cuff tear and cervical disc disorder. Assigning codes M75.1 and M50.20 respectively was crucial for their insurance to approve a comprehensive treatment plan combining physical therapy and possible injections. Without precise coding, the patient might have faced delays or denials.
For fellow clinicians, I recommend leveraging detailed notes and collaborating with coding specialists, as highlighted in orthopedic consultation notes. This teamwork ensures that all clinical nuances are captured, ultimately benefiting patients through smoother care journeys.
If you’ve encountered challenges or successes related to orthopedic diagnosis codes or care, I’d love to hear your stories or questions in the comments below. Sharing experiences can build a supportive community around these often overlooked yet vital details.
Mastering Complex Orthopedic Coding: Strategies for Multimorbidity and Overlapping Diagnoses
Orthopedic patients frequently present with multiple concurrent conditions, which can complicate the coding process. For example, a patient may exhibit both degenerative joint disease and concurrent traumatic injury, necessitating the use of combination codes or multiple diagnosis codes to accurately reflect the clinical picture. The ICD-10-CM guidelines explicitly recommend sequencing diagnoses to indicate the primary reason for care while capturing all relevant comorbidities that influence treatment. This layered approach ensures that payers understand the full scope of the patient’s condition, which can be critical for reimbursement and care authorization.
In practice, clinicians and coders must collaborate closely to differentiate between chronic baseline conditions and acute exacerbations or new injuries. For instance, distinguishing between M17.0 (primary osteoarthritis of the knee) and a recent meniscal tear (S83.2XXA) requires detailed clinical documentation, including symptom onset, imaging results, and physical examination findings. Without this granularity, coders risk underrepresenting the patient’s condition, which can delay or limit access to appropriate interventions.
What Are the Best Practices for Documenting and Coding Complex Orthopedic Cases Involving Multiple Diagnoses?
Accurate documentation is paramount. Experts recommend the use of comprehensive orthopedic consultation notes that clearly delineate each diagnosis, its acuity, and its impact on the patient’s function. Utilizing standardized templates that prompt inclusion of specific details—such as laterality, chronicity, and injury mechanism—can enhance coding precision. Additionally, ongoing education about ICD-10-CM updates and payer-specific coding policies helps clinicians avoid common pitfalls.
Integration of electronic health records (EHR) with advanced coding software can further assist by flagging potential coding conflicts or omissions. When uncertainty arises, consulting with certified professional coders or orthopedic coding specialists is advisable to optimize accuracy.
Emerging Trends: Incorporating Precision Medicine and Biomarkers into Orthopedic Diagnosis Coding
Recent advances in orthopedic research have introduced precision medicine concepts, including the use of biomarkers and genetic profiling, which influence diagnosis and personalized treatment plans. These developments herald a future where traditional diagnosis codes may be augmented by modifiers or new codes that capture molecular or genetic data relevant to musculoskeletal diseases.
For example, osteoarthritis phenotyping based on inflammatory biomarkers could eventually be codified to differentiate subtypes that respond differently to therapeutic modalities. This evolution will require ongoing collaboration between clinical experts, coding authorities, and regulatory bodies to ensure that coding systems remain aligned with scientific progress and clinical utility.
Staying informed about these emerging coding frameworks will position providers to leverage advanced diagnostics effectively while maintaining compliance and optimizing reimbursement.
How Will the Integration of Genomic Data Transform Orthopedic Diagnosis Coding in the Next Decade?
The incorporation of genomic data into diagnostic coding promises to revolutionize personalized orthopedic care by enabling risk stratification, prognostication, and tailored interventions. However, challenges include developing standardized nomenclature, ensuring data privacy, and updating coding manuals to accommodate this complexity. Collaborative efforts from organizations like the American Medical Association and the World Health Organization will be pivotal in this transformation.
Clinicians and coders should anticipate gradual incorporation of these elements and proactively engage in education and system upgrades to harness the full potential of precision orthopedics.
For those interested in deepening their understanding of advanced orthopedic coding and emerging trends, consider exploring specialized workshops and certifications offered by the AAPC Certified Orthopedic Coder Program. Engaging with such expert resources can significantly enhance your coding proficiency and clinical impact.
Decoding Multimorbidity: Navigating the Intricacies of Orthopedic Coding in Complex Cases
Orthopedic patients often present with multifaceted clinical pictures, where chronic degenerative diseases coexist with acute traumatic injuries. This intersection requires a sophisticated coding approach that accurately reflects the dynamic interplay of conditions. For instance, integrating codes that distinguish baseline osteoarthritis from recent ligamentous injuries not only clarifies clinical intent but also optimizes insurance adjudication and clinical outcome tracking. Precision in sequencing and specificity remains paramount to capture the full spectrum of patient pathology.
