When Your Nerves Throw a Tantrum: The Orthopedic Non-Surgical Playbook
Picture this: your hand suddenly tingles like it’s been stuck in a bucket of ice, or your back starts whispering (read: shouting) with nerve pain. Nerve compression isn’t just a fancy medical term; it’s a daily reality for millions, and the thought of surgery can send chills down anyone’s spine. But fear not, the world of orthopedic care isn’t all scalpels and stitches. There’s a treasure trove of non-surgical treatments that can soothe those rebellious nerves without the drama of the operating room.
Why Skip the Knife? Because Non-Surgical Nerve Compression Treatments Are More Than Just Placebos
Orthopedic medicine has evolved, and with it, the understanding that surgery is not always the answer. Non-surgical treatments like physical therapy, nerve blocks, and ergonomic adjustments often provide relief and restore function. For example, targeted nerve block therapies can calm inflammation and pain without the risks surgery entails.
Is It Really Possible to Untangle Nerve Compression Without Surgery?
Absolutely! The key lies in early diagnosis and a tailored treatment plan. Physical therapy focuses on strengthening muscles to relieve pressure on nerves, while ergonomic interventions correct posture and reduce repetitive strain. Additionally, orthopedic injections can offer quick relief, giving patients a chance to heal naturally.
Real Stories, Real Relief: A Personal Glimpse into Non-Surgical Triumphs
Take Jane, a desk worker whose carpal tunnel syndrome made typing a nightmare. With a blend of splinting, nerve gliding exercises, and ergonomic tweaks, she avoided surgery and returned to work pain-free. Stories like hers underscore why effective nerve compression treatment today leans heavily on conservative management first.
Trust But Verify: Where Does Science Stand on These Treatments?
According to a 2021 review published in the Journal of Orthopedic Research, non-surgical interventions for nerve compression syndromes show significant improvement in pain and functionality for most patients, especially when started early (source). This reinforces the orthopedic community’s shift toward conservative care and patient-centric approaches.
Curious how to navigate these options yourself? Explore the nuances of non-surgical nerve compression treatments and share your experiences or questions below. After all, your journey through nerve pain is worth a conversation.
Exploring Cutting-Edge Conservative Therapies for Nerve Compression
The landscape of orthopedic care is constantly evolving, embracing innovations that refine non-surgical options for nerve compression syndromes. Beyond traditional physical therapy and nerve blocks, advanced modalities such as ultrasound-guided hydrodissection and regenerative medicine techniques like platelet-rich plasma (PRP) injections are gaining traction. These treatments aim not only to relieve pain but also to address underlying tissue abnormalities, promoting long-term nerve health.
What Are the Emerging Non-Surgical Techniques Changing Orthopedic Nerve Care in 2024?
In 2024, orthopedic specialists are increasingly integrating minimally invasive interventions that enhance precision and efficacy. Ultrasound-guided hydrodissection involves the careful separation of nerve adhesions using fluid injection, which can reduce nerve entrapment without surgery. Concurrently, regenerative therapies like PRP are being studied for their potential to accelerate healing by delivering concentrated growth factors to damaged nerve areas.
These approaches represent a paradigm shift, emphasizing tissue repair and functional restoration. For patients hesitant about surgery, these options expand the therapeutic arsenal, offering hope for durable relief. A detailed discussion on these innovative treatments can be found in resources covering minimally invasive back pain treatments.
Integrating Multidisciplinary Care: The Key to Successful Non-Surgical Outcomes
Effective management of nerve compression often demands a multidisciplinary approach. Orthopedic physicians collaborate with physical therapists, pain specialists, and occupational therapists to create personalized care plans. This alliance ensures that interventions such as ergonomic modifications, tailored exercise regimens, and pain management strategies work synergistically. This comprehensive model not only improves symptom control but also addresses lifestyle factors contributing to nerve stress.
Patients benefit from this holistic framework as it caters to both symptom relief and prevention. For instance, physical therapy not only eases nerve irritation but also strengthens supporting musculature, decreasing future injury risk. Moreover, ergonomic counseling helps modify daily activities that may exacerbate nerve compression, a critical step for those with repetitive strain injuries.
How Do Non-Surgical Treatments Impact Long-Term Nerve Function and Quality of Life?
