Decoding Orthopedic Diagnosis: Why Codes Matter More Than You Think
In orthopedic medicine, precision in diagnosis is paramount—not only for effective patient care but also for seamless communication among healthcare providers, insurers, and legal entities. The orthopedic diagnosis codes common list represents a structured language that captures complex musculoskeletal conditions succinctly. Beyond mere billing, these codes embody clinical narratives essential for treatment planning and outcome tracking. This article navigates the essentials of orthopedic diagnosis codes, revealing their critical role in modern orthopedic practice.
Unveiling the Core: What Constitutes the Common Orthopedic Diagnosis Codes?
The backbone of orthopedic coding lies primarily in the International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM). Common codes encompass a wide spectrum of musculoskeletal diagnoses—from fractures (S42.2 for clavicle fracture) and sprains (S93.4 for ankle ligament sprain) to degenerative diseases like osteoarthritis (M17.11 for unilateral primary osteoarthritis of the knee). Mastery of these codes ensures clarity in documenting patients’ conditions, facilitating accurate treatment strategies and reimbursement.
How Do Orthopedic Diagnosis Codes Influence Treatment and Insurance Processes?
Orthopedic diagnosis codes play a pivotal role in bridging clinical assessment and administrative procedures. Clinicians rely on these codes to articulate the nature and severity of injuries, which directly impacts treatment pathways—from conservative management to surgical interventions. Meanwhile, insurers scrutinize these codes to validate claims, ensuring that care aligns with diagnosed conditions. For example, distinguishing between a simple rotator cuff tear and a complex labral tear via precise coding can determine eligibility for advanced therapies or surgical coverage.
Beyond the Basics: Integrating Orthopedic Codes in Clinical Documentation
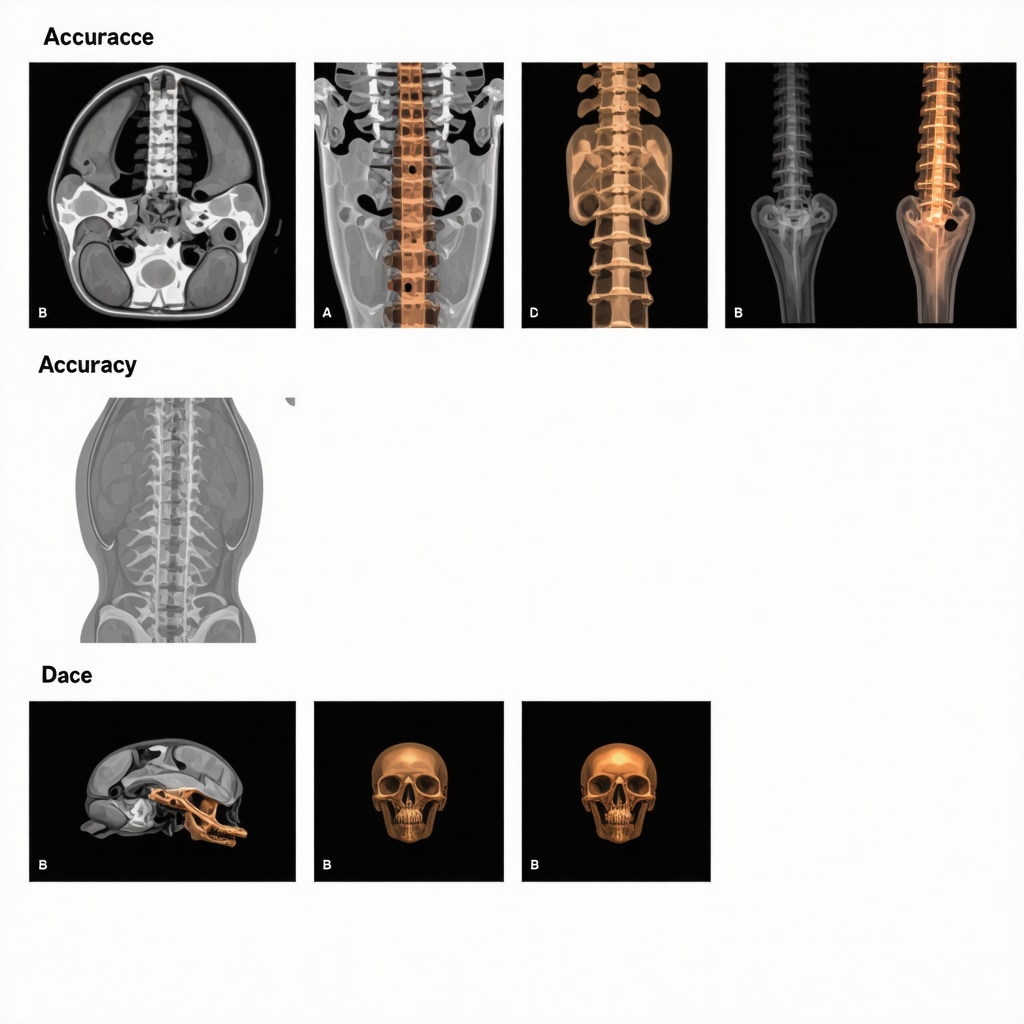
Effective orthopedic documentation transcends listing codes; it involves contextualizing diagnosis within patient history, physical findings, and imaging results. This holistic approach enhances the utility of codes in multidisciplinary care coordination. For instance, detailed documentation supporting ICD-10 code M51.26 (other intervertebral disc displacement, lumbar region) not only guides orthopedic surgeons but also informs rehabilitation specialists and pain management teams. Such integration fosters personalized care plans that address both structural pathology and functional recovery.
Expert Tips: Navigating Challenges in Orthopedic Code Selection and Updates
