Imagine this: I was mid-sentence, reaching for my coffee mug when a sharp, shooting pain suddenly gripped my neck. My first instinct was to shrug it off—just a stiff muscle, I thought. But as hours turned into days, the pain intensified, radiating down my arm and making even simple movements a challenge. It was a lightbulb moment for me: I needed professional help. That experience taught me how crucial it is to recognize when a pinched nerve requires expert treatment, especially from a qualified Orthopedic Doctor.
Why Your Pinched Nerve Demands Immediate Attention
Pinched nerves are more common than you might think. According to a study published in the Journal of Orthopedic Surgery, approximately 85% of adults will experience back or neck pain caused by nerve compression at some point. If left untreated, a pinched nerve can lead to chronic pain, numbness, or even permanent nerve damage. It’s not just about discomfort; it’s about protecting your mobility and quality of life. That’s why seeking guidance from a specialist can make all the difference.
Question: Is Seeing an Orthopedic Doctor Actually Worth the Hype?
Early on, I made the mistake of trying to self-diagnose and delay professional care. I thought rest and over-the-counter medications would suffice. But the pain persisted and worsened. An experienced orthopedic surgeon can accurately diagnose the root cause of nerve compression and recommend effective treatments—whether surgical or non-surgical. Trust me, consulting a specialist early can save you from prolonged suffering and costly complications.
If you’ve ever wondered whether your symptoms warrant professional intervention, keep reading. I’ll walk you through how to identify the signs and what steps to take to find the right expert for your needs. Navigating this journey might seem daunting, but understanding your options is the first step toward relief and recovery. Ready to learn the secrets to overcoming a pinched nerve? Let’s dive into the practical solutions that can help you regain control over your health.
} }#assistant {
Consult a Qualified Orthopedic Doctor for Accurate Diagnosis
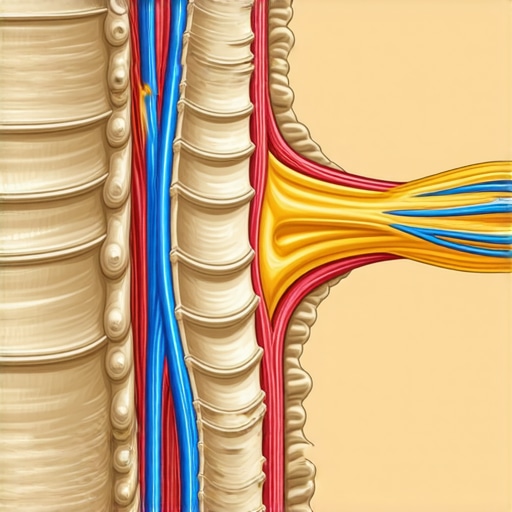
The first crucial step is to schedule an appointment with an experienced orthopedic surgeon. During this visit, the doctor will perform a comprehensive physical exam, review your medical history, and may order imaging tests like MRI or X-ray to pinpoint the exact cause of nerve compression. I remember visiting my orthopedic specialist after weeks of persistent pain. The detailed scans they ordered revealed a herniated disc pressing on my nerve, which I never suspected. This precise diagnosis allowed for targeted treatment planning.
Explore Non-Surgical Treatment Options First
Physical Therapy and Rehabilitation
Engage in specialized physical therapy aimed at reducing inflammation, strengthening supporting muscles, and improving flexibility. A tailored rehab program can significantly alleviate symptoms and prevent recurrence. For example, I followed a dedicated rehab protocol prescribed by my therapist, which helped me regain mobility without surgery. Consistency in exercises and adherence to professional guidance are key.
Medications and Injections
Over-the-counter anti-inflammatory drugs or prescribed medications can reduce swelling and pain. In some cases, epidural steroid injections provide targeted relief by decreasing nerve inflammation. I found that these injections offered quick symptom relief, allowing me to participate more actively in physical therapy.
