Unlocking the Mysteries of Nerve Compression: Why Timely Orthopedic Care Matters
Nerve compression, often manifesting as persistent pain, numbness, or tingling sensations, can significantly disrupt daily life. Orthopedic specialists play a pivotal role in diagnosing and treating these conditions, offering solutions that not only alleviate symptoms but also address the root causes. Understanding the complexities of nerve compression syndromes is essential for effective treatment and long-term recovery.
Innovative Orthopedic Treatments: Beyond Conventional Pain Relief
Modern orthopedic care for nerve compression has evolved beyond temporary symptom management. Techniques such as targeted nerve blocks, minimally invasive decompression surgeries, and personalized rehabilitation plans are transforming patient outcomes. For example, electromyography (EMG) and nerve conduction studies (NCS) enable precise identification of nerve impairment extent, guiding tailored interventions. These advances reduce recovery times and improve functional restoration.
How Do Orthopedic Experts Determine the Best Nerve Compression Treatment?
Determining the optimal treatment requires a comprehensive assessment that integrates clinical evaluation with advanced diagnostic tools. Orthopedic doctors consider factors like the compression site, severity, patient activity levels, and overall health. Non-surgical approaches such as physical therapy, ergonomic adjustments, and support braces are often first-line treatments. When these measures are insufficient, minimally invasive surgical options become viable, aiming to relieve pressure while preserving surrounding tissue integrity.
Case Study Spotlight: Real-World Success Stories in Orthopedic Nerve Care
Consider the case of a middle-aged patient with carpal tunnel syndrome resistant to conservative therapy. After thorough nerve conduction testing, the orthopedic team performed a targeted endoscopic release, enabling rapid symptom resolution and return to work within weeks. Such examples underscore the importance of individualized care plans informed by precise diagnostics and expert surgical technique. These insights are supported by studies published in journals like The Journal of Orthopaedic Surgery and Research, highlighting improved outcomes with early intervention.
Integrating Orthopedic Nerve Treatment Into Your Healing Journey
Embarking on a treatment plan for nerve compression involves collaboration between patient and orthopedic provider. Patient education on activity modification and symptom monitoring is crucial. Additionally, combining therapies—such as using support braces (learn how to choose the right fit) with physical rehabilitation—can amplify healing potential. Staying informed about emerging treatments empowers patients to make decisions aligned with their lifestyle and goals.
If you or a loved one is facing nerve compression symptoms, engaging with an experienced orthopedic specialist can open pathways to effective relief and restored function. Reach out today to explore personalized treatment options tailored to your unique needs.
When Nerve Compression Feels Personal: My Journey with Orthopedic Care
Reflecting on my own experiences with nerve compression, I recall the frustration of those early symptoms—numbness creeping into my fingers and that persistent tingling that just wouldn’t quit. It’s easy to underestimate these signals, but they are the body’s way of crying for attention. What struck me personally was how pivotal finding the right orthopedic specialist was in shifting from mere symptom management to actual healing. This wasn’t just about taking painkillers; it was about understanding the root cause and embracing a treatment plan tailored specifically to me.
Why Early Diagnosis and Accurate Testing Matters More Than You Think
One of the most eye-opening moments in my care journey was undergoing an EMG and nerve conduction study (NCS). Witnessing how these tests unveiled the precise areas of nerve damage gave me confidence that my treatment was on the right track. It’s fascinating how technology and expert interpretation work hand in hand to create a roadmap for recovery. According to a comprehensive review in the Journal of Orthopaedic Surgery and Research, early and accurate diagnosis significantly improves patient outcomes by guiding targeted interventions.
Have You Ever Wondered How Lifestyle Changes Can Complement Orthopedic Treatments?
This question resonated with me as I realized that managing nerve compression isn’t solely about doctor’s visits or surgeries. Incorporating ergonomic adjustments in daily activities—like redesigning my workspace or modifying how I carry objects—played a surprisingly big role. Simple habits like taking frequent breaks, practicing gentle stretching, and even choosing the right support braces (here’s how to pick the best brace) made a tangible difference in my comfort and progress. It’s a powerful reminder that healing is holistic, blending medical expertise with mindful living.
Practical Tips From My Recovery Toolbox: What Truly Helped
From my personal experience, I can’t stress enough the value of a well-rounded rehabilitation plan. Physical therapy sessions focusing on strengthening and flexibility complemented my surgical and non-surgical treatments perfectly. Also, staying informed about treatment options, such as minimally invasive procedures, helped me make empowered decisions. I found that open communication with my orthopedic team was key to adjusting my plan as I healed, ensuring that progress was steady and setbacks were minimized.