Beyond immediate symptom control, non-surgical treatments can profoundly influence long-term nerve function and patient quality of life. Research published by the American Academy of Orthopaedic Surgeons emphasizes that early conservative care correlates with better functional outcomes and reduced need for surgery (source). These findings underscore the importance of timely intervention and adherence to prescribed regimens.
Additionally, patients engaged in conservative care often report enhanced mobility and reduced disability, enabling them to maintain work and social activities. This holistic benefit highlights the critical role of orthopedic specialists in guiding patients through evidence-based, personalized treatment plans.
For those navigating nerve compression challenges, sharing your experiences or questions can provide valuable insights to others facing similar issues. Feel free to comment below or explore more about personalized orthopedic care at our contact page to connect with experts who can tailor treatments to your needs.
Precision in Practice: How Ultrasound Guidance Revolutionizes Non-Surgical Nerve Care
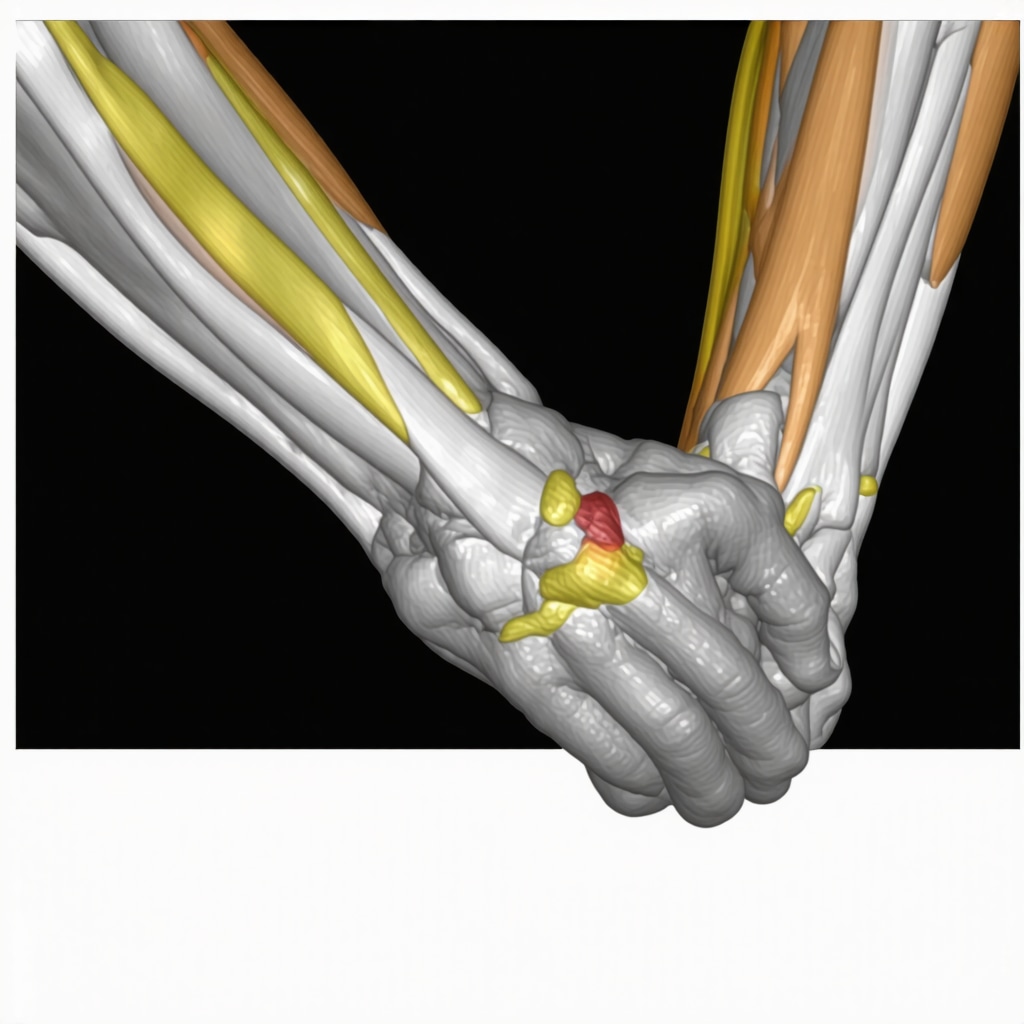
Ultrasound-guided interventions have transformed the landscape of conservative nerve compression treatment by offering unparalleled precision. Unlike blind injections, ultrasound visualization allows orthopedic specialists to identify nerve entrapments, surrounding fibrotic tissue, and vascular structures in real-time. This capability ensures that treatments such as hydrodissection or corticosteroid injections are delivered exactly where needed, minimizing risks and maximizing efficacy.
