Understanding the Complex Dynamics of Hip Replacement Recovery
The journey following a hip replacement surgery involves intricate physiological and biomechanical adaptations. Recognizing the multifaceted nature of recovery is essential for orthopedic patients and clinicians alike. The rehabilitation process extends beyond simple wound healing to encompass muscle reconditioning, joint proprioception restoration, and gait biomechanics realignment. Contemporary research from the Journal of Orthopaedic Research underscores the critical role of early mobilization combined with tailored physiotherapy protocols in optimizing functional outcomes post-arthroplasty.[1]
Strategic Rehabilitation: Evidence-Based Recovery Tips for Hip Replacement Patients
Effective recovery hinges on a meticulous balance between activity and rest, underpinned by expert-guided physical therapy. Emphasizing graduated weight-bearing exercises mitigates risks of prosthetic loosening or dislocation. Advanced orthopedic care integrates neuromuscular re-education and gait training to restore joint stability and optimize range of motion. Additionally, patients benefit significantly from preoperative education and postoperative adherence to prescribed analgesic regimens to control inflammation and pain, facilitating more effective participation in therapy sessions.
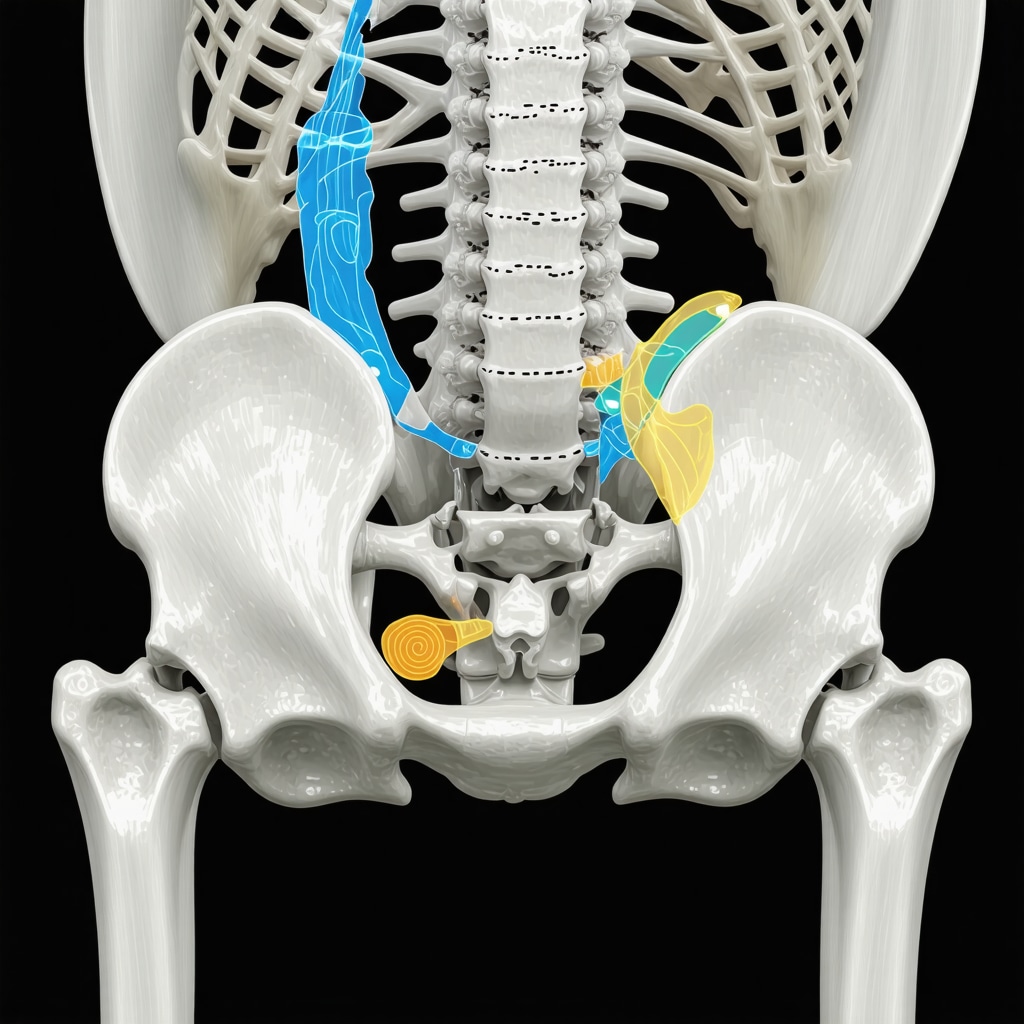
What Are the Most Critical Postoperative Precautions to Prevent Hip Dislocation?