If you’re navigating similar challenges, I’d love to hear about your experiences or answer any questions you might have. Feel free to share your story or ask away in the comments below—our shared journeys can offer strength and insight to each other. And if you’re just starting to explore your options, don’t hesitate to reach out to a trusted orthopedic specialist who can guide you through the process with expertise and care.
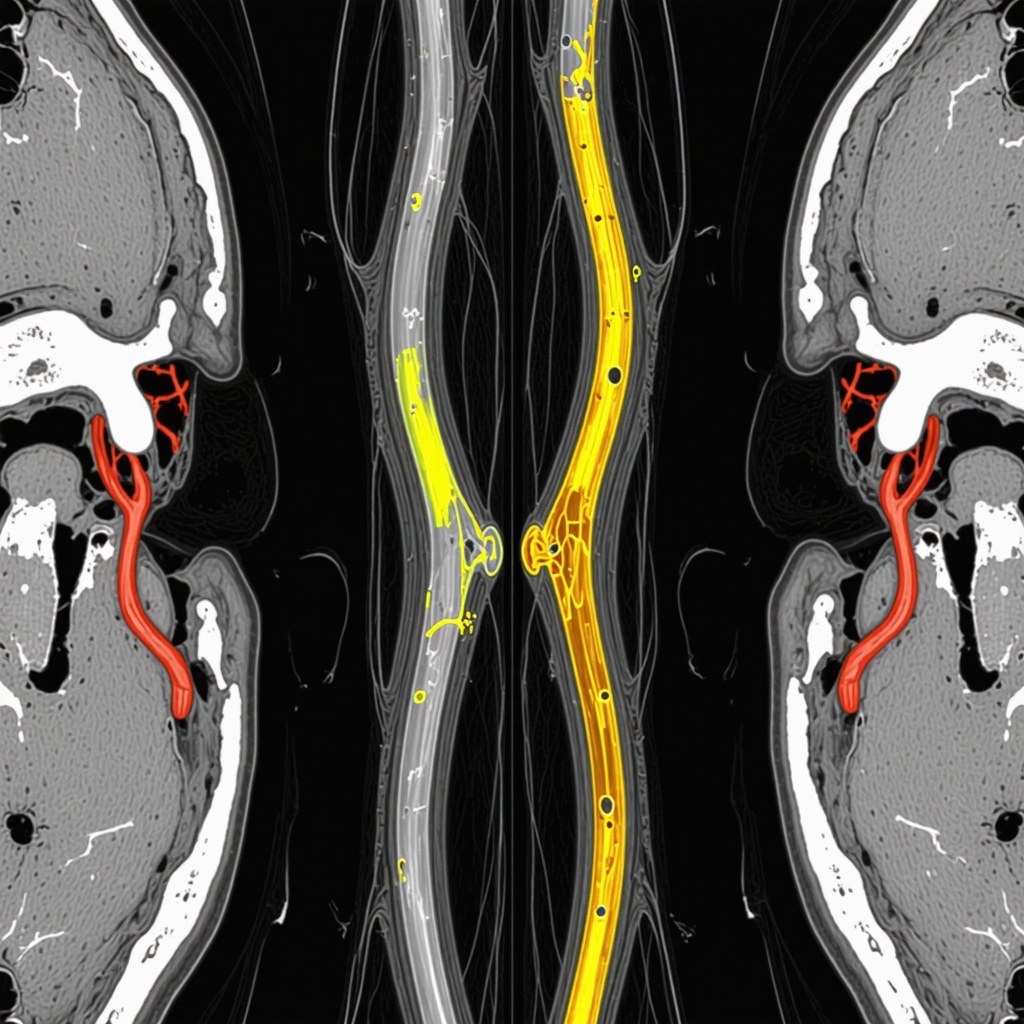
Decoding Complex Nerve Compression: The Role of Advanced Imaging and Electrophysiology in Precision Orthopedics
When nerve compression presents with atypical symptoms or involves multiple sites, traditional assessment methods may fall short. Here, advanced diagnostic modalities such as high-resolution ultrasonography, magnetic resonance neurography (MRN), and refined electrophysiological techniques become indispensable. MRN, in particular, offers unparalleled visualization of nerve morphology and surrounding tissue pathology, allowing orthopedic specialists to discern subtle entrapments or inflammatory changes that standard MRI might miss. Coupled with dynamic nerve conduction studies, these tools facilitate a nuanced understanding of the compressive etiology, guiding surgeons toward precisely targeted interventions that minimize collateral tissue trauma and optimize functional recovery.