Hydrodissection, specifically, employs fluid to gently separate nerve adhesions, freeing compressed nerves without the need for incisions. The technique’s minimally invasive nature and immediate symptom relief potential have made it a cornerstone in managing conditions like carpal tunnel syndrome and cubital tunnel syndrome. Moreover, ultrasound guidance enhances patient safety by reducing inadvertent nerve injury and improving patient comfort during procedures.
What Are the Biomechanical Mechanisms Behind Ultrasound-Guided Hydrodissection’s Effectiveness?
Hydrodissection works by mechanically disrupting perineural fibrosis and adhesions that tether nerves, restoring their gliding capacity within anatomical tunnels. This biomechanical liberation reduces aberrant nerve stretch and compression during limb movement, directly alleviating neuropathic symptoms. Additionally, the injected fluid may dilute inflammatory mediators around the nerve, contributing to pain reduction. Emerging studies suggest that repeated sessions can promote remodeling of scar tissue, offering sustained improvements beyond immediate decompression.
For a comprehensive review of hydrodissection’s applications and biomechanical rationale, refer to the detailed analysis published in the Journal of Orthopaedic & Sports Physical Therapy (source).
Regenerative Medicine: Platelet-Rich Plasma and Beyond in Nerve Compression Treatment
Regenerative orthopedics is pushing boundaries by focusing on tissue repair and nerve regeneration rather than mere symptom control. Platelet-rich plasma (PRP), derived from autologous blood, delivers concentrated growth factors such as platelet-derived growth factor (PDGF) and vascular endothelial growth factor (VEGF) directly to affected nerves. These bioactive molecules stimulate angiogenesis, reduce inflammation, and enhance axonal regeneration.
Clinical trials investigating PRP for peripheral nerve entrapments have reported significant improvements in pain and functional scores, sometimes comparable to surgical outcomes. However, standardizing PRP preparation and dosing remains a challenge, requiring individualized protocols tailored by experienced clinicians. Emerging adjuncts like stem cell therapies and extracellular vesicles are also under exploration for their potential synergistic effects in nerve healing.
How Does PRP Compare to Traditional Conservative Treatments in Long-Term Nerve Recovery?
While physical therapy and ergonomic modifications primarily address mechanical contributors to nerve compression, PRP targets the biological milieu, promoting intrinsic nerve repair. Studies indicate that PRP injections can accelerate recovery times and improve nerve conduction velocities when combined with conventional therapies. Nonetheless, PRP is not a panacea and is best integrated into a multimodal treatment plan. Ongoing randomized controlled trials aim to delineate patient selection criteria and optimize treatment algorithms.
Customized Orthopedic Care: Integrating Patient-Specific Factors for Optimal Outcomes
Not all nerve compression cases are identical, and thus, treatment must be tailored to individual patient profiles. Factors such as nerve injury chronicity, comorbidities like diabetes, occupational demands, and psychosocial stressors influence therapeutic responsiveness. Advanced diagnostic tools, including nerve conduction studies and high-resolution imaging, inform treatment personalization.
Moreover, patient education on lifestyle modifications, activity pacing, and ergonomic adaptations underpins successful conservative management. Orthopedic experts often incorporate cognitive-behavioral strategies to address pain perception and improve adherence. This holistic approach ensures not only symptom alleviation but also empowerment and sustained functional restoration.
Engage with us to explore how cutting-edge, patient-centric orthopedic nerve compression treatments can be tailored to your unique condition. Visit our contact page to consult with specialists who combine precision medicine and regenerative technologies for your benefit.
Beyond Basics: Harnessing Technology and Biology for Nerve Compression Mastery
As orthopedic care advances, the synergy of technology and biology is redefining how we approach nerve compression syndromes without surgery. The integration of ultrasound precision with regenerative medicine not only alleviates symptoms but also fosters intrinsic nerve healing. This convergence marks a critical leap from symptom management to true restoration.
How Are Patient-Specific Diagnostics Shaping the Future of Non-Surgical Nerve Treatments?
