When Is Spine Surgery the Next Step? Inside an Orthopedic Specialist’s Decision-Making
Back pain and spinal issues are among the most common reasons patients seek orthopedic care, but determining when to escalate treatment to spine surgery is a nuanced process that combines clinical expertise with patient-centered judgment. Orthopedic specialists weigh many factors before recommending surgical intervention, aiming always to balance risks, benefits, and the individual’s quality of life. Understanding these signs can empower patients to engage proactively in their care journey.
Decoding Persistent Symptoms: When Conservative Care Falls Short
One of the most telling indicators for considering spine surgery is the persistence or worsening of symptoms despite comprehensive non-surgical treatments. Patients who undergo rigorous physical therapy, medication management, and minimally invasive procedures but still experience debilitating pain, neurological deficits, or functional impairment may be candidates for surgical evaluation. For instance, a patient with a herniated disc causing severe leg weakness after months of conservative care demonstrates a clinical scenario where surgery might be the prudent next step. This aligns with expert recommendations found in effective non-surgical care protocols that emphasize surgery as a last resort when conservative options prove ineffective.
Neurological Red Flags: Signs That Demand Immediate Attention
Orthopedic specialists vigilantly assess for neurological red flags that signify potential spinal cord or nerve root compromise. Symptoms such as progressive muscle weakness, numbness, loss of bowel or bladder control, or severe sciatica pain that does not respond to treatment necessitate urgent surgical consultation. These signs often indicate conditions like spinal stenosis, cauda equina syndrome, or severe nerve compression where timely surgery can prevent irreversible damage. Recognizing these warning signs early is critical for optimal outcomes.
How Do Orthopedic Experts Differentiate Between Surgery and Non-Surgical Treatments for Spine Issues?
Orthopedic experts utilize a multifaceted approach combining clinical assessment, imaging studies, and patient history to determine the appropriateness of surgery. Key factors include the severity and duration of symptoms, the degree of structural abnormalities on MRI or CT scans, and the patient’s overall health status and lifestyle goals. For example, degenerative disc disease might be managed conservatively for years, whereas a traumatic spinal fracture with instability often requires prompt surgical stabilization. Decisions are personalized, often involving multidisciplinary teams to ensure comprehensive care. For deeper insight, readers may explore when to escalate to a spine surgeon, which delves into specific clinical criteria guiding surgery referrals.
Patient Stories Illuminate the Path: Real-World Cases of Escalation to Surgery
Consider the case of a 52-year-old patient with chronic lumbar pain that progressively limited mobility and daily function. After exhaustive physical therapy and injections failed, worsening numbness and weakness prompted surgical evaluation. Post-surgery, the patient regained significant function and pain relief, underscoring the critical role of timely surgical intervention. Such examples add experiential depth to clinical guidelines, illustrating how individualized care decisions translate into improved quality of life.
Beyond Surgery: The Role of Ongoing Orthopedic Care and Rehabilitation
Escalating to spine surgery is not an isolated event but part of an integrated care continuum. Postoperative rehabilitation, bracing, and lifestyle modifications are essential to sustain surgical benefits and prevent recurrence. Orthopedic teams emphasize patient education and long-term management strategies to optimize spine health. For those interested, resources like orthopedic rehab tips after lumbar fusion surgery offer valuable guidance on recovery.
Understanding when to escalate to spine surgery can feel daunting, but informed patients equipped with expert insights and clear warning signs can navigate their care with confidence. Feel free to share your experiences or questions in the comments below — your story might help others facing similar decisions.
For authoritative clinical guidelines on surgical indications for spine disorders, the North American Spine Society (NASS) provides comprehensive resources at spine.org, a trusted source for both patients and clinicians.