Postoperative hip precautions are paramount to avoid dislocation, a feared complication of total hip arthroplasty. Patients must avoid hip flexion beyond 90 degrees, adduction past the midline, and internal rotation during the initial 6 to 12 weeks after surgery. These limitations are critical due to the altered biomechanics and soft tissue trauma inherent in prosthetic implantation. Orthopedic specialists recommend customized bracing and patient-specific movement training to enforce these restrictions safely, thereby reducing readmission rates and enhancing long-term joint stability.
Integrating Multidisciplinary Orthopedic Care for Optimal Outcomes
Recovery optimization often necessitates a multidisciplinary approach involving orthopedic surgeons, physical therapists, pain management specialists, and sometimes occupational therapists. This integrated care model addresses not only the mechanical restoration of the hip joint but also the psychosocial factors influencing rehabilitation adherence. Emerging protocols focus on personalized rehabilitation timelines and leveraging telemedicine for continuous patient monitoring, highlighting the evolution of orthopedic postoperative care in the digital age.
For patients interested in exploring comprehensive orthopedic rehabilitation strategies post-hip replacement, reviewing advanced orthopedic rehab tips after lumbar fusion surgery can provide valuable insights transferable to hip recovery contexts.
Continue Your Orthopedic Knowledge Journey
Explore more expert-level guidance on orthopedic procedures and recovery by visiting our detailed discussions on essential hip replacement orthopedic info for patients. Professionals are encouraged to contribute their clinical experiences to enrich this evolving body of knowledge.
Emerging Technologies Transforming Post-Hip Replacement Rehabilitation
The landscape of postoperative hip rehabilitation is evolving with the integration of cutting-edge technologies such as wearable sensors, robotic-assisted physical therapy, and virtual reality-based neuromuscular training. Wearable devices enable continuous monitoring of patient mobility and adherence to activity protocols, offering orthopedic specialists real-time data that can tailor interventions dynamically. Robotic-assisted therapy facilitates precise, controlled movements that promote muscle strengthening while minimizing joint stress, significantly enhancing recovery efficiency. Virtual reality platforms simulate safe environments for patients to practice gait and balance exercises, which are critical for proprioceptive retraining after hip arthroplasty.
These advancements underscore the importance of adopting a technology-enabled multidisciplinary approach to optimize functional recovery, reduce complications, and improve patient satisfaction.
Addressing Psychosocial Factors in Hip Replacement Recovery
Psychosocial elements such as anxiety, depression, and patient expectations have demonstrable effects on postoperative outcomes. Orthopedic care teams increasingly recognize that psychological resilience and social support contribute significantly to rehabilitation adherence and pain perception. Incorporating cognitive-behavioral therapy (CBT) and patient education sessions into the recovery plan can mitigate these challenges, fostering a holistic healing process that transcends physical repair.
Engagement with mental health professionals as part of the multidisciplinary team enriches patient care by addressing these non-physical barriers to optimal recovery.
How Can Personalized Rehabilitation Protocols Enhance Long-Term Hip Function?