The dynamic nature of ICD-10-CM demands continuous education and vigilance. Orthopedic professionals must stay abreast of annual code updates and revisions that reflect emerging clinical knowledge and evolving treatment modalities. Misapplication of codes can lead to claim denials or compromised patient records. Utilizing resources like the CDC ICD-10-CM official guidelines ensures authoritative reference for accurate coding. Additionally, leveraging electronic health records with integrated coding assistance can streamline documentation and reduce errors.
Discovering the Nuance: How Does Accurate Coding Enhance Patient Outcomes?
Precise orthopedic diagnosis coding transcends administrative necessity—it directly influences patient outcomes. Accurate codes enable targeted interventions by identifying specific conditions promptly. Consider a case where early coding of a lumbar disc herniation (M51.27) facilitates timely referral to non-surgical spine care specialists, improving recovery prospects and reducing chronic pain risks. Such strategic use of codes supports evidence-based practice and optimizes resource allocation across the care continuum.
For those interested in expanding knowledge on orthopedic care strategies, exploring resources like effective non-surgical care for herniated discs can provide valuable insights.
Curious about how orthopedic diagnosis codes can impact your own practice or treatment plans? Share your thoughts or questions below and join the conversation with fellow professionals and patients navigating the complexities of orthopedic care.
Personal Reflections on the Complexity of Orthopedic Coding
When I first started working with orthopedic diagnosis codes, I was overwhelmed by the sheer volume and specificity. Each code seemed like a tiny puzzle piece, representing a unique condition or injury. Over time, I learned that these codes are far more than just administrative tools; they’re a vital language that connects all facets of patient care. For example, accurately coding a condition like a lumbar disc herniation (M51.27) not only guides the surgeon’s approach but also informs physical therapists and pain management specialists of the precise issue to address.
How Can We Make Orthopedic Coding More Accessible and Accurate in Everyday Practice?
This question often comes up during discussions with colleagues and patients alike. The answer, in my experience, lies in continuous education and leveraging technology. Electronic Health Records (EHR) systems with integrated coding assistance can be a game-changer, reducing human error and streamlining documentation. Yet, nothing replaces a solid understanding of the codes themselves and the clinical nuances they represent.