Innovative Multimodal Therapeutic Approaches: Synergizing Orthopedic Surgery with Regenerative Medicine
Beyond decompression, emerging therapies integrate biologics such as platelet-rich plasma (PRP) and stem cell injections to enhance nerve healing post-intervention. These regenerative modalities, when combined with meticulous surgical technique and structured rehabilitation, accelerate axonal regeneration and reduce neuropathic pain. Orthopedic experts now evaluate the timing and candidacy for such adjunct treatments through rigorous patient profiling, ensuring personalized protocols that address both mechanical compression and the biochemical milieu inhibiting nerve recovery. Recent randomized controlled trials, including those published in The Journal of Orthopaedic Research, underscore the promising outcomes of combining surgical decompression with regenerative injections in refractory nerve compression syndromes.
What Are the Latest Criteria for Selecting Candidates for Minimally Invasive Versus Open Nerve Decompression?
Determining surgical approach has evolved from a one-size-fits-all to a highly individualized decision. Candidates for minimally invasive procedures typically exhibit localized entrapment with minimal perineural fibrosis and no prior surgical scarring. Conversely, open decompression remains the gold standard in cases with extensive fibrosis, recurrent compression, or anatomical anomalies. Preoperative imaging and electrophysiological assessment inform this stratification, while patient comorbidities and functional demands further refine surgical planning. Orthopedic surgeons also consider the potential for concurrent pathology, such as tendonitis or joint instability, which may necessitate combined surgical strategies.
Integrating Lifestyle and Ergonomic Engineering: A Preventative Orthopedic Paradigm
Orthopedic nerve specialists increasingly emphasize the intersection of biomechanics and lifestyle in both prevention and management. Customized ergonomic assessments, including workplace and home environment evaluations, identify modifiable risk factors such as repetitive strain, improper posture, and suboptimal tool use. Advanced wearable technologies now enable continuous monitoring of limb positioning and nerve stress, empowering patients to self-correct in real time. Incorporating these insights into comprehensive care plans not only mitigates symptom progression but also enhances long-term nerve health. This holistic approach represents a paradigm shift from reactive treatment to proactive nerve preservation.
If you’re interested in exploring how cutting-edge diagnostics and regenerative therapies can revolutionize your nerve compression treatment journey, connect with our orthopedic experts for a personalized consultation tailored to your unique clinical profile.
Harnessing Cutting-Edge Diagnostics: The Frontier of Precision Nerve Imaging
As nerve compression cases grow increasingly intricate, the integration of advanced imaging modalities has become indispensable. High-resolution ultrasonography enables dynamic, real-time visualization of nerve entrapment during movement, while magnetic resonance neurography (MRN) provides exquisite detail of nerve fascicles and perineural tissues. These technologies allow orthopedic specialists to detect subtle pathologies such as microvascular compromise or early inflammatory changes that traditional MRI might overlook. This diagnostic precision facilitates bespoke surgical planning, minimizing iatrogenic injuries and maximizing functional restoration.
How Can Electrophysiological Innovations Refine Orthopedic Treatment Plans for Nerve Compression?
Electrophysiological assessments, including refined nerve conduction velocity metrics and advanced electromyography techniques, have evolved to discern multifocal nerve lesions and differentiate demyelination from axonal degeneration. Such granular data empower orthopedic clinicians to stratify patients based on disease severity and prognosis, tailoring interventions accordingly. For instance, dynamic nerve conduction studies performed during provocative maneuvers can identify positional nerve impairments, informing decisions between conservative management and targeted decompression. These nuanced insights underscore the shift towards personalized orthopedic nerve care.
Synergistic Therapeutics: Merging Surgical Precision with Regenerative Medicine
Emerging evidence supports the application of biologic adjuvants such as platelet-rich plasma (PRP) and mesenchymal stem cell therapies alongside traditional decompression surgeries. These regenerative approaches potentiate axonal regeneration, modulate local inflammatory milieus, and expedite symptomatic relief. Orthopedic specialists meticulously select candidates based on comprehensive profiling, including electrophysiological severity, symptom chronicity, and comorbidities. The integration of these modalities represents a paradigm shift, endorsed by recent randomized controlled trials published in The Journal of Orthopaedic Research, demonstrating superior outcomes in refractory nerve compression syndromes.
Ergonomics Meets Technology: Proactive Strategies for Sustained Nerve Health
Prevention and long-term management now encompass biomechanical optimization through customized ergonomic interventions enhanced by wearable sensor technologies. These devices provide continuous feedback on limb positioning and nerve stress, enabling real-time correction of detrimental postures and repetitive strain patterns. Orthopedic clinicians leverage these data to design adaptive work environments and personalized activity modifications, transforming patient engagement from passive recipients to active participants in their healing journey. This innovative intersection of biomechanics and digital health fosters durable nerve preservation beyond episodic clinical encounters.
