Unlocking the Path to Shoulder Healing: The Role of Your Orthopedic Doctor in Rotator Cuff Tear Treatment
Experiencing persistent shoulder pain or weakness can be a sign of a rotator cuff tear, a common yet often misunderstood injury. Understanding what to expect when seeking treatment from an orthopedic doctor can empower you to navigate your recovery journey with confidence and clarity. This article dives deep into expert approaches, innovative therapies, and practical steps tailored to help restore shoulder function and quality of life.
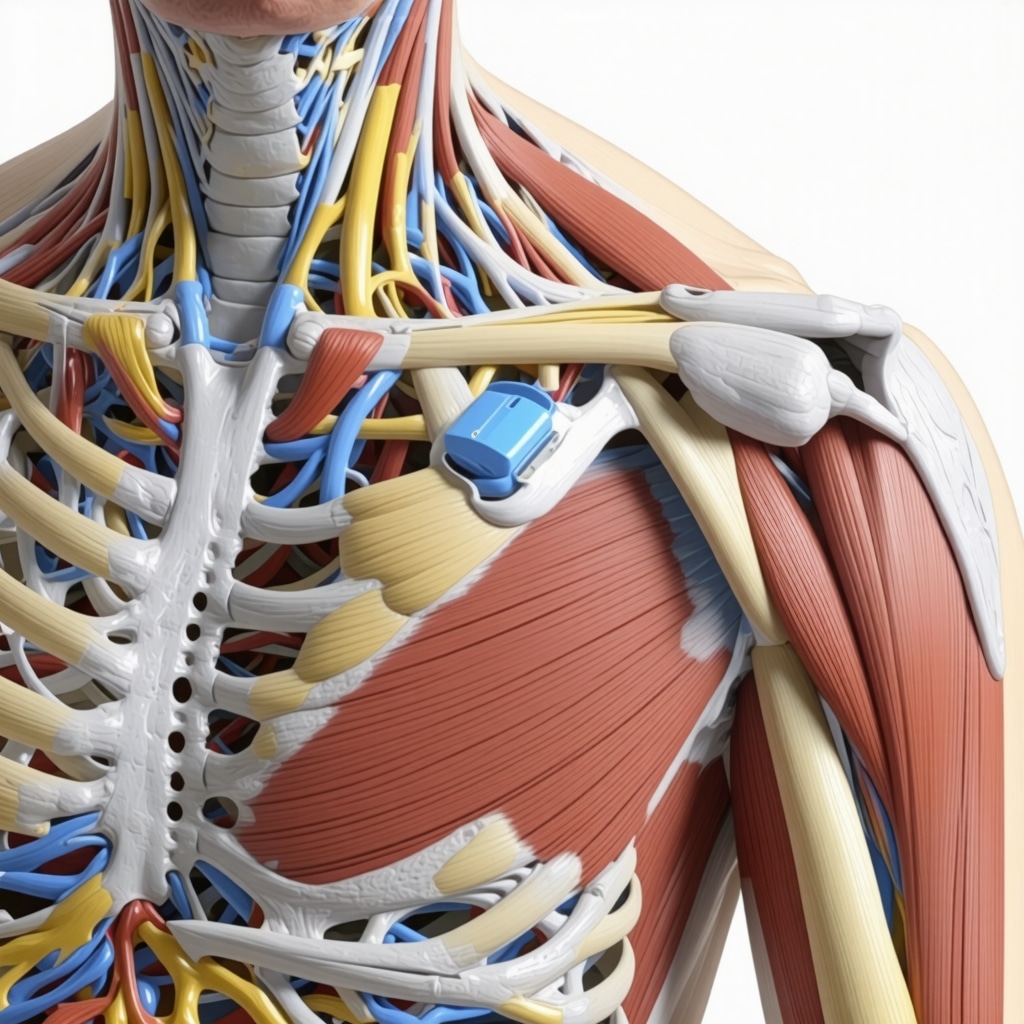
The Anatomy of Recovery: How Orthopedic Specialists Diagnose and Plan Treatment
Orthopedic doctors begin with a comprehensive evaluation involving detailed patient history, physical examination, and advanced imaging techniques like MRI or ultrasound to precisely identify the extent and location of the rotator cuff tear. This meticulous diagnostic phase is critical for crafting a personalized treatment plan that balances conservative management with surgical options when necessary.
