When Your Neck Needs a Specialist: A Tale of Twists, Turns, and Treatments
Ever woken up with that stubborn neck pain that refuses to quit, no matter how many times you stretch or sip your morning coffee? You’re not alone. The cervical spine—the neck region—is a marvel of engineering, yet prone to all sorts of misadventures. Enter the cervical spine treatment specialist, the superhero in scrubs who transforms neck woes into stories of recovery. But what exactly happens when you step into their office? Buckle up; let’s unravel the journey together.
More Than Just a Chiropractor: Who Is This Specialist, Anyway?
While the word “specialist” might conjure images of white coats and complex machines, a cervical spine treatment specialist is often an orthopedic surgeon, neurologist, or a physical therapist with a laser-like focus on neck issues. These pros don’t just throw a band-aid on your pain; they investigate the root cause—be it herniated discs, pinched nerves, or degenerative changes—and tailor a treatment plan that fits like a bespoke suit. If you’re curious about selecting the right expert, you might want to peek at how to choose the right orthopedic surgeon for your spine.
Is It Just a Pain in the Neck, or Something More Serious?
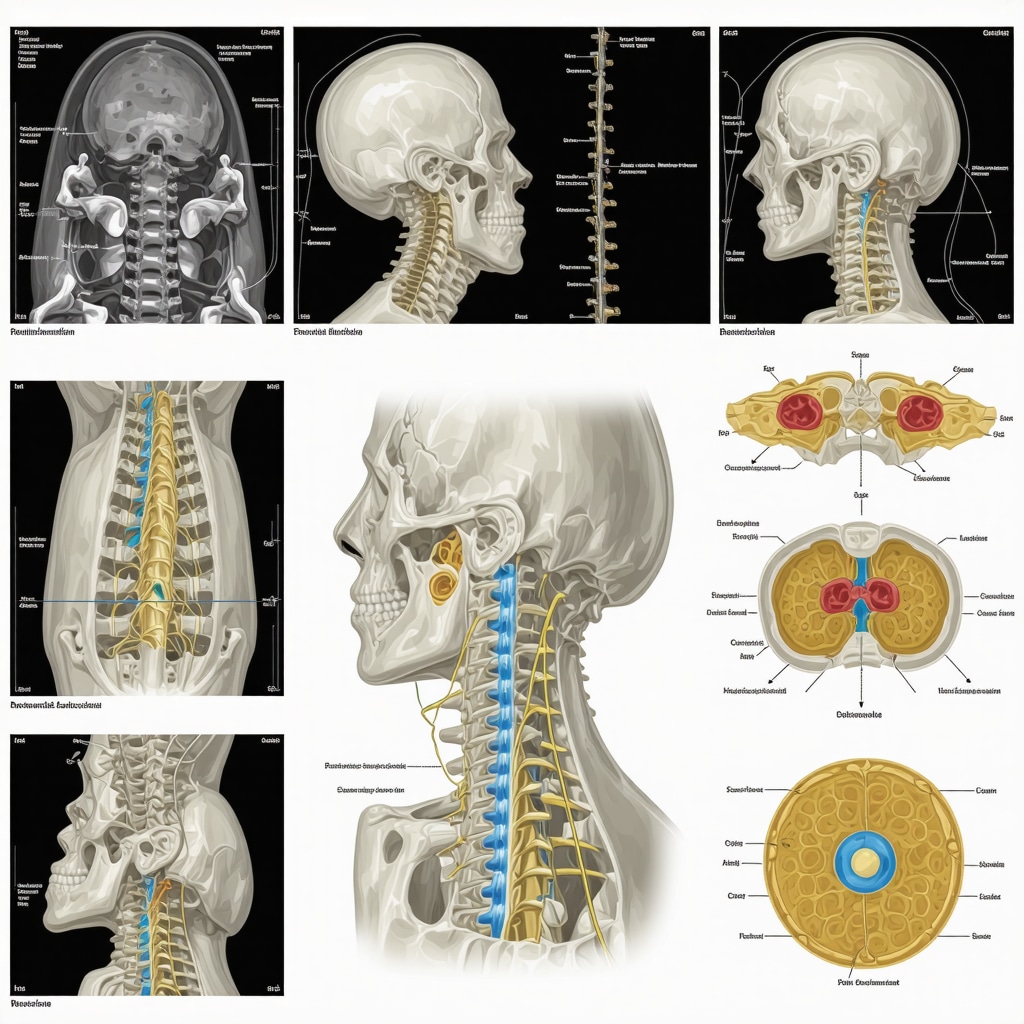
This question is the million-dollar inquiry. Neck pain is often shrugged off as a minor nuisance, but persistent or radiating pain could be a red flag. Specialists will typically run through a gamut of diagnostic tests—X-rays, MRIs, or nerve conduction studies—to get to the bottom of your discomfort. The key is not to wait for the pain to become unbearable. According to a study published in the National Library of Medicine, early intervention in cervical spine disorders significantly improves outcomes.
