Decoding Your Back Pain: Surgery or Chiropractic Care?
When persistent spine discomfort strikes, deciding between spine surgery and chiropractic care can feel daunting. This crossroads demands expert evaluation to understand the root cause of your pain and the most effective path forward. An orthopedic evaluation serves as a crucial compass, guiding patients through this complex decision-making process with clarity and precision.
Why an Orthopedic Evaluation Is Your Best First Step
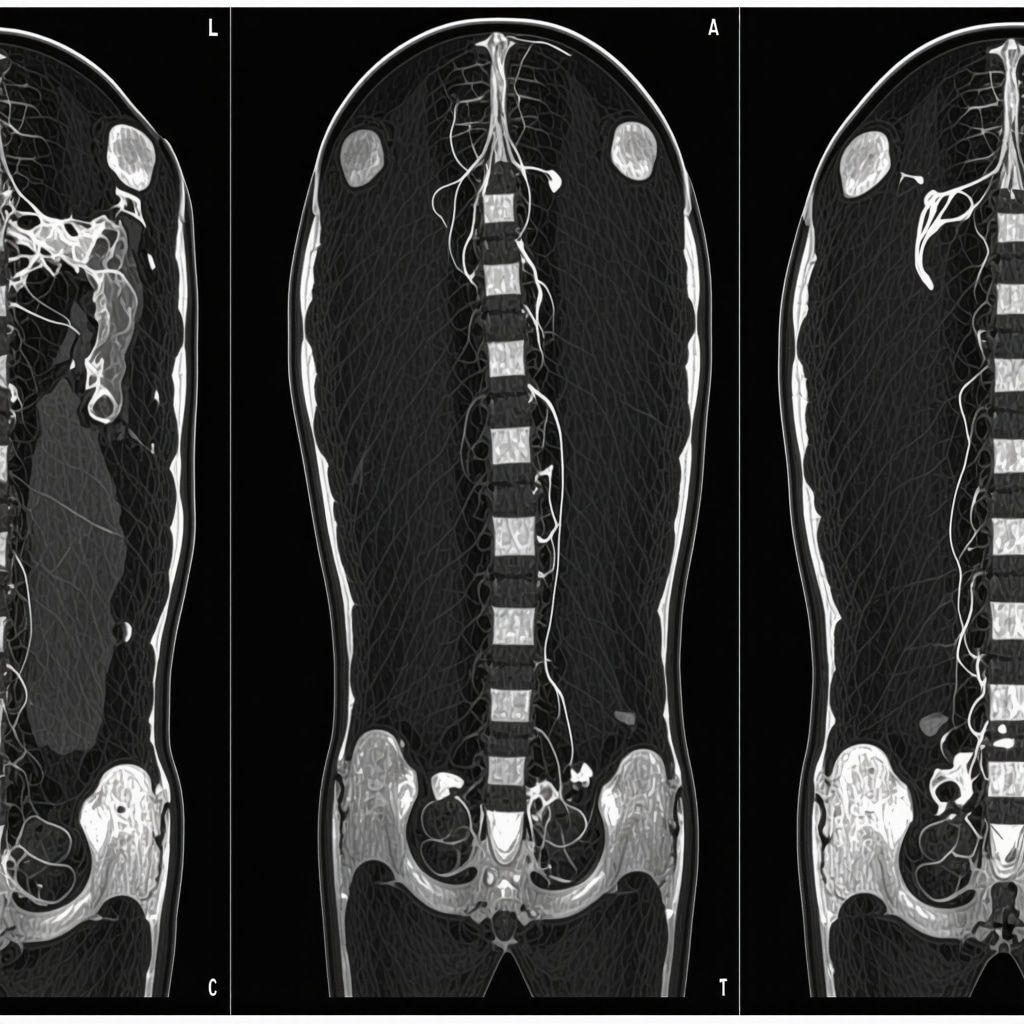
Orthopedic specialists bring a wealth of knowledge about musculoskeletal health, particularly the spine’s intricate anatomy and biomechanics. Through comprehensive physical examinations, detailed medical histories, and advanced imaging techniques like MRI or CT scans, orthopedic doctors can pinpoint whether your condition necessitates surgical intervention or if conservative treatments like chiropractic care could suffice. For example, a patient suffering from a herniated disc causing nerve compression might initially benefit from non-surgical options, including chiropractic adjustments, physical therapy, or orthopedic injections, but if neurological deficits progress, surgery might become imperative.