Listening to Your Body: The Subtle Signs That Might Be Overlooked
In my experience working closely with patients and specialists, I’ve learned that sometimes the most critical indicators for escalating to spine surgery aren’t the dramatic ones like sudden loss of mobility, but rather the subtle, persistent changes that can easily be dismissed. For example, a patient might report a gradual decrease in their ability to perform everyday tasks or notice a creeping discomfort that doesn’t quite reach severe pain levels but steadily worsens. These nuances often require a keen eye and attentive listening from orthopedic specialists to catch early. It reminds me how vital open communication and thorough documentation are during consultations — elements that can significantly influence treatment pathways.
Balancing Risks and Rewards: Personalizing Surgical Decisions
One of the most challenging aspects I’ve observed in orthopedic care is balancing the potential benefits of surgery against the risks, especially with spine operations that can be complex. Age, overall health, lifestyle demands, and even psychological readiness play essential roles. I recall a patient in their sixties who was hesitant about surgery despite clear indications. We explored conservative options longer and incorporated a multidisciplinary approach including physical therapy and pain management. However, when neurological symptoms progressed, surgery became unavoidable. The successful outcome reaffirmed that timing and patient readiness are as crucial as the clinical indications themselves.
What Are the Latest Advances in Minimally Invasive Spine Surgery That Could Influence Treatment Choices?
It’s fascinating to see how technological advancements have reshaped the landscape of spine surgery. Minimally invasive techniques now allow for reduced recovery times, less postoperative pain, and lower infection risks, making surgery a more accessible option for patients who might have been wary before. According to recent studies highlighted by the North American Spine Society, these techniques continue to evolve with better imaging and surgical tools enhancing precision. This progress means that patients and doctors can often consider surgery earlier with greater confidence in outcomes, especially when conservative treatments don’t suffice.
Integrating Holistic Orthopedic Care: Beyond the Operating Table
Another insight I’ve gained is the importance of integrating holistic care approaches alongside surgical planning. This includes nutrition, mental health support, tailored physical therapy, and ergonomic adjustments in daily life. For instance, patients recovering from spine surgery benefit enormously from education on posture and activity modification to sustain improvements. If you’re interested in learning more about post-surgical rehabilitation, check out orthopedic rehab tips after lumbar fusion surgery for practical advice.