What Happens During Your First Visit? Spoiler: It’s Not Just Small Talk
Your initial appointment is akin to a detective story. The specialist will delve into your medical history, lifestyle, and symptoms with Sherlock-level attention. They’ll perform physical exams to assess your neck’s range of motion, strength, and reflexes. This isn’t a mere formality—it’s crucial groundwork that informs your entire treatment journey.
From Therapy to Surgery: The Spectrum of Care You Might Encounter
Not every neck problem calls for a scalpel. Many patients find relief through conservative treatments such as physical therapy, cervical traction, or even innovative non-invasive spinal decompression techniques. For those with stubborn issues, minimally invasive spine surgery might be on the table—an option that promises less downtime and quicker recovery (check out what patients should know about minimally invasive spine surgery). The cervical spine treatment specialist guides you through these options with a mix of science and empathy.
Curious about the finer details of non-surgical care? Explore effective non-surgical care for herniated discs to understand alternative paths to relief.
Why Trusting Your Neck to a Specialist Changes the Game
Neck pain is tricky; it can masquerade as something simple but hide complex underlying issues. Specialists bring a treasure trove of experience and up-to-date knowledge to the table, ensuring you’re not just another appointment on the calendar but a partner in your healing journey. Their expertise transforms uncertainty into a clear roadmap towards recovery.
So, if you’re wrestling with neck discomfort that doesn’t quit, why not share your story or ask questions? Drop a comment below or connect with a trusted expert to start your path to relief.
Integrating Multidisciplinary Care for Complex Cervical Conditions
One of the most effective approaches in modern cervical spine treatment involves a multidisciplinary care model, where orthopedic surgeons, physical therapists, pain management specialists, and neurologists collaborate closely. This integrated strategy ensures that patients receive comprehensive assessment and tailored interventions that address not only the mechanical aspects of neck pain but also the neurological and functional impairments accompanying it. For patients navigating complex cases, such a model often results in improved recovery trajectories and reduced risk of recurrent symptoms.
Clinical evidence supports the benefits of this approach; according to a review by the American Academy of Orthopaedic Surgeons (AAOS), multidisciplinary care optimizes outcomes by combining surgical precision with rehabilitative expertise and pain control modalities (AAOS, 2023). This synergy is especially valuable for patients with challenging diagnoses such as cervical radiculopathy or myelopathy, where layered treatment plans can adapt dynamically to a patient’s response.
Emerging Technologies Shaping the Future of Cervical Spine Treatment
The landscape of cervical spine care is evolving rapidly with the advent of minimally invasive techniques, robotic-assisted surgeries, and enhanced imaging modalities. These innovations aim to reduce operative trauma, shorten recovery periods, and improve surgical accuracy. For instance, advances in intraoperative navigation enable surgeons to precisely target affected vertebrae while preserving surrounding healthy tissues.
Furthermore, regenerative medicine applications such as platelet-rich plasma (PRP) injections and stem cell therapies are gaining traction as adjuncts or alternatives to traditional surgical interventions. While still under investigation, early clinical trials suggest promising potential for these biologics in promoting tissue healing and modulating inflammation in cervical disc pathology.
How Can Patients Evaluate When to Transition from Conservative to Surgical Treatment?
Determining the optimal timing for surgery remains one of the most nuanced decisions in cervical spine management. While conservative measures—such as physical therapy, cervical traction, and non-invasive spinal decompression—are the frontline treatments, persistent or worsening neurological deficits may necessitate surgical consultation.
Orthopedic specialists often assess factors including pain severity, functional impairment, imaging findings, and response to non-surgical care when advising patients. The goal is to balance risks and benefits, ensuring surgery is reserved for cases where structural correction can provide meaningful symptomatic relief and prevent long-term disability.
Patients interested in understanding this decision-making process further can explore resources like minimally invasive back pain treatments explained for a clearer picture of contemporary surgical indications and recovery expectations.
Emphasizing Patient Empowerment Through Education and Communication
Another critical dimension of successful cervical spine treatment is fostering patient engagement. Specialists emphasize transparent communication, enabling patients to comprehend their diagnosis, treatment options, and expected outcomes. This empowerment facilitates shared decision-making, adherence to therapeutic regimens, and ultimately, better health results.