Dynamic Treatment Strategies: From Non-Surgical Care to Advanced Surgical Interventions
Non-surgical rotator cuff tear treatments often serve as the first line of defense and include physical therapy, anti-inflammatory medications, and orthopedic injections designed to reduce pain and promote healing. For more severe or persistent tears, minimally invasive arthroscopic surgery may be recommended to repair the damaged tendons. Surgeons utilize refined techniques to minimize tissue disruption, facilitating quicker recovery and better functional outcomes.
What Should Patients Expect During the Rotator Cuff Tear Rehabilitation Process?
Post-treatment rehabilitation is a critical cornerstone to successful recovery. Patients can anticipate a structured physical therapy regimen focusing initially on pain management and gentle mobilization, gradually progressing to strength-building exercises that restore shoulder stability and range of motion. The orthopedic doctor will often coordinate closely with rehabilitation specialists to monitor progress and adjust protocols, ensuring a safe and effective return to daily activities and sports.
Integrating Cutting-Edge Orthopedic Care with Personalized Patient Support
Modern orthopedic care for rotator cuff injuries emphasizes a holistic approach, blending medical expertise with patient education and support systems. Orthopedic doctors not only address the physical injury but also guide lifestyle adjustments to prevent re-injury. For those interested in exploring comprehensive treatment options, resources such as choosing the right orthopedic doctor for rotator cuff tear treatment offer valuable insights.
Evidence-Based Insights: Trusting Orthopedic Expertise Backed by Research
According to research published by the American Academy of Orthopaedic Surgeons (AAOS), early intervention combined with tailored rehabilitation significantly improves outcomes for rotator cuff tears (source). Orthopedic doctors leverage such evidence to optimize treatment pathways, balancing innovation with proven modalities to enhance healing.
Engage and Empower: Share Your Rotator Cuff Recovery Experience or Questions
Have you recently undergone rotator cuff treatment or are considering your options? Share your story or ask questions in the comments below to connect with others navigating similar challenges and gain expert feedback.
Real-Life Reflections: My Journey Through Rotator Cuff Tear Rehabilitation
When I first faced the reality of a rotator cuff tear, the flood of questions and uncertainty was overwhelming. How long would it take to heal? Could I regain full function? The answers weren’t immediate, but through close collaboration with my orthopedic doctor and physical therapist, I discovered that patience and persistence are just as vital as the treatment itself.
One of the most valuable lessons I learned was the importance of listening to my body while adhering to the prescribed rehabilitation protocols. Early on, gentle mobilization exercises helped reduce stiffness and pain, making daily tasks more manageable. As weeks progressed, gradually increasing strength-building activities restored my confidence and shoulder stability.
The Role of Patient Education in Empowering Your Recovery
Beyond medical interventions, my orthopedic doctor emphasized understanding the mechanics of the shoulder and the nature of my injury. This knowledge transformed my approach to rehab — I wasn’t just going through motions but actively participating in my healing process. This aligns with findings from the American Academy of Orthopaedic Surgeons, which highlight that patient education combined with tailored therapy boosts recovery outcomes (AAOS source).
How Can You Stay Motivated During the Slow Phases of Recovery?
Recovery can sometimes feel like a slow climb, especially when progress plateaus or setbacks occur. I found that setting small, achievable goals and celebrating each milestone made the journey more manageable. Whether it was regaining a few degrees of motion or experiencing less discomfort during sleep, these wins kept my spirits high.
Connecting with others who have undergone similar treatments also provided emotional support and practical tips. If you’re interested, communities often gather online or through local support groups, which can be a valuable resource.
Practical Tips: Integrating Orthopedic Care With Daily Life
Incorporating lifestyle adjustments was another key aspect of my recovery. Ergonomic modifications at work, such as using a supportive chair and adjusting desk height, helped reduce unnecessary strain on my healing shoulder. If you’re a desk worker, exploring orthopedic support braces might also be beneficial, as discussed in this guide on orthopedic support for desk workers.
Moreover, staying consistent with home exercises prescribed by my therapist ensured that I maintained progress even outside clinic visits. It’s a reminder that orthopedic care extends beyond the doctor’s office — it’s a lifestyle commitment.
When Should You Consider Getting a Second Opinion?
While my orthopedic team provided excellent care, I also explored the option of getting a second opinion to confirm the diagnosis and treatment plan. This step can be crucial if you feel uncertain or your symptoms persist despite therapy. Resources like getting a second opinion from an orthopedic surgeon offer guidance on how to approach this process thoughtfully and effectively.
Let’s Keep the Conversation Going!
Have you or someone you know experienced a rotator cuff tear? What strategies or treatments worked best for you? I’d love to hear your stories, questions, or tips in the comments below. Sharing our experiences helps build a supportive community and empowers everyone on their path to healing.