Consider Minimally Invasive Procedures
If conservative treatments don’t provide sufficient relief, your doctor might recommend minimally invasive procedures like spinal decompression or microdiscectomy. These techniques involve smaller incisions, less pain, and quicker recovery times. I was apprehensive but opted for a minimally-invasive back treatment, which resulted in significant pain reduction and restored function within weeks.
Evaluate Surgical Options as a Last Resort
In cases where nerve compression is severe or persists despite other treatments, surgical intervention may be necessary. Procedures such as spinal fusion or discectomy can decompress the nerve and stabilize the spine. My doctor explained the risks and benefits thoroughly, emphasizing that surgery is a last resort after exhausting all non-invasive options. Learning about these procedures helped me make an informed decision when my symptoms worsened.
Post-Treatment Care and Lifestyle Adjustments
Recovery doesn’t end with the procedure. Follow your doctor’s instructions for rehabilitation, and incorporate lifestyle changes such as ergonomic adjustments, regular exercise, and weight management to prevent future nerve issues. I incorporated daily stretching routines and ergonomic work setups, which contributed to long-term relief and prevented recurrence.
< >
>
Common Myths That Cloud Your Understanding of Pinched Nerves
One of the most pervasive misconceptions is that all pinched nerves are the same and require immediate surgery. In reality, most cases can be effectively managed with conservative treatments, such as physical therapy or epidural injections. Another myth is that pain always correlates with nerve damage severity. However, research in the Journal of Orthopedic Surgery shows that nerve compression symptoms can vary widely regardless of the extent of physical damage, leading some patients to underestimate their condition.
The Nuance of Early Diagnosis and Its Impact on Outcomes
Many believe that waiting it out will lead to spontaneous healing. But, as I learned firsthand, early intervention by a qualified orthopedic specialist can significantly alter the prognosis. Delays can result in chronic pain or permanent nerve impairment. The key is recognizing subtle early signs—such as intermittent numbness or tingling—and seeking expert assessment promptly.
Advanced Mistakes: Overreliance on Imaging and Ignoring Functional Symptoms
A common mistake is to rely solely on MRI or X-ray results without correlating findings with actual functional impairments. Imaging can sometimes show nerve compression that isn’t clinically significant, leading to unnecessary invasive procedures. Conversely, some patients dismiss persistent symptoms because imaging looks normal. An expert clinician evaluates both imaging and functional tests, including nerve conduction studies, for a comprehensive diagnosis.
Question: How Can Understanding the Nuances Influence Your Treatment Plan?
Knowing that nerve pain can stem from various causes—such as disc herniation, bone spurs, or ligament thickening—allows for personalized treatment strategies. For example, a rehab plan tailored to the specific cause can improve outcomes. Additionally, understanding that some nerve issues respond better to non-surgical interventions prevents unnecessary surgeries and promotes recovery through targeted therapies.
In my experience, recognizing these nuances helped me avoid rushed surgical decisions and instead pursue effective conservative care, which ultimately restored my mobility. If you’re dealing with nerve symptoms, consider consulting a specialist who understands these complexities. Have you ever fallen into this trap? Let me know in the comments.
Maintaining your spine health and ensuring long-term relief from a pinched nerve requires the right set of tools and consistent strategies. Over the years, I’ve found that integrating specific equipment and software can make a significant difference in recovery and ongoing management.
Invest in Quality Support Equipment
One of my top recommendations is a high-quality ergonomic chair with adjustable lumbar support. It helps maintain proper posture during daily activities, reducing strain on your spine. Personally, I use an ergonomic office chair with memory foam lumbar support, which has been crucial in preventing aggravation of my nerve issues. Additionally, consider a supportive cervical pillow for sleep, as proper alignment during rest can prevent unnecessary pressure on your cervical nerves.
Utilize Effective Physical Therapy Tools
Incorporating tools like foam rollers and massage sticks into your daily routine can aid in muscle relaxation and improve flexibility. I regularly use a foam roller on my back and hips to release tension, which complements my physical therapy sessions. For targeted nerve relief, TENS (Transcutaneous Electrical Nerve Stimulation) units have been a game-changer. These devices deliver gentle electrical impulses to nerve pathways, reducing pain and inflammation effectively.