Whether navigating the complexities of selecting a cervical spine surgeon or weighing the merits of emerging therapies, informed patients are better equipped to advocate for their care. Inviting dialogue—be it through questions during consultations or sharing experiences in supportive communities—enhances the healing journey.
If you have insights or experiences related to cervical spine treatment, we encourage you to comment below and join the conversation. For those seeking expert guidance, consider visiting our contact page to connect with leading specialists dedicated to your spinal health.
Precision Diagnostics: Beyond the Basics in Cervical Spine Evaluation
When standard imaging tools like X-rays and MRIs don’t fully capture the complexity of a patient’s cervical condition, specialists turn to advanced diagnostics such as dynamic fluoroscopy and high-resolution diffusion tensor imaging (DTI). These modalities provide real-time visualization of vertebral motion and nerve tract integrity, respectively, offering nuanced data crucial for tailoring treatment strategies in cases where subtle instability or nerve compromise is suspected.
Additionally, electrophysiological studies like electromyography (EMG) and somatosensory evoked potentials (SSEPs) help quantify neural function, guiding decisions about the urgency and type of intervention. This comprehensive diagnostic approach exemplifies the specialist’s commitment to precision medicine, ensuring that no detail is overlooked in pursuit of optimal patient outcomes.
What Are the Emerging Biomarkers and Imaging Techniques That Could Revolutionize Cervical Spine Treatment?
Emerging research highlights several promising biomarkers detectable in blood and cerebrospinal fluid that may predict disease progression in degenerative cervical myelopathy and disc degeneration. Concurrently, ultra-high-field MRI systems (7 Tesla and above) offer unprecedented spatial resolution, enabling visualization of microstructural changes in spinal cord tissue previously invisible to conventional scanners.
These innovations, though still primarily in research settings, hold the potential to transform early diagnosis and personalized therapies. For an in-depth review of these advances, see the recent article published in The Spine Journal.
Integrating Biologics and Rehabilitation: Crafting Synergistic Treatment Protocols
Modern cervical spine treatment increasingly embraces the synergy between biologic therapies and rehabilitative protocols. For instance, platelet-rich plasma (PRP) injections administered alongside targeted physical therapy can potentiate soft tissue healing and functional restoration, particularly in chronic tendon and ligament injuries associated with cervical instability.
Moreover, regenerative strategies are being refined to integrate with neurorehabilitation techniques that harness neuroplasticity. Combining stem cell therapies with advanced neuromuscular electrical stimulation (NMES) or virtual reality-assisted exercises aims to enhance motor recovery in patients with cervical spinal cord injury or myelopathy. This interdisciplinary melding of biologics and rehabilitation represents a frontier in patient-centered care that prioritizes restoring quality of life alongside symptom management.
Patient-Centered Decision Making: Navigating Complex Choices in Cervical Care
In the labyrinth of cervical spine treatment options, patient values, lifestyle, and risk tolerance are key compass points guiding therapeutic decisions. Specialists employ shared decision-making frameworks supported by decision aids that elucidate the benefits and potential complications of surgeries, conservative therapies, and emerging treatments.
This approach not only respects patient autonomy but also improves adherence and satisfaction. Understanding that the “right” treatment varies individually, experts facilitate nuanced discussions about expected recovery timelines, potential impacts on vocation and daily activities, and long-term prognosis.
Understanding the Role of Psychosocial Factors in Cervical Spine Recovery
Increasing evidence underscores the influence of psychosocial elements—such as anxiety, depression, and social support—on cervical spine treatment outcomes. Specialists often incorporate psychological screening and cognitive-behavioral therapy referrals into comprehensive care plans, recognizing that mental health substantially affects pain perception, rehabilitation engagement, and overall recovery trajectories.
Addressing these dimensions holistically aligns with the biopsychosocial model, promoting resilience and functional restoration beyond mere symptom alleviation. For clinicians, this means integrating mental health professionals into multidisciplinary teams and tailoring communication strategies to foster trust and motivation.
By acknowledging the mind-body interplay, cervical spine specialists elevate the standard of care from mechanical correction to genuine healing.