Have you or someone you know faced the tough choice between continuing conservative care and opting for spine surgery? What factors influenced your decision? Sharing your story in the comments can provide invaluable support and perspective to others navigating this path. And if you want to dive deeper into understanding when to consult a spine surgeon, consider exploring this detailed guide that breaks down key warning signs and decision-making criteria.
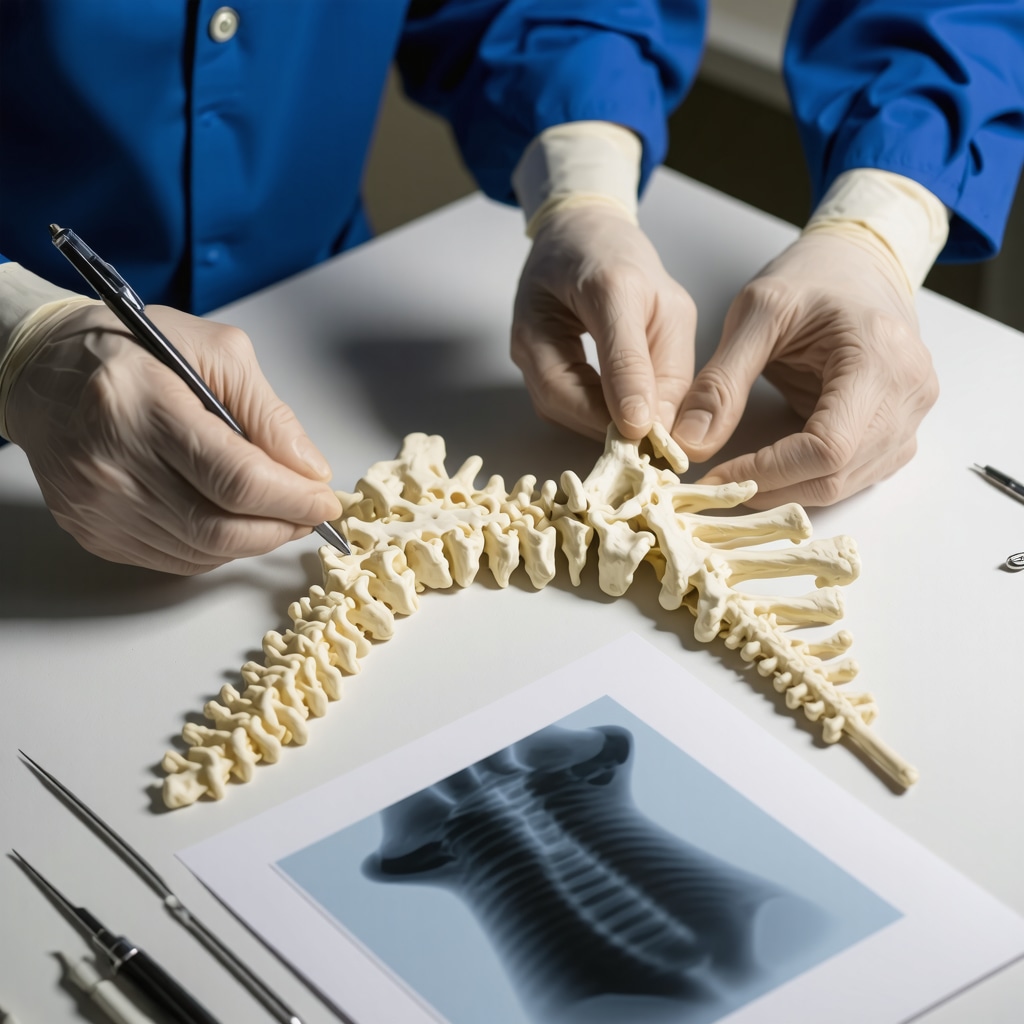
Biomechanical Complexities and Their Role in Surgical Decision-Making for Spinal Disorders
Understanding the intricate biomechanics of the spine is paramount in discerning when surgical intervention is warranted. The spine is a dynamic structure, balancing flexibility and stability through intervertebral discs, facet joints, ligaments, and musculature. Degenerative changes disrupt this harmony, leading to altered load distribution and abnormal motion patterns. Orthopedic specialists incorporate advanced biomechanical assessments—such as dynamic flexion-extension radiographs and motion-preserving imaging techniques—to evaluate instability or aberrant kinematics that conservative treatments cannot address effectively. For example, segmental instability identified on imaging, coupled with persistent neurologic symptoms, often tips the scale towards surgical stabilization to restore biomechanical integrity and prevent progressive deformity.
Integrating Advanced Imaging Modalities: Beyond Conventional MRI and CT in Surgical Planning
While MRI and CT scans remain foundational, cutting-edge imaging technologies offer nuanced insights that refine surgical candidacy. Diffusion tensor imaging (DTI) and functional MRI (fMRI) provide detailed visualization of spinal cord microstructure and neural pathways, revealing subtle nerve fiber disruptions not apparent on standard imaging. In complex cases involving spinal cord compression or myelopathy, these modalities assist surgeons in prognosticating outcomes and tailoring interventions to minimize neurological compromise. Additionally, intraoperative navigation systems leveraging 3D imaging enhance precision during minimally invasive procedures, reducing operative morbidity. Such technological integration underscores the evolving paradigm where imaging guides not only diagnosis but also personalized surgical strategy.
How Do Emerging Neurophysiological Monitoring Techniques Influence Intraoperative Spine Surgery Decisions?
