When Pain Strikes, Who You Gonna Call? Hint: It’s Not Ghostbusters
Imagine this: You’re limping through your day, a sharp, nagging pain shooting through your joint like an unwelcome guest who just won’t leave. Orthopedic pain isn’t just a nuisance; it’s a persistent reminder that something’s amiss beneath the surface. For many, the anxiety of invasive surgery looms large. Enter nerve block orthopedic management, the unsung hero of pain relief that offers a trusted, targeted solution without the drama of the operating room.
Nerve Blocks: The Artful Dodger of Orthopedic Pain
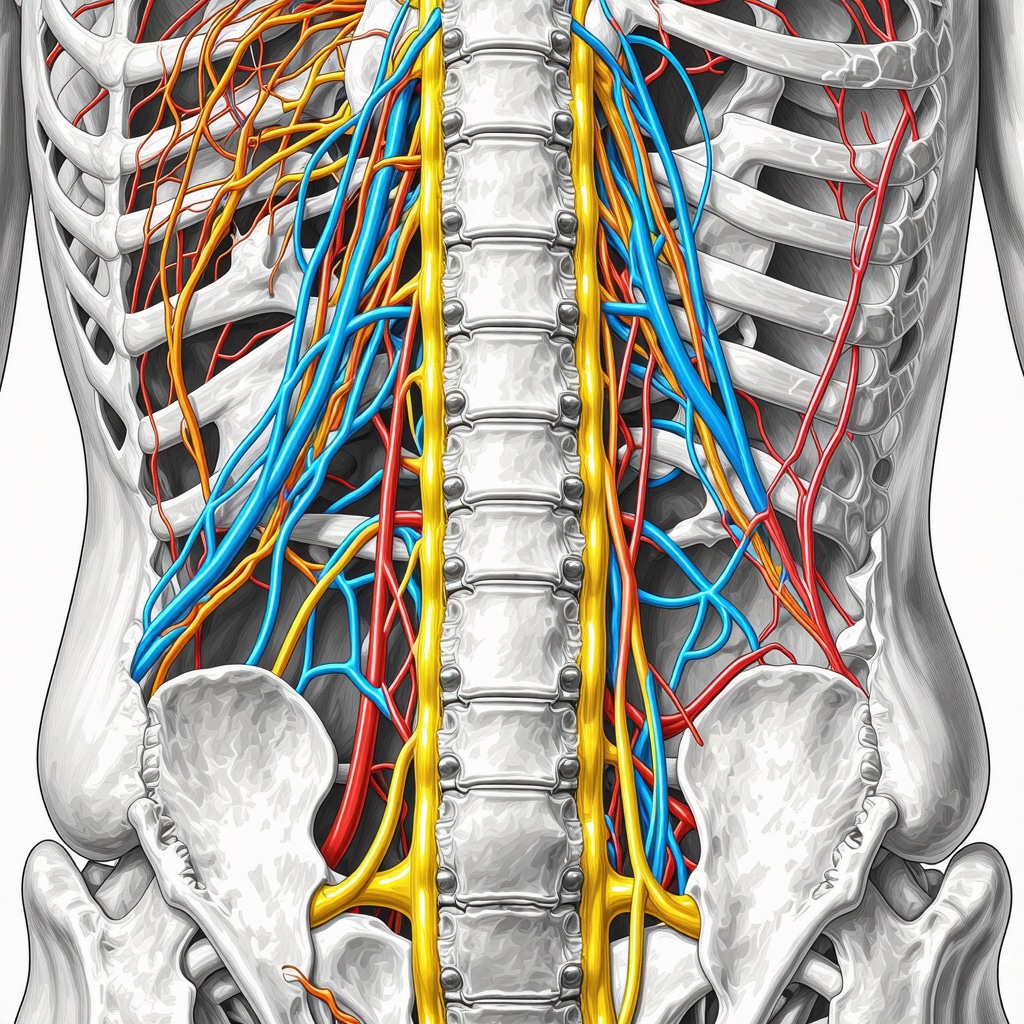
Nerve blocks are like the stealthy ninjas of orthopedic pain management. By precisely interrupting the pain signals traveling along specific nerves, they provide relief that’s both swift and effective. Whether it’s chronic back pain, joint inflammation, or post-surgical discomfort, nerve blocks can serve as a powerful tool in the orthopedic arsenal.