How Do Orthopedic Experts Differentiate Between Cases Needing Surgery or Chiropractic Care?
Orthopedic evaluation focuses on several key factors: the severity of symptoms, neurological involvement (such as numbness, weakness, or loss of bladder control), response to prior treatments, and specific diagnostic findings. Surgery is typically reserved for cases with structural instability, significant nerve compression, or when conservative management fails. Conversely, chiropractic care is often effective for mechanical back pain, minor disc bulges, or muscular imbalances without alarming neurological signs. This nuanced decision hinges on balancing risks, benefits, and patient preferences, underscoring the importance of expert guidance.
Case Study: Navigating Treatment Choices with Expert Insight
Consider a 45-year-old woman with chronic lower back pain radiating down her leg. After an orthopedic evaluation revealing moderate lumbar disc herniation without severe nerve impairment, she embarked on a chiropractic care regimen combined with physical therapy. Over several months, her symptoms improved significantly, avoiding the risks associated with surgery. This real-world example highlights how orthopedic assessments can facilitate tailored treatment plans that prioritize safety and efficacy.
Integrating Orthopedic and Chiropractic Approaches for Optimal Spine Health
In many cases, orthopedic surgeons and chiropractors collaborate to optimize patient outcomes. Orthopedic clearance is essential before initiating chiropractic care in complex cases to rule out contraindications. Additionally, incorporating minimally invasive treatments and orthopedic injections can complement chiropractic adjustments, providing faster relief and improved function. For more in-depth insights on conservative spine treatments, explore effective non-surgical care for herniated discs.
According to the American Academy of Orthopaedic Surgeons, conservative management is recommended initially for most spinal conditions unless urgent neurological symptoms arise (AAOS Low Back Pain Guide).
Ready to Make an Informed Choice on Spine Care?
If you’re wondering whether spine surgery or chiropractic care is right for you, an expert orthopedic evaluation is indispensable. Contact our orthopedic specialists today to schedule a consultation and embark on a personalized journey toward spine health.
Understanding the Gray Areas: When Surgery Becomes Necessary
One thing I’ve learned through my journey and countless patient stories is that the decision between spine surgery and chiropractic care isn’t always black and white. Sometimes, the symptoms evolve or worsen despite conservative interventions. For example, if you start experiencing worsening numbness, muscle weakness, or even bowel and bladder control issues, these are red flags that warrant urgent orthopedic re-evaluation. In such scenarios, surgery often becomes the safest and most effective choice to prevent permanent nerve damage.
During one of my follow-up visits, an orthopedic specialist explained how dynamic spinal conditions can be. A seemingly minor disc herniation can progress, causing increased nerve compression, which might not be apparent until neurological symptoms develop. That’s why staying vigilant and maintaining regular orthopedic follow-up care is critical, which you can learn more about in this guide on orthopedic follow-up care.
Personalizing Treatment: Why One Size Doesn’t Fit All
What stood out for me in my orthopedic evaluations was how personalized the treatment plans were. Factors like age, activity level, overall health, and even personal preferences play a vital role. For instance, a young athlete with a herniated disc might lean toward minimally invasive surgery for a faster return to sports, while an older adult may prefer extended conservative care to avoid surgical risks.
Orthopedic experts often collaborate with chiropractors and physical therapists to craft integrative plans. This multidisciplinary approach was key in my recovery journey, and it’s supported by research published by the American Academy of Orthopaedic Surgeons (AAOS), which highlights the benefits of combining conservative and surgical strategies based on individual patient needs.
How Do You Know When to Escalate From Chiropractic Care to Surgery?