Intraoperative neurophysiological monitoring (IONM) has become an indispensable tool during spine surgeries, providing real-time feedback on the functional integrity of neural elements. Techniques such as somatosensory evoked potentials (SSEPs), motor evoked potentials (MEPs), and electromyography (EMG) enable immediate detection of potential nerve injury, allowing surgeons to modify their approach dynamically. This is especially critical in deformity corrections and tumor resections where the risk to neural structures is heightened. Recent advances in IONM involve multimodal monitoring and integration with robotic-assisted systems, enhancing safety profiles and expanding the scope of operable pathologies. According to the latest guidelines from the American Clinical Neurophysiology Society, IONM significantly reduces postoperative neurological deficits and improves patient outcomes.[1]
Personalized Risk Stratification Models: Predicting Surgical Outcomes Through Data-Driven Approaches
The decision to proceed with spine surgery increasingly leverages predictive analytics and personalized risk stratification models. By incorporating patient-specific variables—such as age, comorbidities, bone density, smoking status, and psychosocial factors—these models forecast surgical risks like infection, non-union, or prolonged recovery. Machine learning algorithms trained on large datasets enhance accuracy, allowing surgeons to counsel patients regarding expected benefits and complications tailored to their unique profile. Such precision medicine approaches optimize shared decision-making and resource allocation, reducing unnecessary surgeries and improving satisfaction rates. Institutions pioneering these models report improved adherence to evidence-based indications and better alignment with patient goals.
Multidisciplinary Collaboration: The Keystone of Complex Spine Surgery Decision-Making
Complex spinal pathologies often demand a multidisciplinary approach that transcends the orthopedic surgeon alone. Collaboration with neurosurgeons, pain management specialists, physiatrists, and physical therapists ensures comprehensive evaluation of each case. This team-based model facilitates the integration of diverse expertise—from advanced imaging interpretation to rehabilitation strategies—maximizing patient-centered care. Multidisciplinary conferences and case reviews foster consensus on surgical timing and technique, balancing aggressive intervention against conservative management. This holistic approach has been shown to reduce complication rates and enhance functional recovery in challenging spine disorders, emphasizing that surgery is but one component of a broader therapeutic continuum.
For clinicians and patients eager to explore the frontier of spine surgery decision-making, continuous education and engagement with expert resources are vital. Dive deeper into the nuances of surgical indications and innovations by visiting the North American Spine Society, where cutting-edge research and clinical guidelines converge.
Expanding the Horizon: Biomechanical Insights Shaping Surgical Indications
Diving deeper into spinal pathophysiology reveals that the spine’s complex biomechanics—encompassing the interplay between vertebral alignment, intervertebral disc integrity, and muscular support—play a pivotal role in determining surgical necessity. Orthopedic specialists increasingly rely on dynamic assessments such as flexion-extension radiographs and kinematic MRI to detect subtle instabilities or aberrant motion patterns that static imaging might miss. These biomechanical nuances inform whether conservative management remains viable or if surgical stabilization is imperative to halt progressive deformity and neurological deterioration.
Revolutionizing Diagnostic Precision: Next-Generation Imaging Techniques
While traditional MRI and CT scans remain foundational, the advent of advanced imaging modalities such as diffusion tensor imaging (DTI) and functional MRI (fMRI) has transformed preoperative evaluation. These technologies provide unparalleled visualization of spinal cord microarchitecture and neural tract integrity, enabling detection of early nerve fiber compromise absent on conventional scans. Additionally, intraoperative 3D navigation systems integrate these imaging advances, offering surgeons real-time guidance to enhance precision, minimize tissue disruption, and optimize outcomes.
How Do Emerging Neurophysiological Monitoring Techniques Influence Intraoperative Spine Surgery Decisions?