Is Blocking Pain Really Blocking Progress?
Here’s the million-dollar question: Could numbing the pain actually hinder your recovery? It’s a common misconception. Pain is a useful alarm bell, sure, but sometimes it’s more of a false alarm that keeps you sidelined unnecessarily. When applied judiciously, nerve blocks not only relieve suffering but also enable patients to engage more fully in physical therapy and rehabilitation — speeding up the journey back to normal life. It’s a nuanced dance, balancing pain control with healing, and that’s where expert orthopedic guidance shines.
Why Trust Nerve Blocks? The Science and Stories Behind the Relief
Beyond the anecdotes, nerve blocks have a robust foundation in medical science. According to a comprehensive review published in The Journal of Pain Research, these injections can significantly reduce pain and improve function in patients with orthopedic conditions. But it’s not just about numbers; it’s the personal stories — like that of a patient who finally returned to hiking after years of debilitating joint pain — that underscore their value.
Of course, nerve blocks aren’t a one-size-fits-all cure. They’re part of a multidisciplinary approach that often includes physical therapy, lifestyle adjustments, and sometimes surgical consultation. If you’re navigating orthopedic pain, understanding the full spectrum of options can empower you to make informed decisions. For insights into non-surgical care alternatives, check out this detailed guide on effective non-surgical care for herniated discs.
Ready to Take Control of Your Pain? Let’s Talk!
Have you or someone you know tried nerve blocks for orthopedic pain? What was your experience like? Share your thoughts and stories in the comments below — because sometimes, the best relief is knowing you’re not alone in this journey. And if you’re seeking expert advice tailored to your situation, don’t hesitate to contact an orthopedic specialist who can guide you through the best pain management strategies.
When Pain Strikes, Who You Gonna Call? Hint: It’s Not Ghostbusters
Imagine this: You’re limping through your day, a sharp, nagging pain shooting through your joint like an unwelcome guest who just won’t leave. Orthopedic pain isn’t just a nuisance; it’s a persistent reminder that something’s amiss beneath the surface. For many, the anxiety of invasive surgery looms large. Enter nerve block orthopedic management, the unsung hero of pain relief that offers a trusted, targeted solution without the drama of the operating room.
Nerve Blocks: The Artful Dodger of Orthopedic Pain
Nerve blocks are like the stealthy ninjas of orthopedic pain management. By precisely interrupting the pain signals traveling along specific nerves, they provide relief that’s both swift and effective. Whether it’s chronic back pain, joint inflammation, or post-surgical discomfort, nerve blocks can serve as a powerful tool in the orthopedic arsenal.
Is Blocking Pain Really Blocking Progress?
Here’s the million-dollar question: Could numbing the pain actually hinder your recovery? It’s a common misconception. Pain is a useful alarm bell, sure, but sometimes it’s more of a false alarm that keeps you sidelined unnecessarily. When applied judiciously, nerve blocks not only relieve suffering but also enable patients to engage more fully in physical therapy and rehabilitation — speeding up the journey back to normal life. It’s a nuanced dance, balancing pain control with healing, and that’s where expert orthopedic guidance shines.
Why Trust Nerve Blocks? The Science and Stories Behind the Relief
Beyond the anecdotes, nerve blocks have a robust foundation in medical science. According to a comprehensive review published in The Journal of Pain Research, these injections can significantly reduce pain and improve function in patients with orthopedic conditions. But it’s not just about numbers; it’s the personal stories — like that of a patient who finally returned to hiking after years of debilitating joint pain — that underscore their value.
Of course, nerve blocks aren’t a one-size-fits-all cure. They’re part of a multidisciplinary approach that often includes physical therapy, lifestyle adjustments, and sometimes surgical consultation. If you’re navigating orthopedic pain, understanding the full spectrum of options can empower you to make informed decisions. For insights into non-surgical care alternatives, check out this detailed guide on effective non-surgical care for herniated discs.
Ready to Take Control of Your Pain? Let’s Talk!
Have you or someone you know tried nerve blocks for orthopedic pain? What was your experience like? Share your thoughts and stories in the comments below — because sometimes, the best relief is knowing you’re not alone in this journey. And if you’re seeking expert advice tailored to your situation, don’t hesitate to contact an orthopedic specialist who can guide you through the best pain management strategies.