Leverage Technology for Consistent Care
Apps like PhysiApp or MyRehab facilitate personalized exercise programs and track your progress over time. I rely on these to stay disciplined with my rehab exercises, ensuring consistency even on busy days. Additionally, wearable devices that monitor posture and activity levels can alert you when you’re slouching or overexerting, allowing you to adjust proactively.
Long-Term Results and Scaling Your Care
As your condition improves, scaling your approach involves gradually increasing exercise intensity and incorporating strength training to support your spine. I recommend consulting with your orthopedic specialist about a long-term plan that includes periodic assessments and updates to your rehab routine. Over time, integrating yoga or pilates can enhance flexibility and core stability, further supporting nerve health.
Question: How do I maintain progress and prevent recurrence?
The key is consistency. Regularly using supportive equipment, following your personalized rehab plan, and staying active with low-impact exercises are vital. Furthermore, keep up with scheduled check-ins with your healthcare provider to monitor your progress and adapt your tools as needed. Remember, proactive maintenance today ensures a pain-free tomorrow.
In my journey, adopting these tools and strategies has been pivotal. I encourage you to explore and personalize these methods for your recovery. Want to learn more about advanced therapies? Check out minimally-invasive back treatments for long-term relief.
The Hardest Lesson I Learned About Pinched Nerves
One of the most profound realizations I had was that pain is often a messenger, not just an inconvenience. I used to dismiss early symptoms, thinking they would pass, but ignoring them only prolonged my suffering. That taught me the importance of listening to my body and seeking expert advice before things worsen.
3 Myths About Pinched Nerves That Held Me Back
Myth one: All pinched nerves require surgery. In reality, most cases respond well to conservative treatments. Myth two: Rest alone cures nerve compression. Active physical therapy is often necessary. Myth three: Imaging results tell the whole story. Clinical evaluation is equally vital. Debunking these myths helped me find the right treatment faster.
What Experts Won’t Tell You About Treating Pinched Nerves
Many professionals focus on immediate relief but overlook the importance of long-term prevention. Regular lifestyle adjustments, ergonomic improvements, and ongoing exercises are crucial. I learned that maintaining spinal health is an ongoing journey, not just a one-time fix. This insight empowered me to take control of my recovery and future well-being.
Curated Resources to Guide Your Recovery
My Essential Toolkit for Pinched Nerves includes:
- Effective Nonsurgical Care: The resource Effective Non-Surgical Care helped me understand alternative treatments that work.
- Expert Tips on Rehab: The guide Orthopedic Rehab Tips provided practical exercises that accelerated my healing.
- Innovative Treatment Options: Learning about Minimally Invasive Back Treatments opened new avenues for my recovery journey.
Your Turn to Try
Dealing with a pinched nerve can be daunting, but with the right knowledge and professional guidance, you can regain control and restore your quality of life. Remember, early intervention and personalized care are your best allies in this journey. Take that first step today, and don’t hesitate to seek expert help—your future self will thank you for it.
What has been your biggest challenge in managing nerve pain? Share your story below, and let’s support each other in overcoming these hurdles together.


Reading this post really resonated with my own experience. I ignored my neck pain at first, thinking it was just muscle strain from sitting at my desk too long. But over time, I noticed the numbness creeping down my arm, which finally prompted me to see a specialist. The detailed diagnosis and personalized treatment plan made all the difference—I learned that early intervention can prevent long-term damage. Have others found that specific ergonomic adjustments, like using an adjustable chair or cervical pillow, helped with recovery? I’ve found that small changes in my daily setup made a big impact on managing my nerve issues and preventing exacerbation. It’s clear that understanding the root cause, from disc herniation to bone spurs, is key to choosing the right treatment approach. What do you all think about the importance of lifestyle adjustments alongside medical treatments for nerve health? Would love to hear your insights and personal success stories.