What Are the Best Practices for Documenting and Coding Complex Orthopedic Cases Involving Multiple Diagnoses?
Experts emphasize comprehensive documentation protocols that encapsulate laterality, acuity, and etiological factors. Utilizing standardized orthopedic consultation templates ensures inclusion of critical clinical details such as symptom chronology, imaging findings, and functional impairment levels. Furthermore, leveraging electronic health record (EHR) systems integrated with intelligent coding software can preempt common errors by flagging coding conflicts or incomplete entries. Collaboration between clinicians and certified orthopedic coders is indispensable for navigating the nuanced coding landscape, thereby enhancing reimbursement accuracy and patient care continuity.
Precision Medicine Meets Orthopedics: The Future of Diagnosis Coding in a Genomic Era
Recent advancements in biomarker discovery and genetic profiling are catalyzing a paradigm shift in orthopedic diagnostics. This evolution anticipates the augmentation of traditional ICD-10 codes with molecular and genetic modifiers that delineate disease subtypes and predict therapeutic responsiveness. For example, osteoarthritis classification may soon incorporate inflammatory biomarker profiles, facilitating personalized treatment algorithms and refined prognostication.
Such a transition demands ongoing collaboration among clinical experts, coding authorities, and regulatory agencies to harmonize coding frameworks with scientific breakthroughs while preserving clinical utility and billing integrity.
How Will the Integration of Genomic Data Transform Orthopedic Diagnosis Coding in the Next Decade?
The integration of genomic insights promises to revolutionize orthopedic care by enabling individualized risk stratification and tailored interventions. Nonetheless, challenges including standardized genomic nomenclature, data privacy safeguards, and comprehensive coder education must be addressed. Organizations like the AAPC Certified Orthopedic Coder Program and the CDC ICD-10-CM resources provide invaluable frameworks for clinicians and coders to adapt proactively to these transformative trends.
Leveraging Technology and Expertise: Elevating Orthopedic Coding Accuracy and Efficiency
The advent of sophisticated electronic health records integrated with artificial intelligence-driven coding assistants is reshaping orthopedic documentation workflows. These tools facilitate real-time validation of diagnosis codes against clinical narratives, significantly reducing errors and enhancing compliance. Moreover, continuous professional development through specialized workshops and certifications empowers practitioners to master evolving coding standards and complex case scenarios.
Clinicians are encouraged to adopt collaborative models involving multidisciplinary teams, including orthopedic surgeons, coders, and billing specialists, to ensure that documentation truly mirrors clinical complexity and meets payer expectations.
Engage with Expert Insights: Elevate Your Orthopedic Coding Practices Today
For professionals navigating the complexities of orthopedic diagnosis coding, embracing these advanced strategies and emerging trends is essential. By integrating precision medicine insights, leveraging cutting-edge technology, and fostering interdisciplinary collaboration, you can significantly enhance coding accuracy and patient care outcomes.
We invite you to delve deeper into these topics by exploring expert certification programs and authoritative resources. Share your experiences or pose your questions in the comments to join a community committed to excellence in orthopedic coding.
Frequently Asked Questions (FAQ)
What are orthopedic diagnosis codes and why are they important?
Orthopedic diagnosis codes, primarily from the ICD-10-CM system, are standardized alphanumeric codes that classify musculoskeletal conditions such as fractures, arthritis, and ligament injuries. They are crucial for accurate documentation, guiding treatment plans, facilitating insurance reimbursement, and enabling epidemiological tracking in orthopedic care.
How do clinicians ensure accuracy when coding complex orthopedic cases with multiple diagnoses?
Accuracy in complex cases is achieved through comprehensive documentation that details each condition’s acuity, laterality, and etiology. Using standardized consultation notes, leveraging EHR-integrated coding tools, and collaborating closely with certified orthopedic coders help differentiate between chronic and acute conditions, ensuring precise code assignment and optimal reimbursement.
Can patients influence the accuracy of their orthopedic diagnosis codes?
Yes, patients play a vital role by engaging in open communication with their providers, asking questions about their diagnoses, and reviewing their medical records. Understanding the specific codes used promotes transparency and empowers patients to advocate for appropriate treatments and insurance coverage.
What challenges do providers face with orthopedic coding, and how can they overcome them?