Beyond the Injection: Integrating Nerve Blocks into Comprehensive Orthopedic Care
While nerve blocks offer targeted pain relief, their greatest effectiveness emerges when combined with a holistic treatment plan. This includes physical therapy to strengthen muscles around affected joints and improve mobility, lifestyle modifications to reduce strain, and sometimes the strategic use of orthopedic injections for chronic back pain to manage flare-ups effectively. For those curious about the synergy between different treatments, exploring minimally invasive back pain treatments can shed light on how nerve blocks fit into broader pain management strategies.
What Are the Emerging Frontiers in Nerve Block Orthopedic Management?
As medical science advances, so do the techniques and applications of nerve blocks. Newer formulations and image-guided precision injections are enhancing the safety profile and efficacy, minimizing side effects, and extending the duration of relief. Additionally, research is exploring combining nerve blocks with regenerative medicine approaches such as platelet-rich plasma (PRP) therapy. These innovative combinations promise to not just mask pain temporarily but also promote tissue healing and long-term functional improvement.
Could Personalized Nerve Block Protocols Revolutionize Orthopedic Pain Relief?
With the rise of personalized medicine, one intriguing question emerges: Can nerve block protocols be tailored to individual patient profiles to optimize outcomes? Factors such as genetic markers, pain sensitivity, and lifestyle may soon guide customized treatment plans. This approach could maximize pain control while minimizing risks, ultimately transforming how orthopedic pain is managed. As highlighted by experts in multidisciplinary orthopedic care models, integrating patient-specific data into treatment algorithms is a promising frontier.source
Share Your Insights and Discover More
If you found this exploration of nerve block orthopedic pain management insightful, share this article with your network to spread awareness about these innovative pain relief options. Have you experienced nerve blocks or other advanced orthopedic treatments? Join the conversation by commenting below and help others navigate their pain management journey. For a deeper dive into related topics, consider reading about orthopedic injection techniques for chronic back pain to broaden your understanding of available therapies.
Precision in Practice: How Image-Guided Nerve Blocks Enhance Orthopedic Outcomes
In the realm of orthopedic pain management, precision is paramount. The evolution from blind injections to modern image-guided nerve blocks has dramatically improved both safety and efficacy. Utilizing ultrasound or fluoroscopic guidance, clinicians can visually confirm needle placement in real-time, targeting the exact nerve structures responsible for pain transmission. This advancement not only increases the likelihood of successful pain interruption but also minimizes risks such as nerve damage or inadvertent vascular injection.
For example, ultrasound-guided nerve blocks have been shown to reduce procedural pain and increase patient comfort, while enabling dynamic assessment of anatomical variations that could complicate traditional approaches. Such precision is especially critical when addressing complex joint pain like that from the shoulder’s suprascapular nerve or the intricate lumbar plexus branches involved in lower back discomfort.
How Does Image Guidance Improve the Safety and Effectiveness of Nerve Blocks in Orthopedics?
Image guidance allows clinicians to navigate the intricate anatomy surrounding nerve targets with unparalleled clarity. This reduces the risk of complications such as hematoma, nerve injury, or inadvertent intravascular injection. Furthermore, precise delivery ensures that the anesthetic or corticosteroid agents reach the intended location, optimizing pain relief duration and functional recovery. A systematic review published in Anesthesiology Clinics confirms that ultrasound-guided peripheral nerve blocks improve success rates and patient satisfaction compared to landmark techniques.
Synergizing Therapies: Combining Nerve Blocks with Regenerative Medicine for Enhanced Orthopedic Repair
Beyond mere symptom control, the future of nerve block orthopedic management lies in integration with regenerative medicine approaches. Platelet-rich plasma (PRP) and stem cell therapies are gaining traction for their potential to stimulate tissue repair and modulate inflammatory pathways. Emerging clinical protocols are exploring concurrent administration of nerve blocks with PRP injections to not only alleviate pain but also encourage biological healing of damaged ligaments, tendons, and cartilage.
This dual-action strategy aims to shorten recovery times and improve functional outcomes, particularly in degenerative conditions such as osteoarthritis or chronic tendinopathies. While still under investigation, preliminary studies suggest that combining nerve blocks with regenerative treatments may reduce the need for surgical intervention, offering a less invasive yet comprehensive therapeutic option.