Beyond the Scalpel: How Precision Diagnostics Elevate Cervical Spine Treatment
In the intricate world of cervical spine disorders, standard imaging is sometimes just the starting point. Specialists now leverage advanced diagnostics like dynamic fluoroscopy and high-resolution diffusion tensor imaging (DTI) to capture subtle instabilities and nerve tract integrity that traditional MRIs might miss. These tools provide a real-time, multidimensional perspective, allowing orthopedic surgeons and neurologists to craft treatment plans with surgical precision and confidence. Complementing imaging, electrophysiological studies such as electromyography (EMG) and somatosensory evoked potentials (SSEPs) quantify nerve function, guiding intervention timing and modality. This level of diagnostic nuance underscores the commitment to personalized medicine, ensuring patients experience optimal outcomes tailored to their unique cervical pathology.
How Are Emerging Biomarkers Revolutionizing Cervical Spine Disease Management?
Cutting-edge research is spotlighting biomarkers detectable in blood and cerebrospinal fluid that predict progression in conditions like degenerative cervical myelopathy and disc degeneration. Paired with ultra-high-field MRI technology—such as 7 Tesla scanners—clinicians can visualize microstructural spinal cord changes with unprecedented clarity. These breakthroughs promise earlier detection and stratified treatment approaches, potentially transforming care paradigms. For the curious, a recent Spine Journal article offers an in-depth exploration of these innovations.
Psychosocial Dynamics: The Hidden Influencers in Cervical Spine Recovery
Neck pain is not merely a mechanical issue; its trajectory is profoundly influenced by psychosocial factors such as anxiety, depression, and social support systems. Specialists increasingly integrate psychological screening and cognitive-behavioral therapy (CBT) referrals into their care models, recognizing the biopsychosocial interplay that shapes pain perception and rehabilitation engagement. This holistic approach fosters resilience, boosts patient motivation, and often accelerates functional restoration. Such integration exemplifies modern cervical spine care’s evolution from symptom management to comprehensive healing.
Synergizing Biologics and Rehabilitation: Next-Level Cervical Spine Protocols
Combining biologic treatments like platelet-rich plasma (PRP) injections with targeted physical therapy exemplifies the frontier of cervical care. These protocols harness the regenerative potential of biologics to enhance soft tissue healing while rehabilitative exercises restore strength and mobility. Additionally, pairing stem cell therapies with neuromuscular electrical stimulation (NMES) or virtual reality-assisted rehabilitation introduces novel neuroplasticity-driven recovery pathways, especially valuable for patients with spinal cord injuries or myelopathy. This multidisciplinary fusion underscores a patient-centered strategy prioritizing both symptom relief and quality of life.
When Should Patients Consider Escalating from Conservative to Surgical Options?
Determining the optimal timing for surgery in cervical conditions remains a delicate balance. While conservative treatments such as physical therapy, cervical traction, and non-surgical care for herniated discs can often suffice, persistent neurological deficits, worsening pain, or functional decline signal the need for surgical consultation. Orthopedic specialists assess pain severity, imaging results, and therapy responsiveness to recommend interventions that maximize benefit and minimize risk. Patients seeking a comprehensive overview of minimally invasive surgical pathways can benefit from resources like this detailed guide.
Championing Patient Empowerment: Communication as the Cornerstone of Healing
Ultimately, cervical spine treatment thrives on transparent dialogue and patient engagement. Specialists prioritize educating patients about diagnoses, treatment options, and prognoses, facilitating shared decision-making that aligns with individual values and lifestyles. This empowerment nurtures adherence, satisfaction, and better health outcomes. We invite readers to share their cervical spine treatment experiences or questions in the comments below, fostering a community of informed and proactive individuals. For personalized guidance, don’t hesitate to connect with our expert team, dedicated to advancing your spinal health journey.
Expert Insights & Advanced Considerations
Precision Diagnostics Are Transforming Cervical Spine Care
Incorporating sophisticated imaging and electrophysiological studies such as dynamic fluoroscopy, diffusion tensor imaging, and electromyography allows specialists to detect subtle biomechanical instabilities and neural impairments that conventional methods might miss. This precision facilitates highly tailored interventions, improving both surgical and non-surgical outcomes.
Multidisciplinary Integration Enhances Recovery and Long-Term Outcomes
The convergence of orthopedic surgeons, neurologists, pain management specialists, and rehabilitation therapists creates a synergistic environment for managing complex cervical conditions. This holistic approach addresses structural, neurological, and psychosocial facets simultaneously, fostering comprehensive healing and reducing the risk of recurrent symptoms.
Emerging Biologics and Neurorehabilitation Represent the Frontier of Treatment
Combining regenerative therapies such as platelet-rich plasma and stem cell injections with advanced neurorehabilitation techniques—including neuromuscular electrical stimulation and virtual reality exercises—capitalizes on neuroplasticity and tissue regeneration. These innovative protocols hold promise for enhancing functional restoration beyond traditional modalities.
