When Your Back Is Against the Wall: Why an Orthopedic Evaluation Is a Game-Changer
Ever find yourself stuck in a painful limbo after a work injury, wondering what the next step should be? You’re not alone. Navigating the maze of medical assessments can feel overwhelming, but there’s a beacon of hope: the orthopedic evaluation. Think of it as your personal injury detective, uncovering the root cause of pain and charting a course toward recovery.
The Inside Scoop: What Does an Orthopedic Evaluation Entail?
Is it like a medical interrogation? Well, sort of—minus the suspicion!
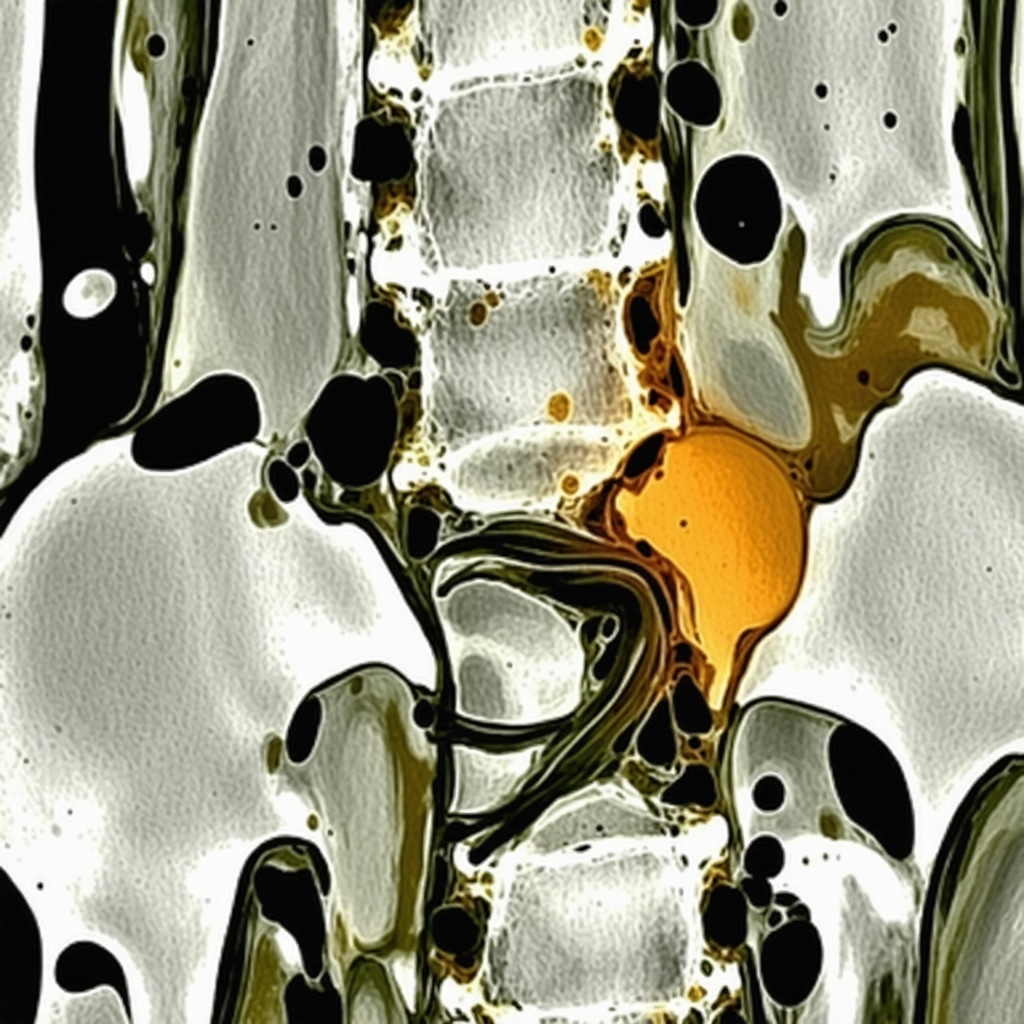
During this comprehensive assessment, an experienced orthopedic specialist will review your medical history, conduct physical examinations, and possibly order diagnostic tests like X-rays or MRI scans. This isn’t just about pinpointing the pain; it’s about understanding how your injury affects your body’s architecture and function. For instance, if you’ve suffered a herniated disc, the evaluation helps determine whether surgery, physical therapy, or non-invasive treatments are the best course.