Contemporary care increasingly relies on nuanced diagnostics such as high-resolution ultrasound elastography and advanced nerve conduction studies. These modalities allow clinicians to quantify nerve stiffness, identify subtle entrapments, and tailor interventions with unprecedented accuracy. For example, elastography can detect early fibrotic changes that precede overt compression, enabling preemptive hydrodissection or targeted PRP injections. This level of precision aligns treatment with individual pathophysiology rather than a one-size-fits-all model, optimizing outcomes and minimizing unnecessary interventions.
Such innovations complement holistic approaches encompassing ergonomic counseling and cognitive-behavioral techniques, as highlighted in non-surgical nerve compression treatments. This precision medicine paradigm embodies the future of orthopedic nerve care.
Decoding the Role of Neuroplasticity in Conservative Nerve Compression Rehabilitation
Orthopedic specialists are increasingly appreciating the nervous system’s ability to adapt—neuroplasticity—in guiding recovery from nerve compression. Rehabilitation protocols now incorporate neuromodulatory exercises and graded sensory retraining designed to recalibrate brain and spinal cord processing of nerve signals. This cognitive-motor integration can reduce chronic pain perception and improve functional use despite persistent structural abnormalities.
Can Neuroplasticity-Based Therapies Reduce the Need for Surgical Intervention in Chronic Cases?
Emerging evidence suggests that neuroplasticity-informed therapies may significantly decrease surgery rates by enhancing symptom control and functional restoration. A 2023 systematic review in Neuroscience Advances reports that patients undergoing sensory discrimination training and mirror therapy experienced notable reductions in neuropathic pain and improved nerve conduction parameters (source). These therapies leverage the brain’s plasticity to diminish maladaptive pain circuits, offering a powerful adjunct to mechanical decompression strategies.
Incorporating these insights into a multidisciplinary framework, alongside physical therapy and regenerative treatments, can provide a comprehensive arsenal for managing even stubborn nerve compression syndromes.
Why Does Individualized Patient Engagement Matter More Than Ever in Non-Surgical Orthopedic Care?
Beyond technical innovations, the human element remains paramount. Patient adherence to therapy, lifestyle modifications, and psychological readiness profoundly influence outcomes. Orthopedic clinicians now emphasize personalized education, motivational interviewing, and shared decision-making to empower patients. This engagement fosters trust and compliance, critical for sustained improvement.
If you are navigating nerve compression challenges, consider reaching out for a bespoke consultation that integrates cutting-edge diagnostics and therapies tailored to your unique needs. Visit our contact page to connect with specialists who prioritize your journey toward recovery.
We invite readers to share your experiences or questions about advanced non-surgical nerve compression treatments below—your insights enrich this vital conversation.
Expert Insights & Advanced Considerations
Ultrasound-Guided Precision Elevates Non-Surgical Outcomes
Leveraging real-time ultrasound imaging for interventions such as hydrodissection and corticosteroid injections dramatically improves treatment accuracy. This precision not only minimizes procedural risks but also enhances therapeutic efficacy by targeting nerve entrapments directly, a critical advancement over traditional blind injection methods.
Regenerative Medicine Is Shaping the Future of Nerve Healing
Platelet-rich plasma (PRP) and emerging biological therapies transcend symptom relief by actively promoting nerve tissue repair and regeneration. Integrating these modalities into multimodal treatment protocols aligns with a paradigm shift from mere decompression to intrinsic nerve restoration, offering promising long-term functional improvements.
Neuroplasticity-Informed Rehabilitation Reduces Chronic Pain and Surgery Rates
Incorporating sensory retraining and neuromodulatory exercises taps into the nervous system’s adaptive capacity to recalibrate pain processing. These strategies complement mechanical decompression, potentially lowering the necessity for invasive surgery and enhancing patient quality of life through central nervous system reeducation.
Personalized Orthopedic Care Must Account for Multifactorial Patient Profiles
Successful conservative management hinges on tailoring interventions to individual factors such as injury chronicity, metabolic health, occupational demands, and psychosocial elements. Advanced diagnostics and patient engagement strategies ensure precision medicine principles translate into meaningful clinical improvements.
Multidisciplinary Collaboration Enhances Treatment Synergy and Compliance
The orchestration of orthopedic physicians, physical therapists, pain specialists, and occupational therapists creates a comprehensive framework addressing both biomechanical and behavioral contributors to nerve compression. This integrated approach fosters adherence and optimizes functional restoration.