Revolutionizing Rotator Cuff Repair: Integrating Biologic Therapies with Surgical Precision
In recent years, orthopedic surgery for rotator cuff tears has transcended traditional repair methods by incorporating biologic adjuncts such as platelet-rich plasma (PRP) and stem cell therapies. These cutting-edge modalities aim to enhance tendon healing by stimulating the body’s natural regenerative capacities. Orthopedic surgeons meticulously assess patient candidacy for these treatments, considering factors like tear chronicity, tissue quality, and systemic health, to optimize outcomes.
For instance, PRP injections administered intraoperatively or during early rehabilitation phases can modulate inflammation and promote collagen synthesis, potentially reducing re-tear rates. Meanwhile, mesenchymal stem cell therapies are being explored for their ability to differentiate into tendon-like cells and secrete bioactive molecules that facilitate repair. Though currently more prevalent in clinical trials, these biologics represent a promising frontier that orthopedic specialists are eagerly integrating into comprehensive care plans.
How Do Orthopedic Experts Determine the Suitability of Biologic Treatments for Rotator Cuff Tears?
Determining the appropriateness of biologic therapies involves a multifaceted evaluation. Orthopedic doctors analyze the severity and size of the tear, patient age, activity level, and comorbidities such as diabetes or smoking status, which may impair healing. Imaging studies provide insight into tendon quality and muscle atrophy, influencing decision-making. Furthermore, evidence from randomized controlled trials—like those reviewed in the Journal of Orthopaedic Research—guides clinicians on efficacy and timing.
This precision medicine approach ensures that biologic interventions complement mechanical repair without unnecessary risks or costs. Patients benefit from a tailored plan that maximizes functional restoration while minimizing complications.
Advanced Rehabilitation Paradigms: Neuromuscular Re-education and Proprioceptive Training Post-Rotator Cuff Repair
Beyond conventional strengthening, contemporary rehabilitation protocols increasingly emphasize neuromuscular re-education to restore shoulder joint proprioception and dynamic stability. This is critical because rotator cuff tears disrupt the intricate sensorimotor pathways that coordinate shoulder movement, often leading to compensatory patterns and increased injury risk.
Physical therapists employ specialized exercises involving closed kinetic chain activities, perturbation training, and biofeedback techniques to retrain muscle firing sequences. Early incorporation of these elements has demonstrated improved joint kinematics, reduced pain, and enhanced functional outcomes. The orthopedic physician and rehabilitation team collaborate closely, monitoring patient response and adjusting intensity to balance tissue healing with neuromuscular demands.
Augmenting Patient Outcomes Through Digital Health Technologies and Remote Monitoring
The integration of telemedicine and wearable sensor technologies into orthopedic care pathways is transforming rotator cuff tear management. These tools facilitate continuous monitoring of adherence to rehabilitation exercises, range of motion, and even muscle activation patterns remotely, enabling timely intervention if deviations or complications arise.
For example, wearable inertial measurement units (IMUs) can quantify shoulder movement quality during home exercises, providing real-time feedback to both patients and clinicians. Mobile applications designed by orthopedic experts deliver personalized exercise regimens with instructional videos and progress tracking, increasing patient engagement and motivation.
This digital shift not only enhances accessibility but also empowers patients to take an active role in their recovery journey, fostering better long-term outcomes.
Exploring the Complexities of Rotator Cuff Tear Healing: What Are the Biological and Mechanical Challenges?
Rotator cuff tendon healing is inherently complex due to the unique enthesis structure—the interface between tendon and bone—that necessitates regeneration of a gradient of tissues with distinct mechanical properties. Achieving a robust, functional repair involves overcoming challenges such as poor vascularity, chronic inflammation, and mechanical loading stresses during rehabilitation.
Orthopedic researchers are investigating biomaterial scaffolds and gene therapy approaches to facilitate enthesis regeneration and improve biomechanical strength of repairs. Understanding these biological and mechanical intricacies is essential for orthopedic doctors to tailor surgical techniques and post-operative protocols that optimize tendon-bone integration.
Continued advancements in this domain promise to reduce failure rates and enhance durability of rotator cuff repairs.
Join the Expert Discussion: Elevate Your Understanding of Rotator Cuff Tear Innovations
Are you intrigued by the evolving landscape of rotator cuff tear treatments or eager to explore how emerging biologics and digital tools might revolutionize your recovery? Engage with our expert community by sharing your questions or experiences below. Delve deeper into evidence-based practices and innovative strategies that can empower your healing journey with unparalleled insight.