Personalized Pain Management: Customizing Nerve Block Protocols Through Genetic and Lifestyle Insights
The concept of personalized medicine is reshaping orthopedic pain management paradigms. Recent research highlights that factors including genetic predisposition to pain sensitivity, metabolic profiles, and patients’ activity levels can influence both the efficacy and duration of nerve block analgesia. By incorporating these variables into treatment planning, specialists can tailor drug selection, dosage, and injection sites to the individual’s unique physiology.
For instance, polymorphisms in genes related to opioid receptors or inflammatory cytokines might predict differential responses to anesthetics or corticosteroids used in nerve blocks. Similarly, understanding a patient’s daily physical demands and comorbidities can guide the timing and frequency of injections to maximize functional gains while minimizing side effects.
Such personalization necessitates a multidisciplinary approach, combining genetic counseling, detailed patient history, and advanced imaging. As noted in a recent publication in Frontiers in Pharmacology, integrating precision medicine into nerve block protocols holds promise to revolutionize orthopedic pain control by optimizing outcomes and patient satisfaction.
Challenges and Considerations: Addressing Limitations in Nerve Block Orthopedic Management
While the promise of nerve blocks is undeniable, several challenges persist. One such limitation is the transient nature of relief offered by local anesthetics and corticosteroids, often necessitating repeat procedures. Additionally, patient-specific factors such as coagulopathy, infection risk, or allergies may contraindicate certain nerve block techniques or agents.
Moreover, the psychological component of pain should not be overlooked. Chronic orthopedic pain often involves central sensitization and psychosocial influences that nerve blocks alone cannot fully address. Hence, comprehensive management must integrate cognitive-behavioral therapy and patient education to achieve sustainable improvement.
What Are the Key Factors Limiting Long-Term Success of Nerve Blocks in Orthopedic Pain?
Key limitations include the temporary duration of analgesia, potential adverse effects of repeated corticosteroid use, and the multifactorial nature of chronic pain syndromes which may involve central nervous system changes beyond peripheral nerve input. Furthermore, variability in patient anatomy and comorbidities can impact procedural success rates. Addressing these challenges requires a holistic treatment framework and ongoing research into novel agents and delivery methods that extend analgesic duration and promote tissue regeneration.
Precision Meets Innovation: Navigating the Complexities of Advanced Nerve Block Techniques
Orthopedic pain management is no longer a one-dimensional pursuit. Cutting-edge advancements in nerve block procedures now emphasize not just pain suppression but also enhancing patient-specific recovery trajectories. Techniques such as ultrasound and fluoroscopic image guidance have revolutionized the precision of nerve targeting, reducing complications and improving therapeutic outcomes. These innovations empower clinicians to address even the most intricate anatomical variations, tailoring interventions to the unique neuroanatomy of each patient.
For those grappling with complex conditions like refractory facet joint pain or multifocal lumbar radiculopathies, combining image-guided nerve blocks with adjunctive therapies can offer a nuanced pathway toward sustained relief. To explore how these minimally invasive interventions fit into broader treatment paradigms, consider reading about minimally invasive back pain treatments.
Synergistic Strategies: How Combining Therapies Enhances Orthopedic Pain Outcomes
Integrating nerve blocks with complementary modalities such as regenerative medicine, physical rehabilitation, and lifestyle optimization is rapidly becoming the gold standard. For example, coupling nerve blocks with platelet-rich plasma (PRP) injections or stem cell therapies may potentiate tissue repair processes while mitigating inflammation-driven pain. This multimodal approach not only targets symptomatic relief but also addresses underlying pathologies, potentially reducing long-term disability.
Furthermore, incorporating tailored physical therapy post-nerve block can optimize functional restoration by leveraging the window of analgesia to enhance mobility and muscle strength. For expert-guided orthopedic rehabilitation insights, visit orthopedic rehab tips after lumbar fusion surgery.
What Role Does Personalized Medicine Play in Optimizing Nerve Block Efficacy?
As precision medicine gains momentum, the concept of customizing nerve block protocols according to individual genetic profiles, pain phenotypes, and lifestyle factors is reshaping orthopedic care. Recent studies have shown that genetic polymorphisms affecting inflammatory mediators and anesthetic metabolism can influence both the intensity and duration of analgesic response.source This emerging knowledge allows clinicians to select tailored anesthetic agents, dosing, and injection sites, thereby maximizing efficacy and limiting adverse effects.