If you aspire to elevate your understanding of advanced nerve compression management or seek tailored orthopedic solutions integrating the latest diagnostic and regenerative advancements, connect with our expert orthopedic team today and embark on a transformative path toward optimal nerve health.
Frequently Asked Questions (FAQ)
What are the earliest signs of nerve compression that warrant orthopedic evaluation?
Early symptoms often include intermittent numbness, tingling, mild weakness, or a burning sensation along the nerve distribution. Prompt orthopedic assessment is crucial when these symptoms persist or progressively worsen, as early intervention can prevent irreversible nerve damage.
How do EMG and nerve conduction studies improve diagnosis compared to standard physical exams?
Electromyography (EMG) and nerve conduction studies (NCS) provide objective, quantifiable data on nerve function, enabling precise localization and severity assessment of compression. Unlike physical exams alone, these tests differentiate between demyelination and axonal injury and can detect multifocal or dynamic nerve impairments, guiding targeted treatment plans.
When is minimally invasive decompression preferred over open surgery for nerve entrapment?
Minimally invasive decompression is typically chosen for localized nerve entrapments without extensive scarring or anatomical complexity. It offers reduced tissue trauma, faster recovery, and less postoperative pain. However, open surgery remains necessary for recurrent cases, widespread fibrosis, or complicated anatomy identified via advanced imaging and electrophysiological studies.
Can regenerative medicine truly enhance nerve healing after decompression surgery?
Yes, adjunctive therapies like platelet-rich plasma (PRP) and mesenchymal stem cell injections have shown promise in accelerating axonal regeneration and modulating inflammation. When integrated with meticulous surgical technique and rehabilitation, these biologics can improve functional outcomes, especially in refractory or chronic nerve compression cases.
How do ergonomic modifications complement orthopedic treatment for nerve compression?
Ergonomic interventions reduce repetitive strain and abnormal nerve stress by optimizing posture, work environment, and activity patterns. Combined with medical treatments, they prevent symptom exacerbation, promote nerve recovery, and support long-term nerve health, making them indispensable in comprehensive management plans.
What role do advanced imaging modalities like magnetic resonance neurography (MRN) play in complex nerve compression?
MRN offers superior visualization of nerve fascicles and perineural tissues, detecting subtle entrapments, inflammation, or microvascular changes that conventional MRI may miss. This enhanced anatomical detail guides precise surgical planning, minimizing collateral damage and improving prognosis in complex or atypical cases.
Are lifestyle changes alone sufficient to manage mild nerve compression symptoms?
While lifestyle and ergonomic adjustments can alleviate mild symptoms and reduce progression risk, they are rarely sufficient as sole therapy for moderate to severe compression. Early orthopedic evaluation ensures appropriate interventions are initiated to prevent chronic nerve injury and functional loss.
How does continuous monitoring with wearable technology benefit nerve compression patients?
Wearable sensors provide real-time feedback on limb positioning and nerve stress, enabling patients to self-correct detrimental postures and reduce repetitive strain. This proactive approach enhances compliance with ergonomic recommendations and supports sustained nerve health beyond clinical visits.
What factors influence the decision to combine surgical decompression with regenerative therapies?
Patient-specific factors such as severity and chronicity of nerve damage, electrophysiological findings, comorbidities, and prior treatment responses guide combined therapy candidacy. Multidisciplinary evaluation ensures personalized protocols that optimize healing and minimize complications.
How important is patient education and communication in successful nerve compression treatment?
Effective patient education empowers individuals to understand their condition, adhere to treatment plans, and implement lifestyle modifications. Open communication with the orthopedic team allows timely adjustments, fosters trust, and ultimately enhances recovery trajectories and functional outcomes.
Trusted External Sources
- The Journal of Orthopaedic Surgery and Research: Provides peer-reviewed clinical studies and reviews on nerve compression diagnosis and treatment innovations, underpinning evidence-based orthopedic practices.
- The Journal of Orthopaedic Research: Features high-quality research on regenerative medicine applications in orthopedics, including clinical trials evaluating biologic therapies for nerve healing.
- National Institute of Neurological Disorders and Stroke (NINDS): Offers authoritative information on nerve disorders, diagnostic techniques, and management guidelines relevant to orthopedic nerve compression care.
- American Academy of Orthopaedic Surgeons (AAOS): Supplies comprehensive clinical resources, patient education materials, and consensus guidelines on musculoskeletal and nerve compression conditions.