Unlocking the Path to Shoulder Healing: The Role of Your Orthopedic Doctor in Rotator Cuff Tear Treatment
Experiencing persistent shoulder pain or weakness can be a sign of a rotator cuff tear, a common yet often misunderstood injury. Understanding what to expect when seeking treatment from an orthopedic doctor can empower you to navigate your recovery journey with confidence and clarity. This article dives deep into expert approaches, innovative therapies, and practical steps tailored to help restore shoulder function and quality of life.
The Anatomy of Recovery: How Orthopedic Specialists Diagnose and Plan Treatment
Orthopedic doctors begin with a comprehensive evaluation involving detailed patient history, physical examination, and advanced imaging techniques like MRI or ultrasound to precisely identify the extent and location of the rotator cuff tear. This meticulous diagnostic phase is critical for crafting a personalized treatment plan that balances conservative management with surgical options when necessary.
Dynamic Treatment Strategies: From Non-Surgical Care to Advanced Surgical Interventions
Non-surgical rotator cuff tear treatments often serve as the first line of defense and include physical therapy, anti-inflammatory medications, and orthopedic injections designed to reduce pain and promote healing. For more severe or persistent tears, minimally invasive arthroscopic surgery may be recommended to repair the damaged tendons. Surgeons utilize refined techniques to minimize tissue disruption, facilitating quicker recovery and better functional outcomes.
What Should Patients Expect During the Rotator Cuff Tear Rehabilitation Process?
Post-treatment rehabilitation is a critical cornerstone to successful recovery. Patients can anticipate a structured physical therapy regimen focusing initially on pain management and gentle mobilization, gradually progressing to strength-building exercises that restore shoulder stability and range of motion. The orthopedic doctor will often coordinate closely with rehabilitation specialists to monitor progress and adjust protocols, ensuring a safe and effective return to daily activities and sports.
Integrating Cutting-Edge Orthopedic Care with Personalized Patient Support
Modern orthopedic care for rotator cuff injuries emphasizes a holistic approach, blending medical expertise with patient education and support systems. Orthopedic doctors not only address the physical injury but also guide lifestyle adjustments to prevent re-injury. For those interested in exploring comprehensive treatment options, resources such as choosing the right orthopedic doctor for rotator cuff tear treatment offer valuable insights.
Evidence-Based Insights: Trusting Orthopedic Expertise Backed by Research
According to research published by the American Academy of Orthopaedic Surgeons (AAOS), early intervention combined with tailored rehabilitation significantly improves outcomes for rotator cuff tears (source). Orthopedic doctors leverage such evidence to optimize treatment pathways, balancing innovation with proven modalities to enhance healing.
Engage and Empower: Share Your Rotator Cuff Recovery Experience or Questions
Have you recently undergone rotator cuff treatment or are considering your options? Share your story or ask questions in the comments below to connect with others navigating similar challenges and gain expert feedback.
Real-Life Reflections: My Journey Through Rotator Cuff Tear Rehabilitation
When I first faced the reality of a rotator cuff tear, the flood of questions and uncertainty was overwhelming. How long would it take to heal? Could I regain full function? The answers weren’t immediate, but through close collaboration with my orthopedic doctor and physical therapist, I discovered that patience and persistence are just as vital as the treatment itself.
One of the most valuable lessons I learned was the importance of listening to my body while adhering to the prescribed rehabilitation protocols. Early on, gentle mobilization exercises helped reduce stiffness and pain, making daily tasks more manageable. As weeks progressed, gradually increasing strength-building activities restored my confidence and shoulder stability.
The Role of Patient Education in Empowering Your Recovery
Beyond medical interventions, my orthopedic doctor emphasized understanding the mechanics of the shoulder and the nature of my injury. This knowledge transformed my approach to rehab — I wasn’t just going through motions but actively participating in my healing process. This aligns with findings from the American Academy of Orthopaedic Surgeons, which highlight that patient education combined with tailored therapy boosts recovery outcomes (AAOS source).
How Can You Stay Motivated During the Slow Phases of Recovery?
Recovery can sometimes feel like a slow climb, especially when progress plateaus or setbacks occur. I found that setting small, achievable goals and celebrating each milestone made the journey more manageable. Whether it was regaining a few degrees of motion or experiencing less discomfort during sleep, these wins kept my spirits high.
Connecting with others who have undergone similar treatments also provided emotional support and practical tips. If you’re interested, communities often gather online or through local support groups, which can be a valuable resource.