Interestingly, a study by the American Academy of Orthopaedic Surgeons highlights that improved coding accuracy correlates with better patient outcomes and more effective insurance claim processes (AAOS Coding and Billing Resources). This reinforces the importance of investing time and resources into mastering these codes, not just for compliance but for enhancing patient care quality.
Integrating Orthopedic Codes into Multidisciplinary Care
From personal experience, when orthopedic diagnosis codes are well-documented and shared across care teams, treatment becomes more cohesive. For instance, a patient diagnosed with a rotator cuff tear requires coordinated care between the orthopedic surgeon, physical therapist, and sometimes a pain specialist. Clear coding ensures everyone is literally on the same page, minimizing miscommunication and facilitating tailored treatment plans.
Moreover, when it comes to insurance, accurate coding can expedite approvals for advanced treatments or surgeries. I recall a case where precise documentation of a complex knee osteoarthritis (M17.12) diagnosis helped secure timely insurance authorization for a minimally invasive procedure, leading to a smoother recovery. For those interested in exploring minimally invasive back pain treatments, resources like this guide offer excellent insights.
Learning from Challenges: Staying Updated and Avoiding Pitfalls
Orthopedic coding is not static; annual updates reflect new discoveries and treatment approaches. I’ve seen colleagues struggle with this dynamic landscape, sometimes leading to claim denials or delayed care. One practical tip I always share is to subscribe to official update newsletters and participate in coding workshops whenever possible.
Additionally, maintaining comprehensive consultation notes that complement diagnosis codes is crucial. Detailed documentation that captures patient history, symptom progression, and imaging results enriches the coding context, supporting both clinical decisions and insurance claims. If you want to dive deeper, check out our detailed post on orthopedic consultation notes essentials.
I’d love to hear your experiences. Have you encountered challenges in orthopedic diagnosis coding? Share your stories or questions below, and let’s learn from each other’s journeys. If you’re navigating specific spine conditions, exploring expert advice from the top orthopedic spine specialists might be a helpful next step.
Mastering Complex Orthopedic Diagnosis Codes: Strategies for Precision and Clinical Depth
In the evolving landscape of orthopedic medicine, moving beyond basic coding to master the nuances of complex diagnosis codes can dramatically impact both clinical outcomes and interdisciplinary communication. For example, differentiating between various types of intervertebral disc disorders—such as M51.26 (other intervertebral disc displacement, lumbar region) versus M51.27 (other intervertebral disc displacement, lumbosacral region)—requires clinicians to integrate detailed patient history, imaging findings, and symptomatology. This precision facilitates targeted interventions, from minimally invasive procedures to specialized rehabilitation protocols.
Moreover, leveraging advanced coding techniques supports research and quality improvement initiatives by enabling granular data collection. This in turn refines evidence-based guidelines and fosters personalized patient care.
How Can Orthopedic Professionals Navigate the Increasing Complexity of ICD-10-CM Coding While Maintaining Clinical Accuracy?
To address this challenge effectively, orthopedic specialists should adopt a multi-pronged approach. First, continuous education through certified coding workshops and specialized webinars is essential to stay current with frequent updates and new code introductions. Second, collaboration with certified medical coders ensures that clinical nuances are accurately translated into codes, minimizing errors that can delay treatment or reimbursement.
Integrating clinical decision support systems (CDSS) within Electronic Health Records (EHRs) can provide real-time prompts and suggestions for appropriate codes based on entered clinical data. Such technologies not only reduce administrative burdens but also reinforce adherence to coding guidelines, as emphasized in a recent publication by the Centers for Medicare & Medicaid Services (CMS).
Harnessing Orthopedic Diagnosis Codes for Enhanced Multidisciplinary Care Coordination
The power of orthopedic diagnosis codes extends well beyond billing; they serve as a critical communication tool bridging surgeons, physiatrists, physical therapists, and pain management teams. For instance, a well-coded diagnosis of a complex rotator cuff tear (M75.121) enables therapists to tailor rehabilitation exercises specifically addressing the injury’s severity and location, optimizing recovery trajectories.