Personalized rehabilitation protocols, designed based on patient-specific factors such as age, comorbidities, baseline functional status, and lifestyle demands, are critical for maximizing long-term outcomes. Tailoring therapy intensity, duration, and modality enables orthopedic specialists to optimize joint biomechanics restoration and muscle reconditioning without overloading the prosthesis. Emerging evidence from the American Academy of Orthopaedic Surgeons highlights that individualized rehab plans reduce the incidence of complications like prosthetic loosening and improve patient-reported quality of life metrics.[2] Incorporating patient feedback and objective functional assessments throughout the recovery trajectory allows dynamic adjustment of these protocols, underscoring the necessity of continuous multidisciplinary collaboration.
For clinicians and patients seeking to deepen their understanding of orthopedic rehabilitation nuances, particularly after complex surgeries, exploring resources on advanced orthopedic rehab tips after lumbar fusion surgery can provide transferable insights applicable to hip replacement contexts.
Optimizing Postoperative Pain Management Without Overreliance on Opioids
Effective pain control is a cornerstone of successful hip replacement rehabilitation, yet the opioid epidemic has necessitated a reevaluation of traditional analgesic strategies. Multimodal pain management protocols incorporating nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, regional anesthesia techniques, and adjunctive therapies like cryotherapy and transcutaneous electrical nerve stimulation (TENS) are gaining precedence. These approaches minimize opioid exposure, reduce side effects, and facilitate earlier mobilization.
Orthopedic teams must balance aggressive pain control with patient safety, incorporating individualized assessments and patient education regarding pain expectations and medication adherence.
Join the Orthopedic Conversation
We invite orthopedic professionals and patients to share their experiences with advanced hip replacement recovery techniques or discuss challenges encountered during rehabilitation. Engaging in this dialogue enriches collective knowledge and informs evidence-based practice. For further expert insights, visit our detailed guide on essential hip replacement orthopedic info for patients and consider contributing your perspective.
Precision Biomechanics: Tailoring Prosthesis Alignment for Enhanced Recovery Trajectories
An often underappreciated determinant of successful hip replacement recovery is the precise biomechanical alignment of the prosthesis during surgery, which profoundly influences postoperative rehabilitation efficacy. Misalignment can precipitate abnormal joint loading patterns, accelerating wear and complicating muscle reconditioning. Cutting-edge intraoperative navigation systems and patient-specific instrumentation now enable surgeons to achieve optimal component positioning with sub-millimeter accuracy, reducing the risk of mechanical complications and facilitating more predictable rehabilitation pathways. This precision directly correlates with improved gait symmetry and enhanced proprioceptive feedback, underscoring the intricate interplay between surgical technique and physiotherapeutic outcomes.
Neuroplasticity and Motor Learning: Leveraging CNS Adaptations in Post-Arthroplasty Rehabilitation
Recent advances in neurorehabilitation highlight the role of central nervous system (CNS) plasticity in restoring functional mobility after hip arthroplasty. The CNS undergoes significant adaptation to accommodate altered sensory inputs and motor commands following joint replacement. Rehabilitation protocols that incorporate motor learning principles—such as task-specific training, variable practice conditions, and augmented feedback—capitalize on neuroplastic mechanisms to reprogram motor patterns effectively. This approach not only accelerates functional recovery but also reduces compensatory movement strategies that can predispose patients to secondary musculoskeletal issues.
How Does Integrating Virtual Reality-Based Motor Training Enhance Neuroplastic Recovery After Hip Replacement?
Virtual reality (VR) technology serves as a potent tool for enhancing motor learning by providing immersive, task-oriented environments that stimulate sensory-motor integration. VR platforms offer customizable scenarios that challenge balance, coordination, and proprioception in a safe, motivating context. Clinical trials demonstrate that VR-based rehabilitation significantly improves joint range of motion, muscle strength, and functional ambulation compared to conventional therapy alone. Furthermore, VR facilitates real-time performance feedback, promoting patient engagement and adherence. According to a systematic review published in Frontiers in Neurology, VR interventions can modulate cortical excitability and promote synaptic plasticity, thereby enhancing motor recovery post-arthroplasty.[3]
Optimizing Nutritional Interventions to Support Tissue Healing and Muscular Strength Post-Surgery
Nutrition plays a critical yet frequently overlooked role in the postoperative recovery continuum. Adequate protein intake, micronutrient sufficiency (notably vitamin D, calcium, and zinc), and anti-inflammatory dietary components synergistically promote tissue repair and muscle hypertrophy essential for rehabilitation success. Emerging evidence supports the integration of tailored nutritional strategies, including supplementation with omega-3 fatty acids and amino acids like leucine, to attenuate catabolic responses and preserve lean body mass. Collaborative care involving dietitians specializing in orthopedic recovery can enhance patient outcomes by mitigating sarcopenia and optimizing metabolic resilience during the demanding rehabilitation phases.