Challenges include overlapping symptoms, multimorbidity, and rapidly evolving coding guidelines. Providers can overcome these by maintaining detailed clinical documentation, participating in continuous coding education, utilizing advanced EHR coding software, and fostering teamwork with coding specialists to ensure compliance and accuracy.
How are emerging trends like precision medicine impacting orthopedic diagnosis coding?
Precision medicine introduces biomarkers and genomic data that may augment traditional diagnosis codes, enabling more personalized treatment approaches. This requires new coding modifiers or codes to capture molecular subtypes, necessitating ongoing updates to coding standards and education for clinicians and coders to integrate these advances effectively.
What role do technology and artificial intelligence play in improving orthopedic coding?
AI-driven coding assistants integrated with electronic health records help validate diagnosis codes in real time, reduce errors, and enhance compliance. These technologies streamline workflows and support clinicians by flagging inconsistencies, promoting coding accuracy and efficiency in orthopedic documentation.
How should multiple orthopedic diagnoses be sequenced in coding?
The primary diagnosis should reflect the main reason for the encounter or treatment, with secondary codes capturing comorbidities or concurrent conditions. Proper sequencing clarifies clinical priorities and influences payer decisions, ensuring that all relevant pathologies are documented for comprehensive care management.
Where can clinicians find authoritative resources for orthopedic diagnosis coding updates?
Clinicians can consult resources such as the CDC’s ICD-10-CM official guidelines, the American Academy of Orthopaedic Surgeons (AAOS) coding manuals, and professional organizations like AAPC for certification programs and updated coding policies tailored to orthopedic practice.
How will genomic data integration address privacy and standardization in orthopedic coding?
Integration demands development of standardized genomic nomenclature and robust data privacy safeguards. Collaborative efforts from regulatory bodies and professional organizations aim to establish secure frameworks and coding standards that balance innovation with patient confidentiality and data integrity.
What certifications or training are recommended to enhance expertise in orthopedic coding?
Programs like the AAPC Certified Orthopedic Coder Program provide specialized training to master complex orthopedic codes, updates, and best practices, equipping clinicians and coders to improve documentation quality and reimbursement outcomes.
Trusted External Sources
- Centers for Disease Control and Prevention (CDC) – ICD-10-CM Resources: Offers the official ICD-10-CM coding guidelines and updates critical for accurate diagnosis coding in orthopedics.
- American Academy of Orthopaedic Surgeons (AAOS): Provides comprehensive coding manuals and clinical practice guidelines that support precise orthopedic documentation and coding.
- American Academy of Professional Coders (AAPC): Offers certification programs and coding resources specific to orthopedic coding complexities and emerging trends.
- World Health Organization (WHO) – ICD-10 and ICD-11 Standards: The authoritative body that develops and maintains international disease classification systems, including updates relevant to orthopedic conditions.
- National Center for Health Statistics (NCHS): Provides data and guidelines that underpin coding standards and quality assurance in musculoskeletal diagnostics.
Conclusion
Orthopedic diagnosis codes are foundational to effective musculoskeletal healthcare, bridging clinical insight with administrative precision. Mastery of these codes demands a deep understanding of anatomy, pathology, and evolving diagnostic paradigms, especially when managing complex, multimorbid patients. Emerging trends in precision medicine and technological advancements promise to further refine coding accuracy and personalized care. By embracing continuous education, leveraging interdisciplinary collaboration, and utilizing innovative tools, clinicians and coders can enhance patient outcomes, streamline insurance processes, and contribute to the advancement of orthopedic medicine. Engage with this knowledge—share, comment, and explore specialized resources—to elevate your orthopedic coding practice and optimize care delivery.

This comprehensive overview of orthopedic diagnosis codes truly highlights how crucial precise documentation is in clinical practice. I’ve seen firsthand how accurate coding can impact both patient care and insurance reimbursement, especially with complex cases involving multiple conditions. It’s interesting to note how evolving coding standards, like differentiating between acute and chronic conditions, directly influence treatment planning. I particularly agree on the importance of detailed documentation and collaboration with coding specialists. In my experience, proactive communication with patients about their diagnoses and understanding the specific codes used can empower them and enhance transparency. Have others found that involving patients in discussions about diagnosis codes improves their engagement and satisfaction? Also, what are some effective strategies you’ve used to stay current with the rapidly changing coding guidelines? It seems like ongoing education and leveraging technology, such as EHR systems with integrated coding tools, are becoming essential for accuracy.