The Hidden Barriers Behind Insurance Denials for Orthopedic Surgery
Orthopedic surgery can be a crucial intervention for many patients suffering from debilitating musculoskeletal conditions. Yet, it’s not uncommon to encounter insurance denials that leave patients and providers frustrated. Understanding why insurance companies may deny coverage requires a deep dive into the complexities of medical necessity, policy stipulations, and the evolving landscape of orthopedic care.
Decoding Medical Necessity: The Gatekeeper to Surgical Approval
One of the primary reasons insurance providers refuse coverage for orthopedic surgery is the question of medical necessity. Insurers require compelling evidence that surgery is essential and that alternative, less invasive treatments have been exhausted or deemed ineffective. For example, a patient with a herniated disc might first be expected to undergo comprehensive non-surgical care as outlined in effective non-surgical treatments for herniated discs before approval for surgery is granted.
What Documentation Do Insurers Expect to Justify Orthopedic Surgery?
Insurance companies often scrutinize the quality and completeness of medical records. This includes detailed orthopedic consultation notes, diagnostic imaging results, and documented trial of conservative therapies. Without thorough documentation adhering to insurance protocols, claims are vulnerable to denial. Industry experts emphasize the importance of precise coding and medical rationale to support claims, as discussed in resources like understanding orthopedic diagnosis codes.
Policy Exclusions and Coverage Limitations: Navigating the Fine Print
Beyond medical necessity, insurance policies often contain specific exclusions or limitations on certain procedures. Elective surgeries or those considered experimental may fall outside coverage. For instance, some insurers may deny coverage for newer spinal procedures until they achieve broader consensus on efficacy and safety, as detailed in expert discussions on laser spine surgery risks and benefits.
The Role of Preauthorization and Second Opinions in Avoiding Denials
Failing to obtain timely preauthorization can be a common pitfall leading to denial. Insurers typically require prior approval to ensure the planned surgery aligns with policy guidelines. Additionally, some policies mandate second opinions from board-certified orthopedic surgeons to confirm treatment necessity. Engaging with specialists early, such as those highlighted in top orthopedic spine specialists, can streamline this process.
How Can Patients Advocate for Approval When Surgery Is Denied?
When faced with a denial, patients should not lose hope. They can request a detailed explanation of the denial reason and work with their orthopedic surgeon to submit an appeal, providing supplemental documentation or alternative expert opinions. Patient advocacy and clear communication are key to navigating these challenges effectively.
Insurance denials are often a complex interplay of clinical evidence, policy details, and administrative procedures. For those interested in exploring non-surgical alternatives or understanding more about orthopedic care options, resources like effective non-surgical care for herniated discs offer valuable insights.
Curious about your specific insurance policy and orthopedic surgery coverage? Share your experiences or questions below to foster a community of informed patients and providers.
For authoritative guidance on insurance coverage criteria and medical necessity, consult the American Medical Association’s overview on medical necessity, which provides a comprehensive framework for understanding insurer decision-making.
Understanding the Appeal Process: My Personal Journey
When I faced an insurance denial for my orthopedic surgery, it felt like hitting a brick wall. But what I learned through this experience was that the appeal process is not just a bureaucratic hurdle; it’s a vital tool for patients. I remember sitting down with my orthopedic surgeon to review all the necessary documentation, including detailed consultation notes and imaging reports. We compiled evidence of how conservative treatments had failed, which proved crucial. This collaborative approach helped me draft a compelling appeal letter that ultimately led to the reversal of the denial.
From my experience, patience and persistence are key. Don’t hesitate to ask your healthcare provider for help—they understand the nuances of what insurers look for. Detailed and accurate documentation can make all the difference, especially when paired with knowledge about your insurance policy’s specific terms.
Why Do Insurance Companies Rely So Heavily on Conservative Treatment Before Surgery?
It’s natural to wonder why insurance companies require patients to try non-surgical treatments first. The reasoning, as I found through reading and discussions with medical professionals, is grounded in evidence-based practice. Conservative treatments like physical therapy, medications, and injections often effectively manage many orthopedic conditions without the risks associated with surgery.
For instance, comprehensive resources on non-surgical care for herniated discs emphasize that many patients experience significant relief without needing invasive procedures. Insurance providers want to ensure that surgery is genuinely the last resort due to its higher costs and potential complications.
Have You Ever Faced a Denial for Orthopedic Surgery? How Did You Navigate It?