Furthermore, accurate coding facilitates the integration of orthopedic care with emerging fields like regenerative medicine and biologics. Documenting eligibility for advanced therapies hinges on precise diagnostic characterization, which in turn influences insurance authorization and patient access.
In addition, shared coding frameworks empower multidisciplinary teams to monitor patient progress and outcomes systematically, fostering data-driven adjustments to care plans. This approach is pivotal in managing chronic musculoskeletal disorders where longitudinal tracking informs treatment efficacy.
What Are the Best Practices for Ensuring Orthopedic Codes Facilitate Effective Communication Across Diverse Clinical Specialties?
Adopting standardized coding protocols paired with comprehensive documentation is paramount. Detailed consultation notes that contextualize ICD-10-CM codes with clinical findings, imaging, and patient-reported outcomes improve mutual understanding among providers. Establishing regular interdisciplinary case reviews where coded diagnoses and treatment responses are discussed can further align team strategies.
Importantly, training all team members—including non-physician providers—in the significance and interpretation of orthopedic diagnosis codes fosters a culture of precision and accountability.
Technological Innovations: Leveraging AI and Machine Learning to Revolutionize Orthopedic Coding Accuracy
Recent advancements in artificial intelligence (AI) and machine learning (ML) offer promising solutions to the complexities of orthopedic diagnosis coding. AI-powered coding assistants analyze clinical notes and imaging reports to suggest the most appropriate and specific ICD-10-CM codes, reducing human error and optimizing documentation completeness.
These technologies can also identify coding discrepancies and flag potential inconsistencies before claims submission, ensuring compliance and accelerating reimbursement cycles. According to research published in Journal of Biomedical Semantics, AI integration in medical coding enhances accuracy by up to 20%, demonstrating substantial efficiency gains.
For orthopedic practices aiming to stay at the forefront, investing in AI-driven coding tools represents not only a technological upgrade but also a strategic clinical asset.
Future Directions: Preparing for ICD-11 and the Next Generation of Orthopedic Coding
With the World Health Organization’s introduction of ICD-11, orthopedic coding is poised for a transformative leap. ICD-11 offers enhanced specificity, incorporating digital health technologies and enabling more nuanced classification of musculoskeletal disorders. Preparing for this transition involves early familiarization with new code structures and potential impacts on clinical workflows.
Engaging in pilot programs and feedback initiatives can help practices adapt smoothly and contribute to refining coding standards for orthopedic medicine globally.
Delving deeper into cutting-edge orthopedic coding strategies? Explore our upcoming series on ICD-11 implications and advanced documentation techniques to elevate your clinical practice.
Revolutionizing Orthopedic Coding with AI: Precision Meets Efficiency
In the contemporary orthopedic landscape, artificial intelligence (AI) and machine learning (ML) have emerged as transformative forces enhancing diagnostic coding accuracy. These sophisticated algorithms analyze voluminous clinical narratives and imaging data to propose the most precise ICD-10-CM codes, mitigating human error inherent in manual coding processes. Beyond mere suggestion, AI systems proactively identify inconsistencies and potential undercoding, thereby expediting claims processing and ensuring compliance with regulatory standards.
For instance, implementation of AI-driven coding assistants has demonstrated improvements in coding precision by approximately 20%, as documented in a comprehensive study published in the Journal of Biomedical Semantics. Such advancements not only streamline administrative workflows but also empower clinicians to focus more intently on patient-centric care.
How Can Orthopedic Practices Effectively Integrate AI Technologies Without Compromising Clinical Nuance?
Successful integration demands a harmonious balance between technological tools and clinical expertise. Orthopedic professionals should engage in multidisciplinary training that encompasses both AI functionalities and the subtleties of musculoskeletal pathology. Furthermore, continuous validation of AI-generated codes against expert clinical judgment ensures fidelity to patient-specific details. Strategic collaboration with IT specialists to customize AI platforms according to practice needs can optimize adoption and utility.