Practical Tips: Integrating Orthopedic Care With Daily Life
Incorporating lifestyle adjustments was another key aspect of my recovery. Ergonomic modifications at work, such as using a supportive chair and adjusting desk height, helped reduce unnecessary strain on my healing shoulder. If you’re a desk worker, exploring orthopedic support braces might also be beneficial, as discussed in this guide on orthopedic support for desk workers.
Moreover, staying consistent with home exercises prescribed by my therapist ensured that I maintained progress even outside clinic visits. It’s a reminder that orthopedic care extends beyond the doctor’s office — it’s a lifestyle commitment.
When Should You Consider Getting a Second Opinion?
While my orthopedic team provided excellent care, I also explored the option of getting a second opinion to confirm the diagnosis and treatment plan. This step can be crucial if you feel uncertain or your symptoms persist despite therapy. Resources like getting a second opinion from an orthopedic surgeon offer guidance on how to approach this process thoughtfully and effectively.
Let’s Keep the Conversation Going!
Have you or someone you know experienced a rotator cuff tear? What strategies or treatments worked best for you? I’d love to hear your stories, questions, or tips in the comments below. Sharing our experiences helps build a supportive community and empowers everyone on their path to healing.
Revolutionizing Rotator Cuff Repair: Integrating Biologic Therapies with Surgical Precision
In recent years, orthopedic surgery for rotator cuff tears has transcended traditional repair methods by incorporating biologic adjuncts such as platelet-rich plasma (PRP) and stem cell therapies. These cutting-edge modalities aim to enhance tendon healing by stimulating the body’s natural regenerative capacities. Orthopedic surgeons meticulously assess patient candidacy for these treatments, considering factors like tear chronicity, tissue quality, and systemic health, to optimize outcomes.
For instance, PRP injections administered intraoperatively or during early rehabilitation phases can modulate inflammation and promote collagen synthesis, potentially reducing re-tear rates. Meanwhile, mesenchymal stem cell therapies are being explored for their ability to differentiate into tendon-like cells and secrete bioactive molecules that facilitate repair. Though currently more prevalent in clinical trials, these biologics represent a promising frontier that orthopedic specialists are eagerly integrating into comprehensive care plans.
How Do Orthopedic Experts Determine the Suitability of Biologic Treatments for Rotator Cuff Tears?
Determining the appropriateness of biologic therapies involves a multifaceted evaluation. Orthopedic doctors analyze the severity and size of the tear, patient age, activity level, and comorbidities such as diabetes or smoking status, which may impair healing. Imaging studies provide insight into tendon quality and muscle atrophy, influencing decision-making. Furthermore, evidence from randomized controlled trials—like those reviewed in the Journal of Orthopaedic Research—guides clinicians on efficacy and timing.
This precision medicine approach ensures that biologic interventions complement mechanical repair without unnecessary risks or costs. Patients benefit from a tailored plan that maximizes functional restoration while minimizing complications.
Advanced Rehabilitation Paradigms: Neuromuscular Re-education and Proprioceptive Training Post-Rotator Cuff Repair
Beyond conventional strengthening, contemporary rehabilitation protocols increasingly emphasize neuromuscular re-education to restore shoulder joint proprioception and dynamic stability. This is critical because rotator cuff tears disrupt the intricate sensorimotor pathways that coordinate shoulder movement, often leading to compensatory patterns and increased injury risk.
Physical therapists employ specialized exercises involving closed kinetic chain activities, perturbation training, and biofeedback techniques to retrain muscle firing sequences. Early incorporation of these elements has demonstrated improved joint kinematics, reduced pain, and enhanced functional outcomes. The orthopedic physician and rehabilitation team collaborate closely, monitoring patient response and adjusting intensity to balance tissue healing with neuromuscular demands.
Augmenting Patient Outcomes Through Digital Health Technologies and Remote Monitoring
The integration of telemedicine and wearable sensor technologies into orthopedic care pathways is transforming rotator cuff tear management. These tools facilitate continuous monitoring of adherence to rehabilitation exercises, range of motion, and even muscle activation patterns remotely, enabling timely intervention if deviations or complications arise.
For example, wearable inertial measurement units (IMUs) can quantify shoulder movement quality during home exercises, providing real-time feedback to both patients and clinicians. Mobile applications designed by orthopedic experts deliver personalized exercise regimens with instructional videos and progress tracking, increasing patient engagement and motivation.
This digital shift not only enhances accessibility but also empowers patients to take an active role in their recovery journey, fostering better long-term outcomes.
Exploring the Complexities of Rotator Cuff Tear Healing: What Are the Biological and Mechanical Challenges?