I’m curious to hear your stories. Did you find success appealing a denial, or did you explore alternative treatments? Sharing real experiences helps build a supportive community, so please leave your comments below. Your insights might just provide the encouragement someone else needs to keep advocating for their health.
Staying Informed: Leveraging Trusted Medical Resources
Throughout my process, I found it invaluable to consult reputable sources to understand the criteria insurers use. The American Medical Association’s overview on medical necessity was particularly insightful. It clarified how medical necessity is defined and applied in coverage decisions, underscoring the importance of well-documented clinical justification.
Additionally, engaging with specialists who are well-versed in insurance protocols, like the top orthopedic spine specialists, can give patients a strategic advantage. These experts often help navigate preauthorization and can provide second opinions that strengthen your case.
Practical Tips for Avoiding Common Pitfalls
One mistake I noticed patients often make is skipping preauthorization or misunderstanding their policy’s nuances. Be proactive in contacting your insurance company to confirm requirements before scheduling surgery. Also, keep a detailed record of all communications with your insurer and healthcare providers.
If your surgery is denied, ask for a clear explanation in writing and review it carefully. This will guide your appeal and help you address specific insurer concerns. Remember, the goal is to demonstrate that surgery is not only necessary but also the most appropriate option given your medical history.
For more guidance on managing back pain with less invasive methods, check out effective non-surgical treatments for herniated discs. It’s a great resource to understand all possible avenues before surgery.
Leveraging Expert Opinions and Multidisciplinary Collaboration to Strengthen Insurance Appeals
When navigating the labyrinth of insurance denials, engaging a multidisciplinary team can significantly bolster your appeal. Beyond the primary orthopedic surgeon, incorporating evaluations from pain management specialists, physical therapists, and radiologists can provide a comprehensive clinical picture that insurers find harder to dispute. These expert opinions help to corroborate the necessity of surgery by demonstrating failed conservative treatments and clarifying complex diagnostic findings.
Moreover, in some cases, a peer-to-peer review between your orthopedic surgeon and the insurance company’s medical reviewer can expedite approval. This direct dialogue allows for nuanced clinical discussions that paperwork alone cannot convey. Patients should inquire proactively about this option, as it often bypasses the extended delays common in written appeals.
How Does Peer-to-Peer Review Influence Orthopedic Surgery Coverage Decisions?
Peer-to-peer (P2P) review is a critical yet underutilized mechanism in the insurance appeal process. It involves a direct conversation between the treating surgeon and an insurer’s medical reviewer, usually a board-certified physician in the relevant specialty. During this exchange, the surgeon can articulate the patient’s clinical status, response to prior treatments, and rationale for surgery in detail, addressing any ambiguities or gaps in documentation.
Research shows that P2P reviews can lead to reversal of denials in a substantial number of cases because they provide the insurer with real-time expert insight that static medical records cannot capture. According to a 2023 study published in Health Affairs, peer-to-peer reviews increased approval rates for complex surgical procedures by 25% when conducted timely and effectively (Health Affairs, 2023).
Understanding Policy Nuances: Navigating Experimental and Investigational Procedure Clauses
Insurance denials often hinge on whether a procedure is categorized as experimental or investigational. This classification can be particularly challenging in orthopedics, where innovative techniques rapidly evolve. Patients and providers must familiarize themselves with the insurer’s criteria for these designations, which typically include the procedure’s FDA approval status, availability of robust clinical trial data, and consensus within the orthopedic community.
For instance, emerging spinal procedures like minimally invasive sacroiliac joint fusion may be denied coverage under some policies despite growing evidence supporting their efficacy. Advocates can counter such denials by submitting peer-reviewed research, clinical guidelines, and expert society position statements. The National Guideline Clearinghouse and orthopedic specialty society publications are invaluable resources for this purpose.