Curated Expert Resources
- Journal of Orthopaedic & Sports Physical Therapy: Offers in-depth biomechanical analyses and clinical evidence on ultrasound-guided hydrodissection techniques, essential for understanding the mechanistic basis of precision interventions (source).
- American Academy of Orthopaedic Surgeons (AAOS) OrthopaInfo: A comprehensive patient and clinician resource outlining evidence-based standards and guidelines for conservative nerve compression management (source).
- Neuroscience Advances: Publishes cutting-edge reviews on neuroplasticity and rehabilitation strategies, providing critical insight into sensory retraining and pain modulation (source).
- Minimally Invasive Back Pain Treatments Explained: An accessible guide detailing emerging orthopedic interventions including ultrasound-guided procedures and regenerative therapies, perfect for clinicians and informed patients (read more).
- Nerve Block Orthopedic Management Techniques and Benefits: A focused discussion on targeted nerve blocks as a cornerstone conservative treatment, highlighting safety and efficacy (learn more).
Final Expert Perspective
Non-surgical nerve compression treatment in orthopedics is evolving beyond traditional boundaries—embracing precision imaging, regenerative biology, and neuroplasticity-informed rehabilitation to redefine patient outcomes. This holistic, patient-centric approach integrates multidisciplinary expertise and cutting-edge diagnostics to deliver personalized care that respects the complexity of nerve pathophysiology and individual patient needs. For those navigating this journey, engaging with specialized orthopedic professionals who leverage these advanced modalities is paramount to achieving durable relief and functional restoration.
We encourage practitioners and patients alike to deepen their understanding, share clinical experiences, and explore further resources such as our contact page to connect with experts dedicated to pioneering non-surgical nerve compression solutions tailored to your unique condition.


This article really captures the hopeful shift toward conservative, patient-centered care. I’m a desk worker and a few years ago developed early carpal tunnel symptoms—tingling at night and a weak pinch. My team’s approach (splinting, nerve-gliding exercises, focused physical therapy and ergonomic keyboard adjustments) made a big difference and let me avoid surgery. Reading about ultrasound-guided hydrodissection and PRP in this post was eye-opening because those weren’t widely discussed when I was treated.
One practical takeaway I’d offer: insist on objective testing (nerve conduction studies or high-resolution ultrasound) early so you can tailor treatment rather than guessing. I’m curious if others have personal experience with hydrodissection or PRP—did you notice faster functional recovery, and how many sessions were needed? Also, has anyone tried neuroplasticity-informed sensory retraining alongside mechanical treatments, and did it change outcomes?
Would love to hear which combination of diagnostics and conservative therapies practitioners on this forum find most reliably helps desk-bound patients return to full function.
This post highlights how crucial early diagnosis and a multidisciplinary approach are when tackling nerve compression issues. I appreciate the mention of ultrasound-guided hydrodissection and PRP—they really seem to be game-changers in minimally invasive care. From my experience working with patients suffering from peripheral nerve entrapments, combining physical therapy with regenerative treatments often produces more durable results than traditional methods alone.
One challenge I see, though, is standardizing PRP protocols for nerve healing, as the preparation can vary significantly between clinics. Has anyone here noticed differences in outcomes based on the PRP concentration or activation methods? Additionally, integrating neuroplasticity-based therapies seems promising, but I wonder how many patients adhere to sensory retraining routines long-term.
It makes me wonder, what strategies have others found effective in encouraging sustained engagement with these advanced rehabilitation techniques? Do they significantly reduce the need for surgical intervention once integrated early in treatment? I’d love to hear more insights from those who have seen particular success combining these modalities.
I really appreciate how this article emphasizes the importance of early intervention and a multidisciplinary approach for nerve compression issues. As someone who has dealt with chronic nerve pain from repetitive strain injuries, I can say that combining regenerative therapies like PRP with targeted physical therapy has made a noticeable difference in my recovery process. Ultrasound-guided hydrodissection was new to me, but hearing about its biomechanical effects gives me hope for those with more stubborn cases. I’ve found that consistent, patient-specific rehab, along with education on ergonomics, can help prevent future flare-ups. Has anyone experienced long-term relief with these minimally invasive treatments, and how do they compare to surgical options in terms of durability? Understanding these options better really helps empower patients to make informed choices about their care.