This question is probably on many minds when exploring spine care options. From my experience and discussions with orthopedic specialists, it boils down to monitoring symptom progression and quality of life impact. If conservative treatments like chiropractic adjustments and physical therapy provide no lasting relief or neurological symptoms appear or worsen, it’s time to seek surgical consultation. Always keep open communication with your healthcare providers and don’t hesitate to get a second opinion if unsure. Resources like how to get a second opinion from an orthopedic surgeon can make this process less intimidating.
Taking the First Step: How to Approach Your Orthopedic Evaluation
Scheduling that initial orthopedic evaluation can feel overwhelming, but preparation helps. I recommend gathering any previous imaging reports, noting symptom patterns, and listing all treatments tried so far. Being open about your lifestyle and goals also allows the orthopedic team to tailor their recommendations effectively.
If you’re considering chiropractic care, it’s wise to first obtain orthopedic clearance, especially if you have complex spine issues. This ensures that chiropractic adjustments are safe and appropriate for your condition. Learn more about choosing the right orthopedic surgeon to guide you through this process.
Have you ever faced this crossroads between surgery and chiropractic care? Share your story or questions in the comments below—I’d love to hear how others navigate these tough decisions. And if you want to dive deeper into related topics, check out our articles on minimally invasive back pain treatments and orthopedic injections for back pain relief to expand your knowledge further.
Unraveling Complex Spine Disorders: The Orthopedic Evaluation’s Critical Role in Tailored Treatment
In cases where spine issues present with atypical or multifactorial symptoms, the orthopedic evaluation transcends routine assessment, becoming a sophisticated diagnostic tool that integrates biomechanical analysis, neurophysiological testing, and advanced imaging interpretation. Specialists often employ dynamic MRI or upright CT scans to capture spine behavior under functional loads, offering insights into instability or subtle nerve impingements invisible in static imaging. This depth of evaluation is vital for distinguishing conditions like foraminal stenosis versus discogenic pain, which demand vastly different treatment trajectories.
What Are the Latest Diagnostic Techniques Orthopedic Experts Use to Differentiate Candidates for Surgery Versus Chiropractic Care?
Beyond conventional MRI and physical exams, cutting-edge modalities like diffusion tensor imaging (DTI) and electromyography (EMG) are increasingly adopted to map nerve integrity and muscular response patterns. Such tools provide objective data to predict surgical outcomes and identify when chiropractic adjustments might exacerbate underlying neural compromise. For instance, DTI can reveal microstructural nerve damage, informing whether conservative care is safe or if decompression surgery is warranted.
Additionally, pressure-sensitive gait analysis and posture mapping augment clinical findings, enabling orthopedic teams to pinpoint biomechanical contributors to pain that chiropractic interventions can address effectively. This multidisciplinary diagnostic approach embodies the future of personalized spine care.
For a detailed review of advanced imaging in spine diagnostics, see the NIH article on Functional MRI and Spine Disorders.
Integrative Protocols: How Combining Surgical Expertise and Chiropractic Care Enhances Recovery
Recognizing the spectrum of spine pathologies, many orthopedic centers now implement integrative protocols where surgical intervention and chiropractic care function synergistically. Pre-surgical chiropractic interventions can optimize spinal alignment, potentially reducing operative risk and improving post-operative rehabilitation outcomes. Conversely, post-operative chiropractic adjustments (with strict orthopedic clearance) help restore mobility, address soft tissue adhesions, and facilitate neuro-muscular re-education.
This collaborative strategy demands continuous communication between orthopedic surgeons and chiropractors, supported by outcome tracking through validated patient-reported metrics. Such integrative care plans have demonstrated improved pain control, functional restoration, and patient satisfaction compared to isolated treatment modalities.
Refining Decision-Making: The Role of Patient-Specific Risk Profiling in Orthopedic Evaluations
Advanced orthopedic evaluations incorporate comprehensive risk profiling, factoring in comorbidities such as osteoporosis, diabetes, and cardiovascular disease, which can influence both surgical risks and chiropractic therapy tolerance. Tools like the Spine Surgical Risk Score (SSRS) help quantify potential complications, guiding personalized recommendations.
