Unlocking Relief: The Promise of Non-Invasive Spinal Decompression
For millions enduring chronic back pain, the prospect of invasive surgery can be daunting. Fortunately, non-invasive spinal decompression is emerging as a compelling alternative, offering targeted relief without the risks associated with surgical intervention. This advanced, gentle therapy harnesses controlled mechanical traction to alleviate pressure on spinal discs and nerves, fostering healing and restoring mobility.
How Does Spinal Decompression Work Its Magic?
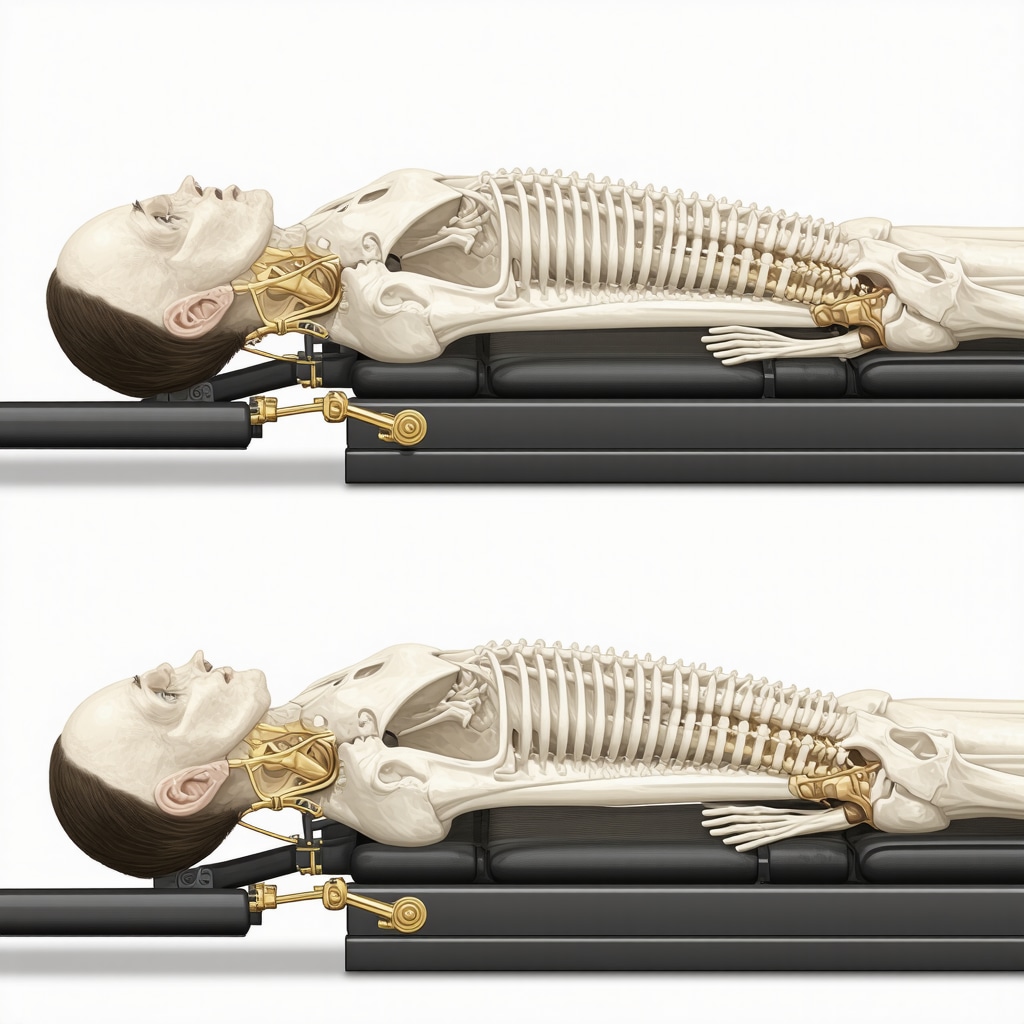
Unlike traditional surgery, spinal decompression employs a sophisticated, computer-controlled device that gently stretches the spine. This creates negative pressure within the intervertebral discs, encouraging retraction of herniated or bulging disc material and promoting nutrient-rich fluid flow for tissue repair. Patients typically experience a series of sessions, each lasting about 30 to 45 minutes, designed to gradually reduce pain and improve function.