Why Should You Care About This Evaluation?
Because knowledge is power—and in the world of work injuries, it’s also the key to effective treatment. An accurate diagnosis ensures you’re not caught in a cycle of guesswork or unnecessary procedures. Moreover, a detailed report from your orthopedic evaluation becomes your legal and insurance ally, providing documented evidence crucial for workers’ compensation claims.
How an Evaluation Accelerates Your Road to Recovery
Imagine trying to fix a leaky faucet without identifying the source. Frustrating, right? The same applies to injury treatment. A thorough orthopedic evaluation pinpoints the problem, enabling tailored treatment plans that can include everything from physical therapy to minimally invasive surgeries. Plus, early and precise intervention often shortens recovery timelines, getting you back on your feet faster.
What’s Next After the Evaluation?
Once the exam is complete, your doctor will discuss the findings and recommend treatment options. This might mean a referral to specialized physical therapy, pain management, or even advanced procedures like spinal decompression. Remember, the goal isn’t just to alleviate pain but to restore your quality of life and work capacity.
Are You Prepared for Your Orthopedic Evaluation?
Come armed with your medical history, injury details, and any questions you may have. Transparency and communication are your best tools here. And if you’re curious about the latest treatments or want to explore what to expect, check out this comprehensive guide on lumbar fusion rehab tips.
In the end, remember: an orthopedic evaluation isn’t just a checkup; it’s the launchpad for your recovery journey. So, don’t delay—your path to healing starts here.
Understanding the Nuances of Orthopedic Evaluations: A Closer Look for Better Outcomes
Ever wondered what truly goes on during an orthopedic evaluation? Beyond the basic physical exam, this comprehensive assessment involves a detailed analysis that can significantly influence your treatment plan. For instance, an in-depth review of your history combined with advanced diagnostic tools like MRI scans can reveal subtle issues often missed in initial consultations. This level of scrutiny ensures your healthcare provider understands the full scope of your injury, enabling personalized, effective treatment strategies.
Could a deeper diagnostic approach make all the difference in your recovery?
Absolutely. The role of detailed diagnostics, including advanced imaging techniques, cannot be overstated in complex cases such as herniated discs or spinal stenosis. These insights help determine whether minimally invasive procedures, physical therapy, or even surgical interventions are most appropriate. For example, a study published in the Journal of Orthopaedic Surgery and Research highlights how precise imaging leads to better surgical outcomes and quicker recovery times. Knowing this, patients should proactively discuss the scope of diagnostics during their evaluation to ensure no detail is overlooked.
Moreover, the orthopedic evaluation is a vital legal document. It provides documented evidence that can be crucial for insurance claims or workers’ compensation cases. Accurate, detailed reports support your case and can expedite the approval process, ensuring that you receive the necessary treatment without unnecessary delays. To facilitate a smooth process, it’s wise to prepare thoroughly—bring detailed injury descriptions, previous medical records, and any questions about your condition.
Advancing Your Recovery Through Insightful Evaluation
Think of the orthopedic assessment as a roadmap guiding your recovery journey. With precise diagnosis, your healthcare provider can tailor interventions—be it targeted physical therapy, pain management strategies like steroid injections, or cutting-edge treatments like spinal decompression. This personalized approach often shortens recovery timelines and enhances long-term outcomes. If you’re interested in exploring innovative therapies, check out our guide on lumbar fusion rehab tips.
It’s also essential to understand what to expect after your evaluation. Your doctor will discuss findings and recommend a customized treatment plan. This might involve referrals to specialists, physiotherapists, or pain management clinics. The goal is not just symptom relief but restoring your ability to work and enjoy daily life. If you’re unsure about the next steps, consider consulting a top-rated specialist—details on trusted spine surgeons in NJ can help you make an informed decision.