Rotator cuff tendon healing is inherently complex due to the unique enthesis structure—the interface between tendon and bone—that necessitates regeneration of a gradient of tissues with distinct mechanical properties. Achieving a robust, functional repair involves overcoming challenges such as poor vascularity, chronic inflammation, and mechanical loading stresses during rehabilitation.
Orthopedic researchers are investigating biomaterial scaffolds and gene therapy approaches to facilitate enthesis regeneration and improve biomechanical strength of repairs. Understanding these biological and mechanical intricacies is essential for orthopedic doctors to tailor surgical techniques and post-operative protocols that optimize tendon-bone integration.
Continued advancements in this domain promise to reduce failure rates and enhance durability of rotator cuff repairs.
Join the Expert Discussion: Elevate Your Understanding of Rotator Cuff Tear Innovations
Are you intrigued by the evolving landscape of rotator cuff tear treatments or eager to explore how emerging biologics and digital tools might revolutionize your recovery? Engage with our expert community by sharing your questions or experiences below. Delve deeper into evidence-based practices and innovative strategies that can empower your healing journey with unparalleled insight.
Frequently Asked Questions (FAQ)
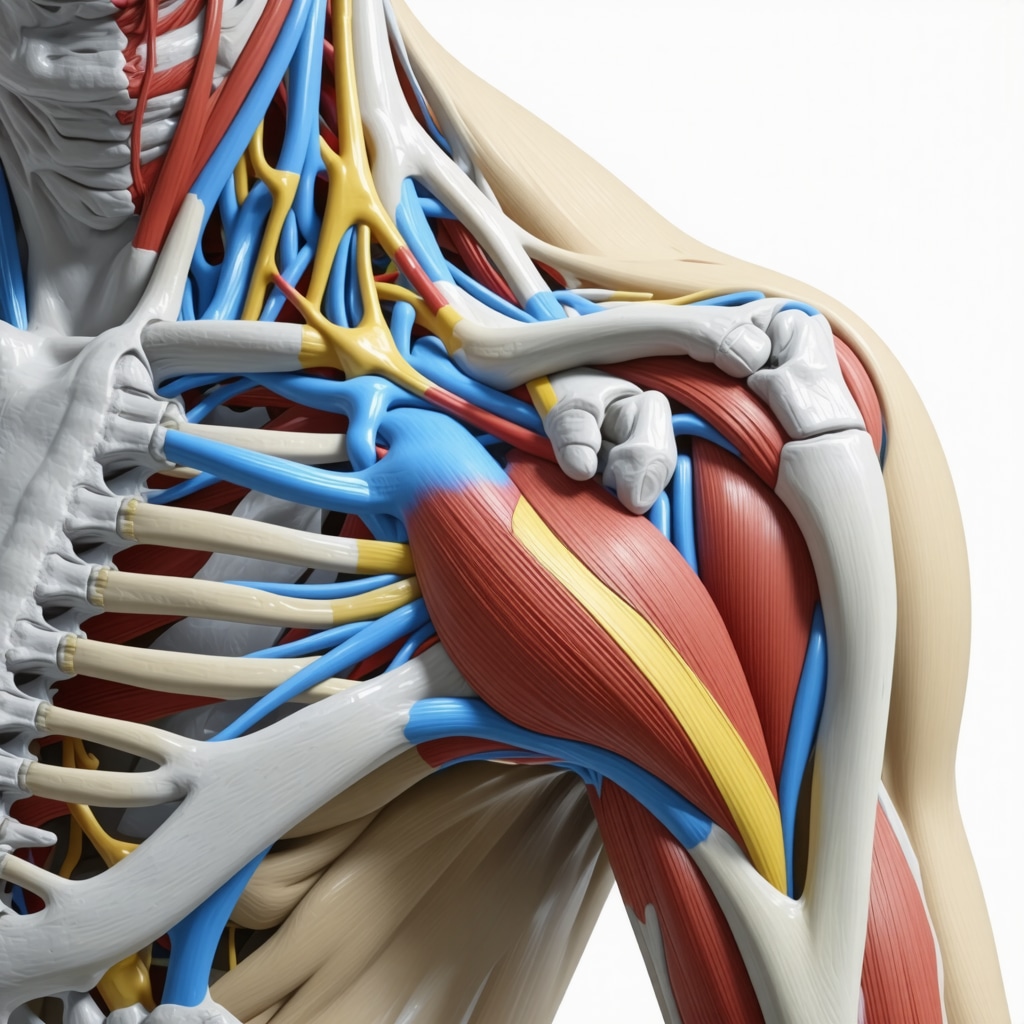
What exactly is a rotator cuff tear and how does it affect shoulder function?