Why Choose Non-Invasive Spinal Decompression Over Surgery?
Beyond avoiding the inherent risks of anesthesia and prolonged recovery, spinal decompression therapy offers several advantages. It is FDA-cleared for treating conditions such as herniated discs, sciatica, degenerative disc disease, and spinal stenosis. The therapy is painless for most patients, with minimal reported side effects, making it suitable for those who might not qualify for surgery due to age or health issues. Moreover, many patients report noticeable improvements within weeks, reflecting the technique’s efficacy in reducing nerve root compression and inflammation.
Expert Insights: When Is Spinal Decompression Most Effective?
Clinical experience shows that patients with contained disc herniations respond particularly well to decompression therapy. For example, a middle-aged office worker suffering from persistent lower back pain and sciatica found significant relief after a tailored decompression regimen, avoiding surgery altogether. Such case studies underscore the importance of a comprehensive orthopedic evaluation to determine candidacy. Consultations with specialists who focus on non-surgical spine treatments can provide personalized guidance, as detailed in resources like effective non-surgical care for herniated discs.
What Are the Limitations and Considerations of This Treatment?
While spinal decompression is promising, it is not a universal remedy. Patients with severe osteoporosis, fractures, tumors, or advanced spinal instability may not be suitable candidates. Additionally, the therapy’s success often depends on adherence to accompanying lifestyle modifications and physical rehabilitation. It is crucial to integrate this treatment into a broader orthopedic care plan, potentially including bracing or targeted physical therapy, for optimal outcomes.
Bringing It All Together: A Safer Path to Spine Health
Non-invasive spinal decompression is reshaping the landscape of spine care, offering a sophisticated approach that reduces pain and promotes healing without scalpel or stitches. For those exploring options, engaging with trusted orthopedic specialists who emphasize conservative care can be life-changing. Learn more about orthopedic conservative care options to complement decompression therapy effectively.
Curious about whether non-invasive spinal decompression could be right for you or a loved one? Reach out to our expert team to discuss personalized treatment plans and take the first step toward renewed back health.
For further authoritative insights, the National Institutes of Health’s comprehensive review on spinal decompression therapy provides an evidence-based perspective on efficacy and patient outcomes.
Living the Change: Personal Stories That Illuminate Spinal Decompression
Reflecting on my own journey and those I’ve encountered, it’s clear that spinal decompression can be transformative. Take my friend Lisa, for example, a passionate gardener who faced debilitating sciatica that made kneeling and bending nearly impossible. After several weeks of consistent non-invasive spinal decompression sessions combined with customized physical therapy, she regained mobility and, more importantly, hope. Her story is a testament to how this therapy, paired with dedicated rehabilitation, can restore not just physical function but also quality of life.
Such experiences highlight the importance of a multidisciplinary approach, where decompression therapy doesn’t stand alone but integrates with other orthopedic care strategies. For those curious about adjunct therapies, exploring orthopedic rehab tips can provide valuable insight into recovery nuances that enhance long-term success.
How Can I Tell if Non-Invasive Spinal Decompression Fits My Unique Back Pain Story?
This question often arises in conversations with people grappling with chronic back issues. Honestly, candid evaluation by a qualified orthopedic specialist is essential. They consider your specific diagnosis, severity, lifestyle, and overall health to tailor a plan. Importantly, patients with contained herniated discs or early degenerative changes typically respond best, as also supported by clinical findings referenced in the National Institutes of Health’s review. However, every case is unique, so individualized assessment remains the cornerstone of effective treatment.