Intraoperative neurophysiological monitoring (IONM) has become an indispensable adjunct in spine surgery, delivering continuous, real-time assessment of neural function. Techniques such as somatosensory evoked potentials (SSEPs), motor evoked potentials (MEPs), and electromyography (EMG) empower surgeons to identify and mitigate neural compromise intraoperatively. Especially in complex deformity corrections or tumor resections, multimodal IONM integration with robotic-assisted surgery systems enhances safety by dynamically adapting surgical maneuvers to preserve neurological integrity. The American Clinical Neurophysiology Society’s guidelines affirm that IONM significantly reduces postoperative deficits, underscoring its critical role in modern spine surgery.[1]
Data-Driven Personalization: Leveraging Predictive Analytics for Risk Stratification
The paradigm of spine surgery decision-making is increasingly informed by sophisticated predictive models that synthesize multifactorial patient data—ranging from demographic parameters to psychosocial variables—to forecast individual surgical risks and outcomes. Machine learning algorithms trained on extensive clinical datasets enable nuanced stratification, facilitating tailored counseling and shared decision-making. This precision medicine approach optimizes resource utilization, minimizes unwarranted surgical interventions, and enhances postoperative satisfaction by aligning treatment strategies with personalized risk–benefit profiles.
Collaborative Excellence: Multidisciplinary Integration in Complex Spine Care
Complex spinal disorders necessitate a cohesive multidisciplinary framework that synergizes expertise across orthopedic surgeons, neurosurgeons, pain specialists, physiatrists, and rehabilitation therapists. Regular interdisciplinary case reviews and collaborative planning optimize surgical timing, technique selection, and postoperative management. This integrated model not only refines patient-centered care but also demonstrably reduces complication rates and fosters superior functional recovery, reaffirming that effective spine surgery transcends the operating room.
For authoritative guidance and the latest advancements in spine surgery decision-making, the North American Spine Society remains an invaluable resource. Engage with these insights and contribute your questions or experiences in the comments to enrich this evolving conversation.
Frequently Asked Questions (FAQ)
What are the primary indicators that conservative treatment for spine issues has failed?
Conservative treatment is considered unsuccessful when patients experience persistent or worsening pain, neurological deficits such as muscle weakness or numbness, or functional impairment despite rigorous physical therapy, medications, and minimally invasive interventions. When these symptoms continue beyond an expected timeframe—typically several months—and significantly impact quality of life, surgical evaluation may be warranted.
How do orthopedic specialists determine if spine surgery is necessary?
Orthopedic specialists integrate clinical examination, patient history, and advanced imaging modalities like MRI, CT, and dynamic studies to assess structural abnormalities and neurological involvement. They consider symptom severity, duration, biomechanical instability, and patient-specific factors such as age and comorbidities. Multidisciplinary collaboration further refines surgical candidacy to ensure personalized, evidence-based decisions.
What neurological signs require urgent surgical consultation?
Neurological red flags include progressive muscle weakness, numbness, loss of bowel or bladder control, and severe unrelenting sciatica. These symptoms may indicate critical conditions like spinal cord compression or cauda equina syndrome where timely surgery is essential to prevent permanent damage.
How have minimally invasive techniques changed spine surgery decision-making?
Minimally invasive spine surgery offers reduced recovery times, decreased postoperative pain, and lower complication rates. These advances have expanded surgical options to patients previously deemed high-risk or hesitant, enabling earlier intervention with improved safety and outcomes.
What role do advanced imaging technologies play in surgical planning?
Advanced modalities such as diffusion tensor imaging (DTI) and functional MRI (fMRI) provide detailed visualization of neural microstructure and pathways, detecting subtle nerve fiber injuries invisible on standard imaging. This allows for more precise surgical targeting and prognostication, optimizing patient outcomes.
How does intraoperative neurophysiological monitoring improve spine surgery safety?
Intraoperative neurophysiological monitoring (IONM) offers real-time assessment of neural function during surgery, allowing immediate detection and prevention of nerve injury. Techniques like SSEPs, MEPs, and EMG help surgeons adjust their approach dynamically, reducing postoperative neurological complications significantly.
Can predictive analytics influence surgical decision-making?