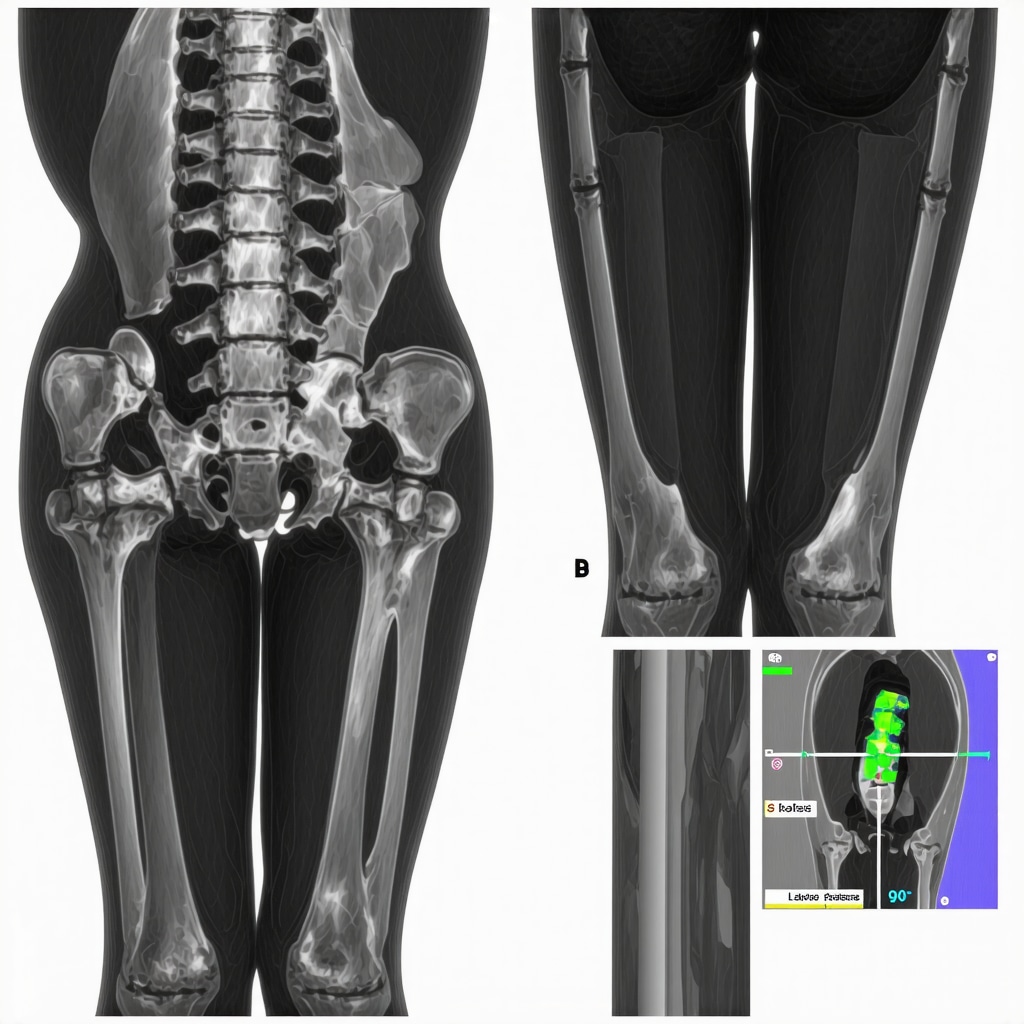
Integrating Advanced Imaging and Biomechanical Assessments to Justify Surgical Necessity
Standard imaging such as X-rays and MRIs sometimes fails to capture the functional impairment that justifies surgery. Incorporating advanced diagnostics like dynamic fluoroscopy, 3D CT reconstructions, and gait analysis can provide objective biomechanical data demonstrating instability or abnormal joint mechanics. These insights not only refine diagnosis but also strengthen the argument that conservative management is insufficient.
By presenting this sophisticated evidence, surgeons can better meet insurers’ demands for proof of medical necessity. This approach requires coordination with specialized imaging centers and may involve additional costs, yet it often proves worthwhile in avoiding denials.
Proactive Patient Engagement: Building a Robust Case from Consultation to Surgery
Patients who actively participate in their care trajectory improve their chances of insurance approval. This includes maintaining organized records of symptom progression, documenting adherence to prescribed conservative therapies, and preparing detailed questions for each clinical visit. Transparency and persistence in communication with both providers and insurers can preempt misunderstandings that lead to denials.
Additionally, seeking second opinions early—preferably from surgeons with expertise in insurance navigation—can identify potential barriers before submitting claims. These specialists often tailor documentation specifically to meet insurer criteria, streamlining preauthorization.
For patients ready to advocate more effectively, consider exploring comprehensive resources such as insurance appeal strategies for orthopedic surgery, which delve into nuanced tactics and real-world examples.
Harnessing Multidisciplinary Collaboration to Fortify Insurance Appeals
Insurance denials for orthopedic surgery often stem from fragmented clinical narratives that fail to convincingly demonstrate medical necessity. By integrating a multidisciplinary team—including orthopedic surgeons, pain management experts, radiologists, and physical therapists—patients can present a comprehensive, corroborated clinical picture. This collective expertise not only substantiates failed conservative therapies but also elucidates complex diagnostic subtleties that insurers frequently overlook.