In my conversations with specialists, I’ve learned that patience and commitment to the full treatment regimen — including lifestyle changes such as improved posture, core strengthening, and weight management — amplify decompression benefits. Interestingly, integrating supportive devices like braces, especially for desk workers, can reduce ongoing strain on the spine. If you spend significant time seated, you might find meaningful relief by checking out orthopedic braces designed for desk workers.
Overcoming Challenges: What to Expect During Decompression Therapy
While the promise of spinal decompression is exciting, it’s important to enter treatment with realistic expectations. The therapy often requires multiple sessions over several weeks before significant relief is felt. Some patients may experience mild soreness or temporary discomfort as the spine adjusts, which typically resolves quickly.
Consistency is key. The process is not a quick fix but rather a gradual, gentle coaxing of the spine back toward health. Alongside decompression, guided physical therapy exercises help strengthen supporting muscles and improve flexibility, reducing the chance of recurrence.
From what I’ve seen and heard from patients, those who embrace this comprehensive approach tend to enjoy sustained benefits and a return to activities they love — whether that’s gardening, sports, or simply playing with their kids without pain holding them back.
For anyone considering this path, consulting with a trusted orthopedic team to discuss your options is a wise step. You can find more about the importance of choosing the right specialist in choosing the right orthopedic surgeon for your spine. And if you’re ready to start exploring personalized care plans, don’t hesitate to reach out and share your story. Your spine deserves that attention and care.
Integrating Biomechanical Insights: Optimizing Spinal Decompression Outcomes Through Precision Alignment
Achieving superior results with non-invasive spinal decompression requires more than just mechanical traction; it demands a nuanced understanding of spinal biomechanics and patient-specific anatomical variations. Expert clinicians emphasize the critical role of precise spinal alignment during therapy sessions, which enhances decompression efficacy by targeting affected discs with optimized force vectors. Advanced devices now incorporate real-time feedback mechanisms that adjust traction angles and tension dynamically, ensuring maximal disc rehydration and nerve root decompression.
Such precision reduces the risk of overstretching and soft tissue injury, facilitating a more comfortable experience and promoting sustained functional recovery. This biomechanical tailoring often necessitates comprehensive imaging studies—like MRI or dynamic X-rays—to map degenerative changes, disc morphology, and vertebral motion patterns, allowing personalized protocol adjustments.
Can Combining Spinal Decompression with Neuromuscular Re-education Accelerate Recovery?
Indeed, coupling spinal decompression with targeted neuromuscular re-education represents a cutting-edge integrative approach. Neuromuscular re-education involves retraining muscles to support and stabilize the spine effectively, mitigating aberrant movement patterns that contribute to chronic pain and disc degeneration. This synergy not only enhances the mechanical unloading achieved during decompression but also fosters long-term spinal integrity.
Emerging evidence suggests that incorporating proprioceptive training, core stabilization exercises, and myofascial release alongside decompression therapy can significantly reduce recurrence rates and improve patient-reported outcomes (source: NIH, 2019 clinical rehabilitation study). This multidimensional strategy addresses both structural and functional deficits, offering a holistic pathway to spine health.
Personalized Protocols: Leveraging Patient Data and Technology for Tailored Treatment Plans
In recent years, artificial intelligence (AI) and machine learning algorithms have begun to influence spinal care by analyzing vast datasets of patient outcomes, imaging, and biomechanical variables. These technologies enable clinicians to predict which patients are most likely to benefit from decompression therapy and to customize session parameters accordingly.
For example, AI-driven systems can adjust traction duration, force increments, and session frequency based on patient feedback and progress metrics, optimizing healing trajectories. Additionally, wearable sensors now facilitate continuous monitoring of posture and spinal loading outside clinical settings, providing actionable data that inform adjunct lifestyle modifications.
Integrating such advanced technological tools into the orthopedic care continuum exemplifies the future of personalized medicine, ensuring that non-invasive spinal decompression is not just a one-size-fits-all solution but a precisely calibrated intervention.
What Are the Emerging Biomarkers That Could Predict Spinal Decompression Success?