Yes, personalized risk stratification models incorporating clinical, demographic, and psychosocial data forecast surgical risks and outcomes. Machine learning algorithms assist surgeons and patients in shared decision-making by identifying those most likely to benefit from surgery while minimizing unnecessary interventions.
Why is a multidisciplinary approach important in complex spine cases?
Complex spinal pathologies benefit from coordinated care involving orthopedic surgeons, neurosurgeons, pain specialists, physiatrists, and therapists. This team-based strategy ensures comprehensive evaluation, consensus on optimal timing and methods, and holistic postoperative management, improving functional recovery and reducing complications.
What subtle symptoms might indicate the need for surgery that patients often overlook?
Gradual declines in functional ability, creeping discomfort without acute severe pain, or subtle neurological changes can signal progressive spinal pathology. Attentive clinical assessment and open patient communication are essential to detect these nuances early and consider surgical options before irreversible damage occurs.
How important is postoperative rehabilitation after spine surgery?
Postoperative rehabilitation is critical to sustain surgical benefits, enhance recovery, and prevent recurrence. Tailored physical therapy, ergonomic education, and lifestyle modifications complement surgical intervention, ensuring long-term spine health and improved quality of life.
Trusted External Sources
- North American Spine Society (NASS) – spine.org: The premier professional society providing up-to-date clinical guidelines, research, and educational resources on spine disorders and surgical indications.
- American Clinical Neurophysiology Society (ACNS) – IONM Practice Guidelines: Authoritative guidelines on intraoperative neurophysiological monitoring techniques critical to enhancing surgical safety and outcomes.
- Journal of Orthopaedic & Sports Physical Therapy (JOSPT): Offers peer-reviewed research on conservative and postoperative rehabilitation strategies supporting orthopedic spine care.
- Spine Journal: A leading publication featuring high-impact studies on spinal biomechanics, surgical innovations, and predictive analytics shaping modern spine care.
- American Academy of Orthopaedic Surgeons (AAOS): Provides comprehensive patient and clinician resources on indications, risks, and advances in spine surgery and orthopedic care.
Conclusion
Deciding when to escalate to spine surgery requires a sophisticated balance of clinical insight, advanced diagnostics, and patient-centered considerations. Persistent symptoms unresponsive to conservative care, neurological red flags, and biomechanical instability often signal the need for surgical intervention. Innovations in minimally invasive techniques, neurophysiological monitoring, and predictive analytics have revolutionized decision-making, enabling safer, more personalized treatment pathways. Multidisciplinary collaboration and comprehensive postoperative rehabilitation further enhance outcomes, underscoring that surgery is one pivotal component within an integrated care continuum. By understanding these nuanced indicators and leveraging expert resources, patients and clinicians can navigate spine health decisions confidently and collaboratively. We encourage readers to share their experiences, ask questions, and explore related expert content to deepen their knowledge and empower informed choices about spine surgery and orthopedic care.

This post provides an excellent overview of the delicate balance orthopedic specialists must maintain when deciding to recommend spine surgery. From my own experience supporting a family member through chronic spinal issues, I’ve seen firsthand how the persistence of symptoms despite rigorous conservative care signals a critical juncture. What stood out to me was the emphasis on neurological red flags like progressive weakness or loss of bladder control—they’re not just warning signs but urgent calls for action. I also appreciate the discussion about how advances in minimally invasive techniques have shifted the threshold for surgery, making it a more viable option earlier in treatment for some patients. However, one challenge I’ve noticed is the patient’s psychological readiness and fear of surgery often delaying necessary intervention, even when clinical indicators suggest surgery could significantly improve quality of life. I’m curious how others have navigated this emotional aspect—does anyone have strategies or experiences where multidisciplinary support helped overcome hesitation and prepare mentally for surgery? It’s clear that surgery is just one piece of a larger, ongoing orthopedic care plan, and understanding these nuances is empowering for patients facing such tough decisions.