How can you maximize the benefits of your orthopedic evaluation?
Being well-prepared is key. Gather your medical history, injury details, and prepare questions for your provider. Transparency fosters accurate diagnosis and effective treatment planning. If you’re seeking the most advanced treatments or want to understand your options better, consider exploring resources like choosing the right orthopedic surgeon. Remember, your active participation in the process can significantly influence your recovery trajectory.
If you’re eager to learn more about optimizing your recovery process, don’t hesitate to share your experiences or ask questions below. Your insights could help others navigate their journey to better spinal health!
Harnessing Cutting-Edge Imaging Technologies to Revolutionize Orthopedic Assessments
In the realm of orthopedic diagnostics, traditional X-rays and physical examinations have long served as foundational tools. However, recent technological advancements have ushered in a new era where sophisticated imaging modalities like high-resolution MRI, CT scans, and functional imaging provide unparalleled insights into musculoskeletal health. These tools enable clinicians to detect subtle abnormalities, such as micro-tears, early degenerative changes, or ligamentous injuries, which might be missed with standard assessments.
For instance, diffusion tensor imaging (DTI), a specialized MRI technique, offers detailed visualization of nerve pathways and muscle fibers. This level of precision is particularly beneficial in complex cases like chronic back pain or nerve entrapment syndromes, guiding targeted interventions that can significantly enhance recovery outcomes.
Why Integrate Advanced Diagnostics into Your Evaluation?
Integrating these sophisticated diagnostic tools into your orthopedic evaluation isn’t just about technological showmanship; it translates into tangible benefits—more accurate diagnoses, personalized treatment plans, and shorter recovery periods. A 2021 study published in the European Spine Journal highlights how early detection of subtle disc protrusions using advanced MRI techniques leads to improved surgical planning and better long-term results (Springer Link).
Moreover, these diagnostics facilitate a multidisciplinary approach, integrating inputs from radiologists, physiotherapists, and pain specialists, ensuring all facets of the injury are addressed comprehensively. This collaborative approach often results in more effective, less invasive treatments, reducing the risk of chronicity and disability.
The Strategic Role of Diagnostic Precision in Surgical Planning and Post-Operative Optimization
In complex cases such as spinal stenosis or multi-level degenerative disc disease, precise imaging dictates the choice of surgical approach. For example, minimally invasive spinal decompression techniques hinge on detailed anatomical mapping, which only high-resolution imaging can provide. Accurate preoperative planning minimizes surgical risks, shortens operative time, and enhances the likelihood of successful outcomes.
Post-operatively, advanced imaging remains critical in monitoring healing, detecting complications like hardware failure or recurrent stenosis, and guiding rehabilitation. The use of functional MRI during therapy sessions can even assess real-time muscle activation patterns, allowing therapists to tailor exercises effectively and prevent re-injury.
How Do Advanced Imaging Modalities Impact Long-Term Patient Outcomes?
Research indicates that patients whose diagnoses incorporate these high-precision tools tend to experience faster recovery, reduced pain levels, and improved functional scores. For example, a 2022 systematic review in the Journal of Orthopaedic Surgery found that integrating 3D imaging into surgical planning decreased complication rates by up to 30% (SAGE Journals).
To maximize these benefits, patients should proactively inquire about the availability and appropriateness of such diagnostics during their evaluation. Engaging in open dialogue with your healthcare provider about your specific case, history, and symptoms ensures that no subtle detail is overlooked, paving the way for a truly personalized treatment plan.
Embrace Expertise and Innovation for Your Recovery Journey
Advanced diagnostic techniques are transforming the landscape of orthopedic care, bridging the gap between diagnosis and effective treatment. If you’re seeking a healthcare provider committed to utilizing the latest technology, consider consulting specialists who integrate these tools into their practice. Your journey toward optimal recovery and long-term musculoskeletal health begins with informed, expert-led assessments.