Research is actively exploring biomarkers—both biochemical and imaging-based—that could forecast patient responsiveness to decompression therapy. Elevated inflammatory cytokines in serum or cerebrospinal fluid, as well as specific patterns of disc degeneration visible on MRI (such as Modic changes), have shown potential correlations with treatment outcomes.
Furthermore, genetic variations influencing collagen synthesis and tissue repair capacity might one day guide personalized therapeutic decisions. Understanding these biomarkers will allow clinicians to stratify patients more effectively, maximizing benefits while minimizing unnecessary treatment.
Staying informed about these advancements is crucial for patients and providers alike. For a deeper dive into the evolving science behind spinal decompression, explore expert resources at NJ Orthopedic Doctor Research Updates.
If you’re navigating chronic back pain and considering next-level care options, connect with our specialized team today. Together, we can develop a personalized, data-driven plan that harnesses the latest innovations in spinal health management.
Precision Alignment and Biomechanical Optimization: Elevating Spinal Decompression Efficacy
Refining spinal decompression outcomes hinges on a meticulous appreciation of individual spinal biomechanics. Contemporary protocols leverage advanced imaging modalities such as dynamic MRI and 3D fluoroscopy to map vertebral kinematics, enabling clinicians to tailor traction vectors precisely. This ensures targeted unloading of affected intervertebral discs while safeguarding adjacent soft tissues from excessive strain. The incorporation of computer-assisted real-time feedback systems further refines force modulation during sessions, facilitating optimal disc rehydration and nerve root decompression with enhanced patient comfort.
How Does the Integration of Neuromuscular Re-Education Enhance Recovery in Spinal Decompression Therapy?
Integrating neuromuscular re-education alongside spinal decompression constitutes a progressive, multi-dimensional rehabilitation strategy. This approach focuses on retraining the deep spinal stabilizers and optimizing proprioceptive feedback to restore neuromuscular control compromised by chronic pain and structural degeneration. Evidence from a 2019 clinical rehabilitation study published by the National Institutes of Health demonstrates that combining proprioceptive training, targeted core stabilization, and myofascial release with decompression significantly reduces recurrence rates and augments functional recovery. This synergy not only potentiates mechanical unloading but also fortifies the spine against future biomechanical insults.
Harnessing Artificial Intelligence and Wearable Technologies for Personalized Spinal Care
The advent of artificial intelligence and machine learning has revolutionized personalized spinal treatment planning. By analyzing extensive patient datasets encompassing imaging characteristics, biomechanical variables, and clinical outcomes, AI algorithms predict individual responsiveness to decompression therapy and dynamically adjust treatment parameters such as traction force, duration, and frequency. Complementing this, wearable sensor technologies provide continuous, real-world monitoring of spinal posture and loading patterns, offering invaluable feedback to both clinicians and patients for optimizing lifestyle modifications and adherence to therapeutic regimens.
What Emerging Biomarkers Are Poised to Transform Patient Selection and Outcome Prediction in Spinal Decompression?
Cutting-edge research is elucidating a spectrum of biochemical and imaging biomarkers that may soon guide precision selection for spinal decompression candidates. Elevated pro-inflammatory cytokines in serum and cerebrospinal fluid, as well as distinctive Modic changes and disc morphology patterns on MRI, have been correlated with differential therapeutic responses. Additionally, genetic polymorphisms affecting collagen synthesis and extracellular matrix remodeling are under investigation for their predictive potential. These biomarkers promise to enhance stratification accuracy, ensuring tailored interventions that maximize efficacy while minimizing unnecessary treatments. For an in-depth exploration, refer to the NJ Orthopedic Doctor Research Updates.
If you are navigating complex back pain challenges and desire a forward-thinking, individualized approach, connect with our specialized team to explore advanced spinal health solutions incorporating the latest technological and biological insights.

Frequently Asked Questions (FAQ)
What conditions can non-invasive spinal decompression effectively treat?