- Radiological Society of North America (RSNA): Provides detailed insights into advanced imaging modalities like magnetic resonance neurography, essential for precision diagnosis and surgical planning.
Conclusion
Effective management of nerve compression hinges on early recognition, precise diagnosis, and individualized treatment strategies that leverage the latest orthopedic innovations. Advanced diagnostic tools such as EMG, nerve conduction studies, and magnetic resonance neurography enable targeted interventions, while minimally invasive surgeries and regenerative medicine approaches optimize nerve recovery. Integrating ergonomic modifications and wearable technologies fosters a proactive, holistic healing journey. Empowered by expert guidance and patient engagement, individuals can overcome nerve compression challenges and restore functional quality of life. To deepen your understanding or explore personalized orthopedic solutions, we invite you to share your experiences, ask questions, and connect with our specialized team dedicated to advancing nerve health and patient well-being.


I found this post’s emphasis on early and precise diagnosis especially insightful. From my experience with nerve compression symptoms, such as intermittent numbness and tingling, the moment I sought evaluation made a big difference in my recovery journey. What really resonated was how tools like EMG and nerve conduction studies go beyond standard physical exams by pinpointing the exact location and severity of nerve impairment. This kind of targeted approach seems essential in determining whether conservative treatments like physical therapy or support braces will suffice or if surgery is necessary.
Additionally, the mention of minimally invasive decompression surgery stood out. It’s encouraging how these procedures can relieve pressure while minimizing tissue damage and downtime. For anyone considering surgery, understanding the surgical criteria involving factors like perineural fibrosis and anatomical anomalies seems crucial.
One thing I’m curious about is how patients balance ergonomic lifestyle changes with medical treatments during recovery. Have others found that certain ergonomic adjustments noticeably improve symptoms or speed healing? It would be great to hear how readers integrate these preventative strategies alongside their clinical care plans.
I appreciate the detailed explanation about the comprehensive approach orthopedic specialists take in managing nerve compression. It’s fascinating how modern diagnostic tools like EMG and nerve conduction studies not only aid in pinpointing the exact location and severity but also facilitate more personalized treatment plans. From what I’ve seen in my own experience with mild wrist numbness, the combination of ergonomic adjustments and a structured physical therapy regimen made a substantial difference. Small changes like adjusting my workstation height and incorporating regular breaks for gentle wrist stretches seemed to alleviate symptoms and prevented progression.
Regarding Cameron’s question about balancing ergonomic lifestyle changes with medical treatments, I’ve found that integrating these adjustments early on complements clinical care remarkably well. It’s about creating a routine that supports nerve health beyond the clinical setting. Has anyone else noticed that certain ergonomic interventions, like using ergonomic keyboards or wrist braces during extended computer use, helped them maintain progress or reduce discomfort? Also, I wonder whether wearable devices that provide real-time feedback on posture and movement might soon become a standard part of rehabilitation plans to empower patients further in self-management. It would be great to hear others’ approaches or experiences with blending technology and lifestyle tweaks alongside professional treatments.
This post wonderfully emphasizes the importance of timely and precise intervention in nerve compression cases. From personal experience, I can attest that early diagnosis with advanced tools like EMG can truly make a difference. In my case, a gradual numbness in my hand was initially dismissed as fatigue, but further testing revealed a pinched nerve that could have led to lasting damage if left untreated. It’s inspiring to see how minimally invasive procedures and regenerative approaches, like PRP injections, are changing patient outcomes. I’m curious—how widely available are these cutting-edge diagnostics like MRN in community hospitals? Additionally, have others integrated regenerative therapies into their recovery plans, and what has been your experience with their effectiveness? It seems holistic management combining medical innovation with lifestyle adjustments holds great promise for long-term nerve health.
Reading this comprehensive post really highlights how advanced diagnostics and personalized treatment plans are transforming nerve compression care. I particularly appreciate the mention of tools like MRN and electrophysiological studies, which bring a new level of precision to diagnosis. In my own experience, early detection through such advanced imaging definitely made a difference in my recovery process — I was able to start targeted therapies sooner, preventing worsening symptoms. I’m curious, though—what are some of the latest developments in regenerative medicine that could further improve nerve healing outcomes? I’ve read about promising results with stem cell therapies and biologics like PRP, but I wonder how soon these might become standard adjuncts to surgical decompression. Has anyone here had experience with these regenerative approaches, and if so, what was your journey like? I believe integrating these innovative treatments with traditional surgical methods could really push the boundaries of recovery for nerve compression patients.