Moreover, psychological assessment for factors like pain catastrophizing or depression is integral, as these influence treatment responsiveness. Patients demonstrating high psychosocial risk may benefit from multidisciplinary programs including cognitive-behavioral therapy alongside physical treatments, ensuring holistic management beyond the mechanical aspects.
How Does Psychosocial Profiling Influence the Choice Between Spine Surgery and Chiropractic Care?
Orthopedic research increasingly highlights that psychosocial factors are predictors of post-treatment outcomes. For example, patients with significant anxiety or depressive symptoms often report less improvement post-surgery and may respond better to conservative care that includes psychosocial support. Integrating these assessments ensures treatment plans align not only with anatomical findings but also with mental and emotional readiness, optimizing overall recovery.
Enhancing Patient Engagement: Tools and Strategies for Informed Orthopedic Consultation
Empowering patients through education is a cornerstone of expert orthopedic care. Interactive decision aids, 3D spine models, and virtual reality simulations are emerging as effective tools that help patients visualize pathology and understand procedural implications. This transparency fosters shared decision-making, reduces decisional conflict, and aligns expectations.
If you want to explore these advanced diagnostic and integrative treatment approaches for your spine condition, connect with our orthopedic specialists to schedule a comprehensive evaluation tailored to your unique needs.
Decoding Complex Spine Disorders: Beyond Traditional Assessments
While many back pain cases can be managed through standard diagnostic tools, complex spine disorders require a more intricate approach. Orthopedic specialists now harness dynamic imaging and neurophysiological testing to elucidate conditions that elude conventional methods. These evaluations provide a multidimensional view of spinal mechanics and nerve function, ensuring treatment plans are precisely tailored to each patient’s unique pathology.
What Are the Latest Diagnostic Techniques Orthopedic Experts Use to Differentiate Candidates for Surgery Versus Chiropractic Care?
Emerging technologies such as diffusion tensor imaging (DTI) and electromyography (EMG) have revolutionized the diagnostic landscape. DTI allows detailed visualization of nerve fiber integrity, detecting microstructural damage undetectable in standard MRI scans, while EMG assesses muscular responses to nerve stimuli, highlighting functional impairments. These modalities enable clinicians to discern when conservative chiropractic adjustments are feasible or when surgical decompression is imperative to prevent further neural compromise.
Complementary assessments like pressure-sensitive gait analysis and advanced posture mapping further refine biomechanical understanding, illuminating subtle dysfunctions amenable to chiropractic intervention. This integrated diagnostic algorithm epitomizes precision medicine in spine care.
For an authoritative exploration of these advanced imaging techniques, consult the NIH article on Functional MRI and Spine Disorders, which delves into the clinical utility of dynamic modalities.
Synergistic Recovery: Merging Surgical Expertise with Chiropractic Care
Recognizing that neither surgery nor chiropractic care alone suffices for all spine conditions, integrative protocols are increasingly adopted. Preoperative chiropractic adjustments can optimize spinal alignment, potentially reducing intraoperative risk and enhancing postoperative healing. Post-surgery, chiropractic interventions—administered with orthopedic clearance—facilitate restoration of mobility, mitigate soft tissue adhesions, and accelerate neuromuscular re-education.
This collaborative continuum necessitates seamless communication between orthopedic surgeons and chiropractors, underscored by outcome tracking through validated patient-reported measures. Evidence indicates such multidisciplinary strategies yield superior pain relief, functional recovery, and patient satisfaction compared to isolated treatments.
Risk Stratification: Personalizing Spine Care Beyond Anatomy
Advanced orthopedic evaluations incorporate comprehensive risk profiling encompassing comorbidities like osteoporosis, diabetes, and cardiovascular disease, which influence not only surgical candidacy but also tolerance to chiropractic therapies. Tools such as the Spine Surgical Risk Score (SSRS) quantify complication probabilities, empowering clinicians to tailor interventions appropriately.
How Does Psychosocial Profiling Influence the Choice Between Spine Surgery and Chiropractic Care?