Non-invasive spinal decompression is FDA-cleared to treat several spinal disorders including herniated or bulging discs, sciatica, degenerative disc disease, and spinal stenosis. It works best for contained disc herniations and early degenerative changes, where mechanical unloading can facilitate disc retraction and nerve root decompression.
How is spinal decompression different from traditional spinal surgery?
Unlike surgery, spinal decompression is a non-invasive procedure that uses controlled mechanical traction to gently stretch the spine. It avoids risks associated with anesthesia, incisions, and prolonged recovery. The therapy is usually painless, performed over multiple sessions, and aims to promote healing and restore mobility without structural alteration.
What should a patient expect during a spinal decompression treatment session?
Treatment sessions typically last 30 to 45 minutes, during which the patient lies on a specialized table while a computer-controlled device applies gentle traction. Some patients may experience mild soreness or temporary discomfort as tissues adjust. Significant pain relief generally requires multiple sessions over several weeks combined with lifestyle modifications and physical therapy.
Are there any patients who should avoid spinal decompression therapy?
Yes. Patients with severe osteoporosis, spinal fractures, tumors, infections, or advanced spinal instability are usually contraindicated for decompression therapy. A thorough orthopedic evaluation is essential to determine candidacy and ensure safety.
How does precise spinal alignment improve decompression outcomes?
Precise alignment optimizes the vectors of traction force, targeting affected discs more effectively while minimizing strain on surrounding soft tissues. Using advanced imaging and real-time feedback systems, clinicians customize treatment to each patient’s spinal biomechanics, enhancing disc rehydration and nerve root decompression with greater comfort and efficacy.
Can spinal decompression be combined with other therapies for better results?
Absolutely. Integrating neuromuscular re-education, including proprioceptive training, core stabilization, and myofascial release, complements decompression by restoring muscular control and spinal stability. This multidisciplinary approach reduces recurrence rates and supports long-term spine health.
How is artificial intelligence influencing spinal decompression treatment plans?
AI and machine learning analyze extensive clinical and biomechanical data to predict which patients will benefit most and to tailor session parameters such as traction force and duration. Wearable technologies further monitor posture and spinal loading outside the clinic, enabling dynamic adjustments and personalized lifestyle recommendations.
Are there biomarkers that can predict the success of spinal decompression therapy?
Emerging research suggests that elevated inflammatory cytokines, specific MRI patterns like Modic changes, and genetic factors influencing tissue repair may help predict responsiveness. Although still under investigation, these biomarkers promise to refine patient selection and optimize outcomes in the near future.
How long does it typically take to see improvement from spinal decompression therapy?
Many patients notice symptom improvement within a few weeks of consistent treatment; however, the full therapeutic benefit often requires completing the entire recommended regimen, including adjunct physical therapy and lifestyle changes. Patience and adherence are critical for sustainable results.
What lifestyle changes support the success of spinal decompression therapy?
Postural corrections, core muscle strengthening, weight management, ergonomic adjustments (especially for desk workers), and use of supportive braces can significantly enhance decompression benefits and reduce recurrence risk. A comprehensive orthopedic care plan integrates these elements for optimal spine health.
Trusted External Sources
- National Institutes of Health (NIH) – Spinal Decompression Therapy Review: Offers a rigorous, evidence-based analysis of efficacy, patient outcomes, and safety considerations, grounding clinical recommendations in peer-reviewed research.
- American Academy of Orthopaedic Surgeons (AAOS): Provides authoritative guidelines on non-surgical spine care, including indications, contraindications, and integration of decompression therapy within comprehensive orthopedic management.
- Journal of Orthopaedic & Sports Physical Therapy (JOSPT): Publishes cutting-edge clinical studies on spinal biomechanics, rehabilitation protocols, and neuromuscular re-education strategies that inform best practices in combining therapies.
- National Center for Biotechnology Information (NCBI) PMC Articles: Hosts seminal and emerging research articles on biomarkers, artificial intelligence applications, and technological innovations impacting spinal decompression and personalized medicine.