A rotator cuff tear involves damage to one or more of the four tendons that stabilize and move the shoulder joint. This injury impairs shoulder strength, range of motion, and can cause persistent pain, limiting everyday activities and athletic performance.
How do orthopedic doctors diagnose the severity of a rotator cuff tear?
Diagnosis includes a detailed patient history, physical examination assessing range of motion and strength, and advanced imaging such as MRI or ultrasound. These tools help determine tear size, location, tendon quality, and muscle condition, critical for tailoring treatment plans.
When is surgery recommended over non-surgical treatments for rotator cuff tears?
Surgery is typically advised for large, full-thickness tears, persistent symptoms despite conservative care, or tears in younger, active patients aiming for full functional recovery. Smaller or partial tears often respond well to physical therapy, anti-inflammatories, and injections.
What innovative biologic therapies are currently used to enhance rotator cuff repair?
Orthopedic surgeons are incorporating platelet-rich plasma (PRP) and mesenchymal stem cell therapies to stimulate tendon healing and reduce inflammation. These biologics are selected based on individual patient factors and are often adjuncts to surgical repair or early rehabilitation.
How important is rehabilitation after rotator cuff treatment, and what does it involve?
Rehabilitation is critical to restoring shoulder function. It progresses from pain management and gentle mobilization to neuromuscular re-education, proprioceptive training, and strength building. Close coordination between orthopedic doctors and therapists ensures safe and effective recovery.
Can digital health technologies improve rotator cuff tear recovery?
Yes, telemedicine, wearable sensors, and mobile apps enable remote monitoring of exercise adherence and movement quality. These tools provide real-time feedback, increase patient engagement, and allow timely clinical interventions to optimize outcomes.
What lifestyle adjustments can support healing and prevent re-injury?
Ergonomic modifications at work, avoiding repetitive overhead activities, maintaining shoulder conditioning, and using orthopedic supports as needed help reduce strain on the healing tendon, promoting durable recovery.
When should a patient consider getting a second opinion for rotator cuff treatment?
If symptoms persist despite treatment, diagnosis is unclear, or surgery is recommended but the patient feels uncertain, seeking a second opinion from another orthopedic specialist can provide reassurance and alternative perspectives.
Are there biological and mechanical challenges unique to rotator cuff healing?
Yes, the tendon-to-bone interface (enthesis) requires regeneration of complex tissue gradients with differing mechanical properties. Poor blood supply and mechanical stress complicate healing, necessitating advanced surgical techniques and tailored rehab protocols.
How can patients stay motivated during slow or plateau phases of recovery?
Setting achievable goals, celebrating small improvements, and connecting with support communities can sustain motivation. Understanding the healing process and active involvement in rehabilitation empower patients through challenging phases.
Trusted External Sources
- American Academy of Orthopaedic Surgeons (AAOS) – Provides authoritative clinical guidelines, patient education resources, and evidence-based updates on rotator cuff pathology and treatment strategies.
- Journal of Orthopaedic Research – Publishes peer-reviewed studies on biologic therapies, surgical innovations, and tendon healing mechanisms essential for advancing orthopedic care.
- National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) – Offers comprehensive information on musculoskeletal disorders including rotator cuff injuries, supporting patient awareness and research advances.
- Orthopaedic Journal of Sports Medicine – Features cutting-edge research on sports-related shoulder injuries, rehabilitation protocols, and outcomes critical for active populations.
- American Physical Therapy Association (APTA) – Provides clinical practice guidelines and rehabilitation techniques specific to rotator cuff tear recovery, emphasizing evidence-based therapy approaches.
Conclusion
Understanding rotator cuff tear treatment requires an integrated perspective combining precise diagnosis, individualized treatment approaches, and advanced rehabilitation techniques. Orthopedic doctors play a pivotal role in orchestrating care plans that incorporate both established modalities and innovative biologic therapies to optimize tendon healing and shoulder function. The emerging use of digital health technologies further empowers patients by enhancing engagement and monitoring adherence, ultimately improving recovery trajectories.
Patient education and lifestyle adaptations are equally vital, fostering active participation and reducing re-injury risk. Whether opting for conservative management or surgical repair, close collaboration with healthcare professionals ensures tailored strategies that address the complex biological and mechanical challenges of rotator cuff healing.
We invite you to apply these expert insights to your recovery journey, share your experiences, and explore related content to deepen your understanding. Together, we can elevate the standard of care and support for those facing rotator cuff injuries.