Moreover, lifestyle considerations such as occupational physical demands and comorbid conditions like diabetes or obesity are increasingly factored into treatment planning, ensuring that nerve block interventions harmonize with the patient’s overall health context and rehabilitation goals.
Addressing the Psychological Dimension: Integrating Mind-Body Approaches with Nerve Block Therapy
Chronic orthopedic pain is not merely a physical phenomenon; it encompasses emotional and cognitive dimensions that can profoundly influence treatment outcomes. Incorporating cognitive-behavioral therapy (CBT), mindfulness, and patient education alongside nerve block protocols helps mitigate central sensitization and fosters adaptive coping strategies.
This holistic perspective encourages patients to view nerve blocks as a component of a comprehensive pain management strategy rather than a standalone solution. Such integration enhances resilience and empowers patients to actively participate in their recovery journey.
Join the Conversation: Share Your Experience and Explore Expert Resources
Have you benefited from personalized nerve block strategies or combined orthopedic treatments? Your insights could illuminate the path for others navigating complex pain management decisions. Share your stories and questions in the comments below, or reach out directly to connect with an orthopedic specialist for individualized guidance tailored to your unique needs.
To further deepen your understanding of comprehensive orthopedic care, explore our detailed resource on effective non-surgical care for herniated discs. Together, let’s advance the conversation on innovative, patient-centered orthopedic pain relief.
Expert Insights & Advanced Considerations
The Nuanced Role of Image-Guided Nerve Blocks in Complex Anatomy
Precision in nerve block administration has evolved beyond traditional landmark techniques. Utilizing ultrasound or fluoroscopy enables targeting intricate nerve pathways with exceptional accuracy, reducing complications and enhancing efficacy. This is especially critical for multifaceted conditions such as refractory facet joint pain or suprascapular nerve entrapments, where anatomy varies considerably among patients.
Integrating Regenerative Medicine to Extend and Enhance Therapeutic Benefits
Combining nerve blocks with regenerative therapies like platelet-rich plasma (PRP) or stem cell injections presents a promising frontier. This synergy not only mitigates pain but also fosters biological repair, potentially reducing the need for invasive surgery. Early clinical protocols suggest improved functional outcomes and shortened recovery timelines when these modalities are used in tandem.
Personalizing Nerve Block Protocols Through Genetic and Lifestyle Profiling
Emerging evidence underscores the importance of tailoring nerve block treatments based on individual genetic markers, metabolic factors, and daily activity demands. Such personalization can optimize drug selection, dosage, and injection frequency, maximizing analgesic effects while minimizing adverse reactions. This approach aligns with the broader trend toward precision medicine in orthopedic pain management.
Addressing the Psychological Component for Sustainable Pain Control
Chronic orthopedic pain often involves central sensitization and psychosocial influences that nerve blocks alone cannot resolve. Integrating cognitive-behavioral therapy, mindfulness, and patient education alongside nerve block interventions facilitates a holistic recovery process, empowering patients to manage pain more effectively over the long term.
Strategic Multimodal Approaches to Optimize Functional Recovery
Employing nerve blocks within a multidisciplinary framework — including physical therapy, lifestyle modification, and selective orthopedic injections — enhances rehabilitation potential. This coordinated care model leverages the analgesic window provided by nerve blocks to improve mobility, muscle strength, and overall patient outcomes.
Curated Expert Resources
- The Journal of Pain Research: Offers comprehensive peer-reviewed studies on nerve block efficacy and pain modulation strategies, essential for evidence-based practice.
- Anesthesiology Clinics: Features systematic reviews on ultrasound-guided nerve block techniques, highlighting advances in procedural safety and patient satisfaction.
- Minimally Invasive Back Pain Treatments Explained: A practical guide contextualizing nerve blocks within broader minimally invasive orthopedic interventions.
- Effective Non-Surgical Care for Herniated Discs: Offers insights into complementary non-surgical modalities that synergize with nerve block management.
- Orthopedic Rehab Tips After Lumbar Fusion Surgery: Provides expert advice on optimizing rehabilitation post-nerve block analgesia.