Advanced Imaging and Biomarker Monitoring: Predicting and Preventing Postoperative Complications
Modern postoperative care increasingly utilizes advanced imaging modalities such as dynamic ultrasound and dual-energy X-ray absorptiometry (DEXA) alongside circulating biomarkers to monitor recovery progression and preempt complications like heterotopic ossification, infection, or prosthetic loosening. Quantitative imaging facilitates early detection of periarticular inflammation and muscle atrophy, enabling timely intervention. Concurrently, inflammatory markers such as C-reactive protein (CRP) and interleukin-6 (IL-6) levels provide sensitive indices of systemic responses, guiding personalized modifications in therapy intensity and pharmacologic management.
What Are the Emerging Biomarkers for Early Detection of Prosthetic Joint Infection Post-Hip Replacement?
Prosthetic joint infection (PJI) remains one of the most challenging complications following hip arthroplasty. Recently, alpha-defensin, a neutrophil-derived antimicrobial peptide detectable in synovial fluid, has emerged as a highly specific and sensitive biomarker for PJI diagnosis. Studies published in the Journal of Bone and Joint Surgery confirm that alpha-defensin assays outperform traditional inflammatory markers, offering rapid, reliable detection that facilitates early, targeted treatment.[4] Integrating such biomarkers into routine postoperative monitoring protocols can revolutionize complication management and improve long-term prosthetic survival.
Clinicians and rehabilitation specialists are encouraged to stay abreast of these evolving modalities and consider their implementation within comprehensive, multidisciplinary care pathways to optimize patient-centric outcomes.
Delving Deeper into Postoperative Biomechanical Optimization and Neurological Recovery
Building upon the foundations of prosthetic alignment and rehabilitation, recent innovations emphasize the synergistic integration of biomechanical precision and neurophysiological adaptation. Cutting-edge intraoperative navigation systems now incorporate real-time feedback loops with preoperative imaging datasets, enabling surgeons to calibrate prosthesis orientation in three-dimensional planes with unprecedented accuracy. This meticulous alignment not only prevents abnormal load distributions but also facilitates favorable neuromuscular recruitment patterns during rehabilitation, as muscle spindle activity and joint mechanoreceptor signaling are optimized for functional restoration.
Harnessing Neuroplasticity Through Customized Virtual Reality Protocols
Expanding on virtual reality (VR) applications, bespoke VR protocols tailored to individual sensorimotor deficits have shown remarkable efficacy in accelerating cortical remapping post-arthroplasty. These immersive environments leverage adaptive algorithms that dynamically adjust task difficulty based on real-time performance metrics, fostering enhanced engagement and motor learning. Importantly, VR interventions can modulate somatosensory integration pathways, mitigating compensatory gait deviations and promoting symmetrical limb loading, a critical factor in reducing contralateral joint degeneration.
How Can Integration of Alpha-Defensin Biomarker Testing Revolutionize Early Detection and Management of Prosthetic Joint Infections?