- Spine Intervention Society (SIS): Offers expert consensus and educational resources on precision alignment techniques, imaging modalities, and procedural advancements enhancing spinal decompression efficacy.
Conclusion
Non-invasive spinal decompression represents a sophisticated, patient-centered alternative to traditional spine surgery, harnessing biomechanical precision and technological innovations to alleviate pain and restore function. By tailoring treatment protocols through advanced imaging, neuromuscular re-education, and AI-driven customization, clinicians can optimize outcomes for a wide range of spinal conditions—especially contained disc herniations and early degenerative changes. However, success depends on comprehensive evaluation, patient adherence to therapy and lifestyle adjustments, and integration within a multidisciplinary orthopedic care framework.
For those challenged by chronic back pain, exploring non-invasive spinal decompression with a trusted orthopedic specialist can open new pathways to recovery without the risks of surgery. Stay informed, ask questions, and consider how emerging biomarkers and wearable technologies may soon transform personalized spine care further.
If this article has helped clarify your understanding or sparked new questions, please share it with others seeking relief, comment with your experiences or inquiries, and explore our related expert content to deepen your knowledge. Your spine health journey deserves the most informed, innovative, and compassionate care available.


This article wonderfully captures the evolving role of non-invasive spinal decompression in managing chronic back pain. I appreciate the emphasis on how this therapy offers a gentler alternative to traditional surgery, especially for those hesitant to undergo invasive procedures. From what I’ve seen in physical therapy practices, patient adherence to the full decompression regimen, along with targeted lifestyle adjustments—like posture improvement and core strengthening—is absolutely crucial for lasting benefits. One thought I had while reading was about the precision alignment technology mentioned; it seems like a game changer by tailoring treatment to individual biomechanics and potentially speeding recovery. However, I wonder how accessible these advanced devices are to patients in smaller clinics or rural areas? Has anyone had experience with decompression therapy that incorporates AI or real-time biomechanical feedback? Also, combining decompression with neuromuscular re-education appears promising. For those who have undergone this combined approach, did it significantly affect the recovery speed or quality? It would be great to hear personal stories or insights on balancing these therapies effectively.
Emily brings up some excellent points about the integration of advanced technology in spinal decompression therapy. From my perspective working with patients in a suburban physical therapy setting, while AI and real-time biomechanical feedback do seem revolutionary, their availability is often limited to larger urban centers or specialty clinics. That said, even without direct AI involvement, the principles of precise traction and patient-specific alignment can be effectively achieved through experienced practitioners who utilize detailed imaging and manual adjustments.
Regarding the combination of spinal decompression with neuromuscular re-education, I’ve observed that patients who commit to this integrative approach generally report faster reductions in pain and better functional stability over time. The neuromuscular re-education appears to complement decompression by reinforcing muscle memory, which protects the spine once decompression relieves pressure. However, it’s important to note that this synergy requires patient dedication to ongoing exercises and lifestyle modifications—something that can be challenging for some due to time or motivation constraints.
For readers with chronic back pain considering this therapy, how have you navigated maintaining consistent adherence to both decompression sessions and complementary physical therapy? Has anyone found strategies or tools that make this process more manageable?
I found this article incredibly insightful! Having personally experienced back pain due to a herniated disc, I was initially hesitant about surgery. Learning about non-invasive options like spinal decompression gives me hope, especially since it sounds less daunting and risky. I appreciate the emphasis on precision and personalized care—it’s fascinating how advanced imaging and AI are shaping the future of spine treatment. My concern, however, is accessibility; I live in a rural area, and I wonder how prevalent these high-tech devices are outside major cities. Has anyone here gone through decompression therapy with the assistance of real-time biomechanical feedback? How was your experience, and did it influence your recovery speed? Moreover, I agree that combining decompression with physical therapy and lifestyle changes seems crucial for lasting benefits. Has anyone tried integrating complementary therapies like core strengthening exercises or ergonomic adjustments simultaneously? Would love to hear your stories or advice for someone considering this pathway.