How Does Peer-to-Peer Review Influence Orthopedic Surgery Coverage Decisions?
Peer-to-peer (P2P) reviews serve as a pivotal mechanism allowing direct dialogue between the treating orthopedic surgeon and the insurance company’s medical reviewer, typically a board-certified specialist. This interaction facilitates nuanced discourse beyond static documentation, enabling real-time clarification of clinical rationale, treatment trajectory, and patient-specific complexities. Research published in Health Affairs (2023) underscores that timely and well-executed P2P reviews can enhance surgical approval rates by approximately 25%, emphasizing their strategic value (Health Affairs, 2023).
Deciphering the Experimental and Investigational Procedure Clauses in Orthopedic Policies
One of the most intricate challenges in securing insurance coverage lies in navigating the experimental or investigational status of advanced orthopedic procedures. Insurers often rely on stringent criteria—including FDA approval, robust clinical trial data, and prevailing consensus within orthopedic subspecialties—to classify procedures. Emerging innovations, such as minimally invasive sacroiliac joint fusion, may face denials despite accumulating evidence supporting efficacy. Counteracting such denials necessitates submission of peer-reviewed clinical research, endorsements from orthopedic specialty societies, and authoritative guideline documents like those available at the National Guideline Clearinghouse.
Leveraging Advanced Imaging and Biomechanical Assessments to Substantiate Surgical Necessity
Traditional imaging modalities often provide insufficient insight into the functional impairments underpinning orthopedic pathology. Incorporating advanced diagnostics such as dynamic fluoroscopy, three-dimensional computed tomography reconstructions, and comprehensive gait analysis offers objective biomechanical evidence of joint instability or aberrant mechanics. These data not only refine the diagnostic precision but also robustly demonstrate the inadequacy of conservative management, thereby strengthening insurance appeals.
Empowering Patients Through Proactive Engagement and Documentation
Active patient participation throughout the clinical continuum significantly enhances the likelihood of insurance approval. Meticulous documentation of symptom evolution, adherence to prescribed conservative treatments, and detailed communication with healthcare providers establishes a transparent and compelling narrative. Early solicitation of second opinions, particularly from orthopedic surgeons adept in insurance protocols, can preemptively identify coverage obstacles and tailor documentation accordingly.
For those seeking an in-depth exploration of tactical approaches to insurance appeals, insurance appeal strategies for orthopedic surgery provides invaluable guidance with practical examples and nuanced insights.
Frequently Asked Questions (FAQ)
Why do insurance companies require conservative treatment before approving orthopedic surgery?
Insurers prioritize evidence-based, cost-effective care that minimizes patient risk. Conservative treatments like physical therapy, medications, and injections often resolve orthopedic issues without surgery. Requiring these first ensures surgery is truly medically necessary, reserved for cases where non-surgical options have failed or are inappropriate.
What documentation is essential to support an orthopedic surgery insurance claim?
Complete and precise medical records are critical. This includes detailed consultation notes, diagnostic imaging reports, documentation of conservative treatments attempted, and clear coding aligned with insurer protocols. Such comprehensive evidence substantiates medical necessity and aligns with insurer criteria to reduce denial risk.
How can patients effectively appeal a denied orthopedic surgery claim?
Patients should request a detailed denial explanation, collaborate closely with their orthopedic surgeon to gather supplemental documentation, and consider obtaining second opinions. Incorporating peer-reviewed research and expert society guidelines strengthens appeals. Engaging in peer-to-peer reviews with insurer medical reviewers can also enhance approval chances.
What role does peer-to-peer review play in insurance appeals?
Peer-to-peer (P2P) review allows direct communication between the treating orthopedic surgeon and the insurer’s medical reviewer. This real-time dialogue clarifies clinical rationale and addresses documentation gaps, improving understanding and often leading to reversal of denials, as supported by recent studies showing a 25% increase in approval rates when P2P is utilized effectively.
How do insurance policies define experimental or investigational procedures, and why does this matter?
Procedures lacking FDA approval, robust clinical trial data, or broad orthopedic consensus may be labeled experimental or investigational. Insurers often exclude coverage for these due to uncertain efficacy or safety. Understanding these classifications helps patients and providers submit appropriate evidence, including clinical guidelines and specialty society endorsements, to contest denials.