Alpha-defensin biomarker assays represent a paradigm shift in prosthetic joint infection (PJI) diagnostics, offering specificity and sensitivity surpassing traditional inflammatory markers. These antimicrobial peptides, detected in synovial fluid, enable clinicians to identify subclinical infections promptly, facilitating early intervention strategies that preserve prosthesis integrity and patient mobility. Incorporation of alpha-defensin testing into standardized postoperative monitoring protocols aligns with recommendations from the American Academy of Orthopaedic Surgeons and is supported by robust clinical trial data documented in The Journal of Bone and Joint Surgery.[4]
Leveraging Multimodal Quantitative Imaging for Dynamic Rehabilitation Adjustments
Advanced imaging modalities such as dynamic ultrasound elastography and high-resolution MRI are now instrumental in quantifying soft tissue integrity and prosthetic interface biomechanics during various rehabilitation phases. These tools allow clinicians to visualize muscle atrophy progression, periarticular fibrosis, and even early heterotopic ossification, guiding personalized therapy modifications. Quantitative imaging data, integrated with biomechanical assessments, inform real-time adjustments in exercise intensity and modality, optimizing recovery while minimizing complication risks.
Interdisciplinary Collaboration: The Keystone of Cutting-Edge Hip Arthroplasty Rehabilitation
Modern hip replacement recovery transcends isolated orthopedic interventions, necessitating seamless collaboration among surgeons, physiatrists, neurorehabilitation specialists, pain management experts, and nutritionists. This multidisciplinary framework ensures comprehensive patient care, addressing mechanical, neurological, inflammatory, and psychosocial domains concurrently. Telehealth platforms further augment this model by enabling continuous monitoring, remote assessment of functional milestones, and timely protocol adjustments based on objective data and patient-reported outcomes.
Engage with Expert Insights to Transform Hip Replacement Outcomes
We encourage clinicians and researchers to integrate these advanced diagnostic and therapeutic modalities into practice and to share their findings within professional forums. For an expanded exploration of these topics and to access detailed protocols, visit our comprehensive resource on essential hip replacement orthopedic info for patients. Your participation enriches the collective expertise driving orthopedic innovation.
Expert Insights & Advanced Considerations
Precision in Prosthesis Alignment as a Cornerstone of Rehabilitation Success
Achieving sub-millimeter accuracy in prosthesis positioning during hip replacement surgery is not merely a surgical goal but a fundamental determinant of rehabilitation outcomes. Optimal alignment minimizes aberrant joint loading, facilitates symmetrical gait patterns, and enhances proprioceptive feedback, thereby reducing the risk of prosthetic loosening and accelerating neuromuscular adaptation. The integration of intraoperative navigation and patient-specific instrumentation exemplifies how surgical precision directly translates to improved functional recovery.
Harnessing Neuroplasticity Through Customized Motor Learning Protocols
Rehabilitation that leverages central nervous system plasticity markedly improves post-arthroplasty functional outcomes. Task-specific training, variable practice, and augmented feedback—particularly when delivered via virtual reality platforms—stimulate cortical remapping and promote efficient motor relearning. This neurorehabilitation approach mitigates compensatory movement patterns, fosters symmetrical limb loading, and thus prevents secondary musculoskeletal complications.
Multimodal Monitoring and Dynamic Rehabilitation Adjustments
The use of advanced imaging techniques such as dynamic ultrasound elastography and biomarker assays including alpha-defensin enables early detection of complications and precise evaluation of soft tissue integrity. These diagnostic tools empower clinicians to tailor rehabilitation intensity and modalities responsively, optimizing recovery trajectories while minimizing risks. Such dynamic adjustments underscore the necessity of continuous multidisciplinary collaboration.
Psychosocial Integration as a Vital Component of Recovery
Beyond physical healing, addressing psychological resilience and social support systems through cognitive-behavioral therapy and patient education substantially enhances rehabilitation adherence and pain management. Recognizing and treating psychosocial factors as integral elements of postoperative care fosters holistic recovery and improved patient satisfaction.
Curated Expert Resources
- American Academy of Orthopaedic Surgeons (AAOS) Hip Replacement Rehabilitation Guidelines: Authoritative protocols that delineate evidence-based rehabilitation timelines and precautions, essential for clinicians optimizing postoperative care.
- Journal of Orthopaedic Research: Cutting-edge research articles exploring biomechanics, neurorehabilitation, and innovative therapies that deepen understanding of hip arthroplasty recovery.