I appreciate the comprehensive detail this post offers about rotator cuff tear treatment and the pivotal role orthopedic doctors play in tailoring individualized care. From my own experience supporting a family member through rotator cuff surgery and rehabilitation, I can attest to how crucial early and precise diagnosis was in designing the treatment plan. The emphasis on combining conservative therapy with surgical intervention when needed really resonated with me — the non-surgical options gave my relative pain relief and improved function initially, which made surgery a more manageable prospect when it became necessary.
What struck me as particularly helpful is the focus on patient education and integrating lifestyle adjustments. Understanding the injury and the healing process empowered us to stay motivated throughout the slow phases of recovery, especially when progress felt frustratingly incremental. The mention of digital health technologies like wearable sensors also seems promising for keeping patients engaged and accountable in their home exercise routines, which I believe is often where people struggle the most.
Given these insights, I’m curious how others incorporate technology or community support in their rehab routines. Have any readers found specific apps, devices, or local groups that significantly boosted their recovery or kept them committed during tougher times? Sharing these practical tools could really offer everyone a valuable edge in their healing journey.
This post offers a very thorough overview of what to expect in rotator cuff tear treatment, which I found incredibly helpful. I had a minor tear repaired surgically last year and was surprised by the importance of the rehab phase. The part about neuromuscular re-education really resonated with me because I initially underestimated how much coordination and proprioception are involved in postoperative recovery. The tech advancements like wearable sensors sound promising—they definitely can help keep patients accountable and motivated, especially during long recovery periods.
One thing I’ve experienced is the psychological challenge during the slow recovery phases; staying patient and positive isn’t always easy. I wonder, what strategies do others use to stay motivated, especially if progress seems to plateau? Personally, setting small goals and tracking my improvements through a mobile app helped me stay engaged, but I’m curious about other effective approaches.
Also, for those considering biologic therapies like PRP or stem cells, have you encountered any compelling evidence or personal experiences that influenced your decision? It seems like a fascinating frontier in orthopedic care that could revolutionize healing outcomes.
Reading through this detailed overview, I was reminded of my own experience with rotator cuff injuries and how crucial early diagnosis really is. When I first felt persistent shoulder pain, I underestimated it, and it wasn’t until I experienced weakness or limited mobility that I sought expert help. The diagnostic process involving MRI scans and detailed examination really underscores how personalized treatment plans can be, especially when considering options like minimally invasive surgery or biologic treatments.
One aspect I’d love to hear more about from others is how they manage the psychological hurdles during recovery. It’s such a slow process, and keeping motivation high is often a challenge. I found that combining physical therapy with mental strategies like mindfulness or even talking to support groups significantly helped me stay positive.
Have any of you tried integrating newer therapies like PRP or stem cells into your recovery? There’s so much promising research, but I’m curious about real-world experiences and outcomes. It seems like a frontier with a lot of potential to improve long-term shoulder function.
This article really highlights the importance of a comprehensive and personalized approach to treating rotator cuff tears. Having gone through conservative therapy and later surgery myself, I agree that early intervention combined with tailored rehab makes a significant difference in outcomes. I was particularly interested in the discussion on biologic treatments like PRP and stem cells. While I haven’t tried them personally, I’ve read mixed reviews, and it seems that their success may depend heavily on individual factors like the extent of the tear and tissue quality. Has anyone had firsthand experience with these therapies, especially in the context of a surgical repair? Additionally, I found the section on neuromuscular re-education fascinating—it’s a reminder of how crucial proprioception and muscle coordination are in recovery. What strategies or tools have others found effective in maintaining motivation during the lengthy rehab process? I believe staying engaged and informed is key, so hearing about different experiences could really help others manage this challenging phase better.
This post really articulates the nuanced role that orthopedic doctors play in the recovery journey for rotator cuff injuries. Having personally gone through shoulder rehab after surgery, I can say that the precision in diagnosis — especially the use of MRI to assess tissue quality — makes a huge difference in planning effective treatment. I was also struck by the emphasis on voltage in neuromuscular re-education; I found that incorporating proprioceptive exercises helped me regain stability faster. It raises an interesting question: how do physical therapists customize neuromuscular training based on individual healing progress? Do any fellow readers have insights or experiences with integrating digital tools like wearable sensors into their rehab routines? I believe these innovations can really enhance engagement and monitor recovery dynamics more precisely. It’s exciting to think about how ongoing research into biologics like PRP influences personalized treatment plans. Has anyone here tried these biologic therapies, and what was your experience? Is the future of rotator cuff repair leaning more towards regenerative medicine, in your opinion?