ICD-11: Navigating the Next Frontier in Orthopedic Diagnosis Classification
The imminent global transition to ICD-11 heralds a paradigm shift characterized by enhanced granularity and digital interoperability in orthopedic diagnosis coding. This next-generation classification system incorporates novel categories reflecting advances in musculoskeletal research and integrates with electronic health infrastructures to facilitate real-time data exchange.
Proactive preparation is essential, including immersive training on new coding architectures and participation in pilot implementation initiatives. Embracing ICD-11 promises to refine diagnostic precision, enable sophisticated epidemiological surveillance, and support personalized medicine approaches.

Strategic Recommendations: Cultivating Expertise for Future-Proof Orthopedic Coding
To adeptly navigate evolving coding standards and technological innovations, orthopedic professionals should cultivate continuous learning pathways, actively contribute to interdisciplinary coding forums, and leverage cutting-edge decision-support systems. Engaging with authoritative resources such as the Centers for Medicare & Medicaid Services (CMS) ensures adherence to best practices and regulatory updates.
By embracing these strategies, orthopedic practitioners can safeguard clinical accuracy, optimize reimbursement, and ultimately enhance patient outcomes in an increasingly complex healthcare environment.
Ready to elevate your orthopedic coding expertise and harness the power of AI and ICD-11? Connect with our expert community and access advanced resources tailored to your practice’s evolving needs.
Frequently Asked Questions (FAQ)
What are orthopedic diagnosis codes and why are they essential?
Orthopedic diagnosis codes are standardized alphanumeric codes, primarily from the ICD-10-CM system, used to classify musculoskeletal conditions. They are essential for clear clinical documentation, facilitating accurate treatment planning, insurance claims processing, and interdisciplinary communication in orthopedic care.
How do orthopedic diagnosis codes impact patient treatment outcomes?
Accurate coding enables precise identification of conditions, allowing clinicians to tailor interventions effectively. For example, differentiating between types of disc herniations or fractures ensures patients receive appropriate surgical or conservative management, improving recovery and minimizing complications.
What challenges do orthopedic professionals face when using ICD-10-CM codes?
The complexity and frequent updates of ICD-10-CM can lead to coding errors or misinterpretations. Challenges include selecting the most specific code, integrating clinical nuances into coding, and staying current with annual revisions, all of which require ongoing education and collaboration with coding specialists.
How can AI and machine learning improve orthopedic diagnosis coding?
AI-powered tools analyze clinical notes and imaging data to suggest accurate codes, reduce human errors, and identify inconsistencies before claim submission. These technologies enhance coding precision by providing real-time support and streamlining administrative workflows without compromising clinical detail.
What preparations are needed for the transition from ICD-10-CM to ICD-11 in orthopedic coding?
Practices should engage in comprehensive training on ICD-11’s new structure, participate in pilot programs, and update electronic health record systems. Early familiarization with ICD-11’s enhanced specificity and digital interoperability ensures smooth adaptation and continued clinical accuracy.
How does accurate orthopedic coding facilitate multidisciplinary care coordination?
Precise codes serve as a common language among surgeons, therapists, pain specialists, and other providers. They enable aligned treatment planning, monitoring of patient progress, and integration of advanced therapies, ensuring cohesive and patient-centered care across specialties.
What are best practices to maintain coding accuracy in everyday orthopedic practice?
Maintaining detailed documentation, continuous education, collaborating with certified coders, using clinical decision support systems, and leveraging AI tools are best practices that help uphold coding accuracy and compliance.
Can orthopedic diagnosis codes influence insurance approvals for advanced treatments?
Yes, specific and accurate codes help validate the medical necessity of treatments, facilitating timely insurance authorizations for surgeries, biologics, or minimally invasive procedures, thereby reducing delays in patient care.
How important is documentation beyond just listing the code?
Comprehensive consultation notes that contextualize diagnosis codes with patient history, clinical findings, and imaging are critical. They enrich the coding context, support medical necessity, and improve communication among care teams and insurers.
What role does continuous education play in mastering orthopedic diagnosis codes?
Continuous education ensures clinicians stay updated on coding changes, understand clinical nuances, and optimize coding accuracy, which directly impacts patient outcomes and reimbursement processes.