Final Expert Perspective
In navigating the complexities of orthopedic pain, nerve block management stands out as a refined, adaptable tool that transcends mere symptom suppression. The integration of image-guidance, regenerative adjuncts, and personalized protocols marks a significant leap forward, offering patients tailored pathways to relief and functional restoration. Yet, the true power of nerve blocks unfolds within a comprehensive, multidisciplinary framework that addresses physical, biological, and psychological dimensions of pain.
For those committed to advancing their understanding or seeking individualized guidance, engaging with orthopedic specialists remains paramount. Explore expert consultation options to tailor pain management strategies effectively. Delve deeper into related approaches such as non-surgical care for herniated discs and minimally invasive back pain treatments to broaden your orthopedic care perspective.
Your journey toward informed, effective orthopedic pain management is ongoing — and the advancing landscape of nerve block therapy offers both hope and tangible options to reclaim quality of life.

I really appreciate how this article highlights nerve blocks as a smart alternative to surgery for managing orthopedic pain. Having dealt with chronic knee inflammation myself, I was initially wary of relying on injections because I thought masking the pain might make me ignore my body’s signals and worsen the injury. However, after receiving a series of ultrasound-guided nerve blocks combined with physical therapy, I found it actually accelerated my rehabilitation. The pain relief allowed me to engage more confidently in exercises that strengthened my muscles and improved my knee function without the lingering fear of intense pain.
What struck me as especially valuable is the emphasis on a multidisciplinary approach—nerve blocks are not a magic bullet but a tool to be integrated thoughtfully along with therapies addressing the physical and psychological aspects of pain. I’m curious if others have noticed differences in recovery depending on how personalized their nerve block protocols are? For those who’ve undergone these treatments, how did your care teams tailor the nerve blocks or accompanying therapies to your specific needs and lifestyle? I’d love to hear how personalization influenced your outcomes or if anyone has insights on advancements in combining nerve blocks with regenerative treatments like PRP.
This article provides a really insightful look into how nerve blocks can be a game-changer for many dealing with persistent orthopedic pain. I’ve had personal experience with nerve blocks for post-op knee pain, and I agree that when done correctly, especially with image guidance, they can significantly improve quality of life without the need for invasive surgery. What caught my attention is the potential for combining nerve blocks with regenerative therapies like PRP, which seems to not only manage pain but also encourage healing at a tissue level. From what I’ve read, this could be especially beneficial in degenerative conditions where tissue repair is key. Have any readers here tried integrating regenerative medicine with nerve blocks? I wonder what the long-term outcomes look like and how accessible these combined treatments are in general practice. It’s exciting to think that future protocols might be even more personalized, taking into account genetic factors and lifestyle, as mentioned in the article. How do others see this evolving, and what are some challenges in making these advanced therapies widely available? I’d love to hear more insights from practitioners or patients who have experienced these innovative approaches.
Reading this post made me reflect on how nerve blocks truly are a nuanced, yet powerful, option for managing persistent orthopedic pain. I’ve personally undergone multiple nerve block procedures for lower back pain, and I can attest to how targeted relief can make a real difference, especially when combined with physical therapy. The article’s point on combining image-guided techniques with regenerative approaches like PRP is quite promising. In my experience, precise delivery, especially under ultrasound guidance, not only improves safety but also enhances the overall effectiveness of the treatment. I wonder, how do practitioners determine the ideal combination of nerve blocks with regenerative treatments for individual patients? Are there specific markers or indicators that guide this personalized approach? It’s fascinating to see how advances like this are shifting the landscape toward more tailored, less invasive therapies that can improve long-term outcomes. I’d love to hear from others who have experienced or are considering these integrated strategies, especially regarding their recovery journeys.
This article sheds important light on nerve blocks as a versatile and targeted pain management option. I’ve personally seen how image-guided nerve blocks, especially when used in conjunction with regenerative treatments like PRP, can really make a difference in patient recovery times and long-term outcomes. One point that stands out is the emphasis on personalized protocols—considering genetic factors and lifestyle, which seems like a huge leap towards more tailored care. I wonder how often practitioners are able to incorporate genetic testing into routine pain management strategies? Also, in your experience, what are some practical challenges in shifting towards these more personalized, less invasive methods on a wider scale? Personally, I believe that training and access to advanced imaging are key barriers that need addressing for broader implementation. Would love to hear more about how clinics are overcoming these hurdles and what the future holds for combining precision medicine with orthopedic pain therapies.