Can advanced imaging and biomechanical assessments influence insurance decisions?
Yes. Standard imaging might miss functional impairments justifying surgery. Advanced diagnostics such as dynamic fluoroscopy, 3D CT scans, and gait analysis provide objective biomechanical evidence of joint instability or abnormal mechanics, thereby strengthening the argument for medical necessity and increasing chances of insurance approval.
What practical steps can patients take to avoid insurance denials for orthopedic surgery?
Proactive engagement is key. Patients should verify preauthorization requirements, maintain organized records of symptoms and treatments, communicate transparently with providers and insurers, and seek early second opinions from specialists experienced in insurance navigation. Understanding policy nuances and preparing thorough documentation can preempt many common denial reasons.
How do multidisciplinary teams enhance the insurance appeal process?
Involving pain management experts, radiologists, physical therapists, and orthopedic surgeons provides a comprehensive clinical picture that corroborates failed conservative treatments and clarifies complex diagnostics. This multidisciplinary approach presents a robust, unified case that insurers find more compelling, often facilitating approval.
Are there resources patients can consult to better understand orthopedic surgery coverage?
Yes. Authoritative sources like the American Medical Association’s guidelines on medical necessity, specialty society publications, and dedicated orthopedic insurance appeal strategy resources offer valuable insights. Engaging with these materials empowers patients to navigate coverage challenges more confidently.
Trusted External Sources
- American Medical Association (AMA) – Their comprehensive overview on medical necessity provides foundational understanding of insurer decision frameworks and ethical considerations in coverage determinations (AMA Medical Necessity Overview).
- Health Affairs Journal – A leading peer-reviewed publication offering evidence-based research, including studies on peer-to-peer review effectiveness in insurance appeals, ensuring data-driven insights (Health Affairs, 2023 Study).
- National Guideline Clearinghouse – Provides authoritative clinical practice guidelines and consensus statements on orthopedic procedures like sacroiliac joint fusion, crucial for countering experimental procedure denials (NGC Guidelines).
- Specialty Orthopedic Societies – Organizations such as the American Academy of Orthopaedic Surgeons (AAOS) offer position statements, clinical practice guidelines, and expert recommendations that inform coverage criteria and support appeal documentation.
- Specialized Orthopedic Publications – Peer-reviewed journals and expert-authored resources provide nuanced insights into emerging procedures, conservative care efficacy, and diagnostic advancements, reinforcing clinical arguments for coverage.
Conclusion
Insurance denials for orthopedic surgery often reflect complex intersections of medical necessity criteria, policy limitations, and documentation rigor. Understanding these dynamics empowers patients and providers to navigate appeals strategically, leveraging comprehensive clinical evidence, multidisciplinary collaboration, and proactive communication. Advanced imaging and peer-to-peer reviews further enhance the strength of coverage requests, while familiarity with policy nuances, including experimental procedure definitions, is indispensable.
Ultimately, patient advocacy combined with expert guidance forms the cornerstone of successful insurance navigation in orthopedic care. By engaging deeply with trusted resources and employing tactical appeal strategies, individuals can overcome barriers to receive essential surgical interventions.
If you found this expert analysis helpful, please share your experiences, ask questions, or explore related authoritative content to continue building a knowledgeable and supportive community around orthopedic health and insurance advocacy.


The way insurance companies scrutinize ‘medical necessity’ when it comes to orthopedic surgery is truly a major hurdle for many patients. From what I’ve experienced with a family member, insurers place a heavy emphasis on exhausting all conservative treatments like physical therapy or injections before approving surgery. However, the challenge lies in how thoroughly and accurately the documentation is presented to justify that surgery is the next appropriate step. Missing or incomplete records can easily lead to denials, which creates additional stress on top of already difficult health issues.
I found the part about preauthorization and second opinions especially insightful. In our case, seeking a second opinion from a surgeon familiar with insurance protocols not only helped clarify the clinical necessity but also sped up the approval process. Another interesting aspect is the peer-to-peer review between the treating surgeon and insurance medical reviewers, which seems like a powerful avenue to clarify grey areas that simple paperwork can’t convey.
I wonder how often patients are made aware of these less obvious but important steps in the approval process early on? It seems like proactive education could empower more patients to navigate the system successfully. Has anyone else found that working closely with specialists knowledgeable about insurance really makes a difference in overcoming denials? I’d love to hear other experiences or tips for advocacy within this complex insurance landscape.