Trusted External Sources
- Centers for Disease Control and Prevention (CDC) ICD-10-CM Official Guidelines: Provides authoritative updates and comprehensive coding instructions essential for accurate orthopedic diagnosis classification.
- American Academy of Orthopaedic Surgeons (AAOS) Coding and Billing Resources: Offers specialized education, coding workshops, and practical tools tailored to orthopedic coding challenges and best practices.
- Centers for Medicare & Medicaid Services (CMS): Delivers regulatory guidance, coding standards, and integration recommendations crucial for compliance and reimbursement in orthopedic care.
- Journal of Biomedical Semantics: Publishes research on AI and machine learning applications in medical coding, highlighting innovations that improve accuracy and efficiency.
- World Health Organization (WHO) ICD-11 Documentation: Presents detailed information on the next-generation coding system, fostering preparation and adoption for future orthopedic coding standards.
Conclusion
Orthopedic diagnosis codes transcend administrative functions to become vital instruments for clinical precision, multidisciplinary collaboration, and optimized patient outcomes. Mastering these codes—through continuous education, embracing technological innovations like AI, and preparing for the transition to ICD-11—empowers orthopedic professionals to deliver nuanced, evidence-based care. Accurate coding ensures seamless communication across specialty teams, facilitates insurance processes, and supports the integration of emerging therapies. As the orthopedic landscape evolves, cultivating expertise in diagnosis coding is not merely a compliance requirement but a strategic imperative for enhancing care quality. Engage with our expert content, share your insights, and apply these advanced coding strategies to elevate your orthopedic practice today.


I’ve worked closely with orthopedic teams where the importance of precise diagnosis coding became glaringly evident. One challenge I’ve noticed is the frequent updates in ICD-10-CM codes, which can sometimes cause confusion, especially in busy clinical environments. The article’s point about integrating clinical notes and imaging results to contextualize codes really resonates with me — it’s not just about the code itself but the story it tells about the patient’s condition. In my experience, multidisciplinary collaboration falters without that depth, leading to misaligned treatment plans. Also, the role of AI in enhancing coding accuracy is fascinating and promising; however, I wonder how smaller clinics with limited resources can adopt such technologies effectively without overwhelming their staff. How have others balanced the need for ongoing education, technology adoption, and practical workflow constraints in maintaining coding precision? It would be great to hear different approaches, especially from those in community or outpatient settings where resources may be tighter.
Reading this comprehensive overview on orthopedic diagnosis codes really highlights how vital accurate coding is beyond just billing—it’s about truly capturing the patient’s clinical picture. I can relate personally to the complexity involved when dealing with frequent ICD-10 updates; initially, it felt overwhelming, especially without a dedicated coding team. Over time, I found that integrating regular training sessions and utilizing EHR systems with built-in coding assistance made a big difference in reducing errors and misinterpretations. Furthermore, I believe that fostering a culture of continuous learning, perhaps through quick weekly case reviews, can keep the team updated without overwhelming resources. The potential of AI tools also excites me, but I do wonder about their integration in smaller clinics where technical infrastructure may be limited. Does anyone have practical tips for implementing these technologies affordably or steps to gradually adopt them? Overall, staying updated and ensuring proper documentation seems critical—not just for reimbursement but for patient safety and care continuity.
This post really underscores how pivotal accurate orthopedic diagnosis coding is for delivering effective patient-centered care. When I started working in outpatient rehab, I quickly realized that proper coding not only helps in administrative processes but actively shapes treatment pathways. One challenge I often face is the frequent updates in ICD codes, which can cause confusion when trying to keep documentation consistent and current. I’ve found that regular team training sessions and creating quick-reference guides can go a long way in maintaining accuracy. Moreover, I’m particularly intrigued by AI’s potential in this space; it seems like a game-changer for smaller clinics that lack dedicated coding specialists. Has anyone here implemented AI tools with success? How have you integrated these technologies without disrupting your clinical workflows? I believe that fostering ongoing education combined with smart tech adoption is the way forward for us all.