Psychosocial dimensions—encompassing anxiety, depression, and pain catastrophizing—exert profound effects on treatment outcomes. Orthopedic research underscores that patients with elevated psychosocial risk often experience diminished post-surgical improvement but may respond favorably to conservative care enriched with psychological support. Incorporating these assessments ensures that treatment plans align holistically with both physiological and emotional patient profiles, optimizing recovery trajectories.
Empowering Patients: Innovative Tools for Informed Orthopedic Consultations
Patient engagement is pivotal for successful spine care. Emerging technologies such as interactive decision aids, 3D spine models, and virtual reality simulations offer immersive educational experiences that demystify complex pathologies and procedural nuances. This transparency fosters shared decision-making, alleviates decisional conflict, and harmonizes expectations between patients and providers.
If you seek to explore these advanced diagnostic and integrative treatment modalities tailored to your spine condition, connect with our orthopedic specialists to schedule a comprehensive consultation and embark on a personalized journey toward optimal spine health.
Frequently Asked Questions (FAQ)
What are the key signs that indicate spine surgery might be necessary instead of chiropractic care?
Signs that surgery may be necessary include progressive neurological deficits such as worsening numbness, muscle weakness, loss of bladder or bowel control, spinal instability, and failure to improve with conservative care. These red flags suggest nerve compression or structural issues that require surgical intervention to prevent permanent damage.
Can chiropractic care be safely combined with orthopedic treatment?
Yes, chiropractic care can be integrated with orthopedic management when guided by orthopedic clearance. Pre- and post-surgical chiropractic interventions, when coordinated with surgeons, can optimize spinal alignment, reduce operative risks, and enhance rehabilitation outcomes, providing a comprehensive approach to spine health.
How does an orthopedic evaluation differentiate between candidates for surgery versus chiropractic care?
An orthopedic evaluation assesses symptom severity, neurological involvement, imaging findings, and response to prior treatments. Advanced diagnostics like MRI, diffusion tensor imaging, and electromyography help clarify nerve integrity and biomechanical factors, enabling a personalized recommendation for either surgical or conservative management.
What role do psychosocial factors play in deciding between surgery and chiropractic care?
Psychosocial elements such as anxiety, depression, and pain catastrophizing significantly influence treatment outcomes. Patients with high psychosocial risk may respond better to conservative care with psychological support, while those mentally prepared and medically indicated may benefit more from surgery. Incorporating psychosocial profiling ensures holistic, patient-centered care.
When should a patient seek a second opinion regarding their spine treatment options?
Patients should consider a second opinion if they are uncertain about their diagnosis, recommended treatment, or if symptoms persist or worsen despite treatment. A second orthopedic consultation can provide reassurance, alternative perspectives, and help confirm the best individualized treatment strategy.
What are the latest diagnostic tools used in orthopedic spine evaluations?
Beyond traditional MRI and CT scans, advanced modalities such as diffusion tensor imaging (DTI), electromyography (EMG), dynamic MRI, and pressure-sensitive gait analysis are increasingly utilized. These technologies provide detailed insights into nerve integrity, muscular responses, and functional biomechanics, improving diagnostic precision.
How does risk profiling influence treatment planning for spine conditions?
Risk profiling incorporates comorbidities like osteoporosis, diabetes, and cardiovascular disease, alongside surgical risk scores to assess complication probabilities. This helps tailor treatment recommendations, balancing benefits and risks, and ensuring patient safety and optimal outcomes.
Is chiropractic care effective for herniated discs?
Chiropractic care can be effective for mild to moderate herniated discs without significant nerve compression or neurological deficits. It focuses on spinal alignment, muscle balance, and pain relief. However, patients must be carefully evaluated to ensure chiropractic adjustments are safe and beneficial.
What should patients prepare before an orthopedic evaluation?
Patients should bring previous imaging studies, document symptom history and patterns, list prior treatments, and clearly communicate their lifestyle and health goals. Being open about psychosocial factors and expectations aids the orthopedic team in crafting personalized, effective treatment plans.
How do orthopedic surgeons and chiropractors collaborate for better patient outcomes?