- Frontiers in Neurology – Neuroplasticity and Motor Learning Reviews: Comprehensive analyses of CNS adaptations relevant to motor relearning strategies post-arthroplasty.
- Journal of Bone and Joint Surgery – Biomarker Developments: Clinical trial data and reviews on alpha-defensin and other biomarkers revolutionizing infection diagnosis in orthopedic implants.
- Advanced Orthopedic Rehab Tips After Lumbar Fusion Surgery (njorthopedicdoctor.xyz): While focused on lumbar fusion, this resource offers transferable insights into complex orthopedic rehabilitation principles applicable for hip replacement patients.
Final Expert Perspective
Hip replacement recovery is no longer confined to the mechanical restoration of joint function; it demands a sophisticated integration of surgical precision, neurophysiological adaptation, dynamic monitoring, and psychosocial support. The expert-level strategies discussed—from biomechanical alignment to virtual reality-enhanced neuroplasticity and biomarker-guided rehabilitation adjustments—collectively elevate patient outcomes beyond traditional paradigms. For orthopedic specialists and patients striving for excellence, embracing these multidisciplinary advances is imperative. We encourage further exploration of essential hip replacement orthopedic info for patients and invite practitioners to contribute their clinical insights to this evolving discourse, fostering innovation and improved standards of care.


The article’s emphasis on the complex interplay of biomechanics and neuroplasticity during hip replacement recovery really highlights how transformative modern rehabilitation has become. I recently went through a hip replacement, and what struck me most was the importance of early mobilization combined with carefully guided physiotherapy tailored to my specific needs. The discussion on proprioception restoration and gait biomechanics realignment resonates with my experience; it’s not just about healing the incision but retraining the entire muscle-joint coordination. I found that incorporating graduated weight-bearing exercises and neuromuscular re-education made a significant difference in my joint stability over time. One area I’d love to hear more about is how virtual reality-based motor training is being integrated in real-world rehab settings. Has anyone here tried such technology or know about its accessibility outside research centers? Also, balancing postoperative pain control without overusing opioids remains a crucial and delicate issue, and I appreciated the article’s insights into multimodal pain management. How do others find the coordination between orthopedic teams and pain specialists in creating personalized rehabilitation timelines that also consider psychological support? This multidisciplinary approach seems vital for long-term success in recovery.
This detailed overview of the recovery process highlights how much modern technology and multidisciplinary care have advanced postoperative rehabilitation. As someone who’s recently gone through a hip replacement, I found the emphasis on tailored physiotherapy and early mobilization spot on. I noticed during my recovery that integrating neuroplasticity principles, alongside traditional physiotherapy, really sped up my progress. The use of virtual reality in rehab, though still relatively new in many clinics, seems promising particularly for balance and proprioception training. Has anyone experienced difficulties accessing VR-based therapy outside research settings, especially in smaller centers? Also, managing pain without relying heavily on opioids is an ongoing challenge. I appreciated the mention of multimodal approaches like TENS and cryotherapy. How are other clinicians balancing pain control with functional goals while minimizing opioid use? Overall, this reinforces how essential a multidisciplinary and technology-driven approach is for successful long-term outcomes. I’d love to hear how some have navigated integrating these advanced methods into routine practice—any tips or lessons learned?
This article really underscores how multifaceted hip replacement recovery has become, especially with the integration of advanced technologies like wearable sensors and VR training. I had a similar experience where early mobilization and personalized physiotherapy made a noticeable difference in my healing process. The mention of neuroplasticity and motor learning principles being harnessed through VR really piqued my interest—I’ve been curious about how accessible these solutions are outside of research settings, especially for patients in rural or smaller clinics. Additionally, managing pain with multimodal approaches while avoiding overreliance on opioids remains a significant challenge. From your experience, how do teams coordinate to tailor rehab plans that balance these complexities? I believe this multidisciplinary, tech-enabled approach holds great promise, but understanding real-world limitations and pathways to broader implementation would be valuable. Has anyone here experienced hurdles in integrating these methods into everyday practice? Would love to hear insights from clinicians and patients alike.