Patient-Centered Decision-Making is Paramount in Navigating Complex Treatment Paths
Given the nuanced balance between conservative and surgical options, shared decision-making frameworks empower patients by aligning treatments with their values, lifestyle, and risk tolerance. Transparent communication and education improve adherence and satisfaction, ultimately optimizing outcomes.
Curated Expert Resources
American Academy of Orthopaedic Surgeons (AAOS): Offers authoritative guidelines and evidence-based reviews on multidisciplinary orthopedic care models and surgical indications, essential for specialists and patients seeking trusted recommendations.
The Spine Journal: Publishes cutting-edge research on emerging biomarkers, ultra-high-field MRI technologies, and regenerative therapies that are revolutionizing spinal disease management.
NjOrthopedicDoctor.xyz Resources: A comprehensive repository including expert advice on selecting spine surgeons, non-surgical treatment options, and minimally invasive surgical insights, offering practical guidance tailored to patient needs.
ClinicalTrials.gov: A valuable portal for tracking ongoing clinical trials in biologics and advanced rehabilitation strategies, enabling specialists and patients to stay abreast of emerging therapeutic opportunities.
Final Expert Perspective
The evolving landscape of cervical spine treatment underscores the importance of integrating advanced diagnostics, multidisciplinary collaboration, and innovative biologic therapies to deliver truly personalized care. Recognizing the multifaceted nature of neck disorders—from mechanical dysfunction to psychosocial influences—is essential for achieving durable recovery and quality of life improvements. Patients and clinicians alike benefit from embracing education, communication, and shared decision-making as foundational pillars in this journey.
If you are navigating cervical spine challenges or seeking to deepen your understanding of the latest treatment paradigms, consider engaging with expert communities and trusted resources. Share your insights or questions below, or explore specialized guidance at our contact page to connect with leading cervical spine specialists dedicated to advancing your spinal health.


I found this article really insightful, especially the focus on the importance of early diagnosis and multidisciplinary care. Often, people underestimate how complex neck pain can be, mistaking it for just muscle strain. In my own experience, consulting a specialist early made a huge difference—especially when I opted for advanced diagnostics like MRI and nerve studies. It’s fascinating how emerging technologies like diffusion tensor imaging could revolutionize how we diagnose subtle nerve issues. Have others here had experience with these cutting-edge diagnostic tools? I’d love to hear how they impacted your treatment plans and outcomes. It seems like combining state-of-the-art imaging with biologic therapies and rehab holds great promise for deep recovery, not just symptom relief. What do you think is the most promising new approach for those with chronic neck issues that don’t respond to traditional therapies? I believe it’s an exciting time for personalized spinal care, and staying informed is key to making the right decisions.
This article sheds light on the complexity of diagnosing and treating neck issues, which I personally experienced. I initially thought my persistent neck pain was just muscle tension until advanced diagnostics revealed a herniated disc pressing on my nerve. The detailed explanation of multidisciplinary care and emerging technologies like diffusion tensor imaging is encouraging, as these approaches seem to offer a more precise understanding of neural impairments. One aspect I found particularly interesting is how biologic therapies, like PRP, are being integrated into recovery protocols. Has anyone here experienced regenerative treatments firsthand? If so, what was your recovery process like, and did you notice meaningful improvements? It’s remarkable how far cervical spine treatment has come, combining innovation and personalized care. I’m curious, what emerging treatments or diagnostics do others believe will make the biggest difference for chronic cases resistant to traditional therapy? For me, staying informed and proactive was key to my recovery, and I’d recommend others consider early and comprehensive evaluations.
Reading this post really resonated with my own experience of dealing with neck pain. I used to think it was just muscle strain from sitting at my desk too long, but after visiting a specialist and undergoing advanced diagnostics like MRI and nerve conduction studies, I learned I had a herniated disc pressing on my nerve. The detailed process of how multidisciplinary care can make a difference really opened my eyes. In fact, combining physical therapy, regenerative injections such as PRP, and patient education helped me recover much faster than I expected. It made me wonder, though—how do you decide when to explore cutting-edge diagnostics like diffusion tensor imaging, especially if initial treatments aren’t working? Would love to hear others’ thoughts or personal stories about including innovative imaging or biologics in their treatment plans. It does seem like we’re moving towards more personalized and less invasive options, which is really encouraging for those with persistent neck issues.