Collaboration involves shared communication, coordinated treatment timing, and mutual understanding of patient status. Orthopedic surgeons provide medical clearance and surgical expertise, while chiropractors contribute biomechanical adjustments and rehabilitation support. This integrated approach enhances recovery, reduces complications, and improves patient satisfaction.
Trusted External Sources
- American Academy of Orthopaedic Surgeons (AAOS) – Provides authoritative guidelines on spine conditions, surgical indications, and conservative management strategies, supporting evidence-based clinical decisions.
- National Institutes of Health (NIH) – Functional MRI and Spine Disorders – Offers in-depth research on advanced imaging techniques like dynamic MRI and diffusion tensor imaging, enhancing diagnostic accuracy in complex spine cases.
- Spine Surgical Risk Score (SSRS) Research Publications – Presents validated tools for quantifying surgical risks and aiding personalized treatment planning based on patient comorbidities.
- Journal of Orthopaedic & Sports Physical Therapy (JOSPT) – Features peer-reviewed studies on integrative spine care approaches, including chiropractic and surgical collaboration outcomes.
- American Chiropractic Association (ACA) – Offers insights on chiropractic best practices, safety considerations, and their role within multidisciplinary spine care frameworks.
Conclusion: Navigating the Path Between Spine Surgery and Chiropractic Care
Deciding between spine surgery and chiropractic care hinges on a comprehensive orthopedic evaluation that integrates clinical findings, advanced diagnostic techniques, and personalized risk assessments. Recognizing the dynamic nature of spine disorders, treatment plans must be adaptable, balancing the benefits of conservative therapies with timely surgical intervention when necessary. Integrative protocols combining surgical expertise and chiropractic care underscore the future of optimal spine health management.
Empowered with thorough knowledge and expert guidance, patients can make informed decisions that align with their unique anatomy, psychosocial profile, and lifestyle goals. If you are facing the crossroads of spine treatment options, prioritize an expert orthopedic consultation to chart the safest and most effective course forward.
Share your experiences, ask questions, or explore our related expert articles to deepen your understanding and take active control of your spine health journey.


This article offers a thorough overview of how an orthopedic evaluation can be crucial in deciding whether surgery or chiropractic care is more appropriate for back pain. I appreciate how it highlights the importance of personalized treatment plans, considering factors like age, activity level, and psychosocial aspects. From my own experience with chronic back issues, I found that combining diagnostic precision with a multidisciplinary approach really made a difference in recovery. It’s reassuring to see that collaboration between surgeons and chiropractors can optimize outcomes. One thing I wonder about is how emerging diagnostic tools like diffusion tensor imaging (DTI) might become more mainstream in evaluating nerve damage. Has anyone here had experience with advanced imaging methods and noticed a difference in their treatment planning? I believe that staying informed about technological advances can truly empower patients to make better decisions.
This is a really comprehensive overview of the decision-making process involved in spine care. From my own experience, I’ve seen how crucial an thorough orthopedic evaluation can be, especially in cases where symptoms aren’t straightforward. The emphasis on personalized treatment plans resonated with me—what works for one patient might not be suitable for another, particularly considering age, activity levels, and psychosocial factors. I’ve wondered, though, how accessible some of these advanced diagnostic tools like diffusion tensor imaging are in regular clinical practice. Are they becoming more common? I believe that wider availability could really improve the accuracy of distinguishing cases that need surgery from those that can be managed conservatively with chiropractic or physical therapy.
This post really sheds light on the importance of a thorough orthopedic evaluation before jumping to treatment options. I had a similar experience where an detailed assessment, including advanced imaging, helped my doctor determine that conservative care was the best initial approach for my herniated disc. I wonder how often orthopedic specialists incorporate newer diagnostic tools like diffusion tensor imaging (DTI) or upright MRI in routine practice. From my understanding, these technologies could make a significant difference in early diagnosis and personalized treatment plans. Has anyone here had experience with these advanced diagnostics, and did it impact their treatment decisions? It seems that staying informed about such advancements can empower patients to advocate for the most appropriate care. I believe an integrated approach between surgeons, chiropractors, and physical therapists offers the best pathway to recovery, tailored to each individual’s needs. Would love to hear more about how others navigated the decision-making process!