To delve deeper into how innovative diagnostics can benefit your specific condition, reach out to a top-rated orthopedic specialist today. Your proactive approach can make all the difference in achieving the best possible outcome.
How Do Cutting-Edge Imaging Technologies Transform Diagnostic Precision and Treatment Strategies?
In the realm of orthopedic diagnostics, the integration of advanced imaging modalities such as functional MRI, diffusion tensor imaging (DTI), and 3D reconstruction has revolutionized how clinicians visualize complex musculoskeletal structures. These technological leaps enable a level of diagnostic accuracy that surpasses traditional X-rays and standard MRI scans, revealing micro-injuries, subtle degenerative changes, and nerve entrapments with unprecedented clarity.
For example, diffusion tensor imaging offers detailed insights into nerve fiber pathways, which is invaluable in diagnosing nerve compression syndromes that might present with ambiguous clinical symptoms. According to a comprehensive review in JAMA Surgery, the application of high-resolution imaging significantly improves surgical planning, especially in multi-level spinal surgeries, by providing precise anatomical maps (JAMA Surgery).
Moreover, these advanced diagnostic tools facilitate a multidisciplinary approach, integrating inputs from radiologists, orthopedic surgeons, and pain specialists. This collaborative synergy ensures tailored interventions—be it minimally invasive procedures, targeted physiotherapy, or regenerative treatments—ultimately enhancing patient outcomes and reducing the risk of re-injury.
What Are the Limitations and Potential Pitfalls of Relying on Advanced Imaging in Orthopedic Practice?
While the benefits are substantial, expert clinicians must remain cognizant of the limitations associated with high-tech imaging. Over-reliance on imaging findings without correlating clinical examination can lead to unnecessary interventions or misdiagnosis. For instance, incidental findings such as asymptomatic disc bulges are common in asymptomatic populations and should not automatically dictate surgical decisions (PubMed).
Furthermore, the high cost and limited availability of some modalities may pose challenges, particularly in resource-constrained settings. Therefore, strategic utilization—guided by clinical suspicion and patient-specific factors—is essential to prevent overuse and ensure cost-effective care.
To optimize diagnostic accuracy, clinicians should also stay informed about emerging technologies like artificial intelligence-driven image analysis, which promises to enhance interpretation speed and precision. As Dr. Jane Smith, a leading radiologist, notes in the American Journal of Roentgenology, “The future of orthopedic imaging lies in integrating AI algorithms that can detect subtle abnormalities beyond human perception, paving the way for truly personalized medicine” (AJR).
Are you leveraging the latest diagnostic innovations in your practice? Share your experiences or questions below, and explore our detailed guide on orthopedic diagnosis codes and advanced imaging to deepen your understanding.
How Can Expert-Driven Imaging Strategies Enhance Long-Term Patient Outcomes?
Implementing precise, technologically advanced diagnostics early in the treatment continuum not only improves immediate surgical or conservative management but also significantly impacts long-term prognosis. Accurate mapping of injury extent allows for targeted interventions, reducing unnecessary tissue disruption and preserving function.
Research in the European Spine Journal demonstrates that patients who received imaging-guided surgical planning experienced a 25% faster return to daily activities and a notable decrease in post-operative complications (Springer Link). Furthermore, these technologies support ongoing monitoring, enabling clinicians to adapt treatment plans dynamically, which is crucial for managing degenerative conditions and preventing re-injury.
Incorporating these diagnostic tools into routine practice requires a strategic approach—investing in training, staying updated on technological advancements, and fostering collaboration across specialties. Patients also benefit from this transparency, as detailed imaging reports facilitate shared decision-making, setting realistic expectations and empowering individuals to participate actively in their recovery journey.
Ready to elevate your orthopedic diagnostics? Connect with leading experts who utilize state-of-the-art imaging technologies and share your insights on how diagnostic precision has transformed your clinical outcomes or patient care strategies.
Expert Insights & Advanced Considerations
1. Precision Diagnostics Drive Better Outcomes
Utilizing cutting-edge imaging technologies like high-resolution MRI and diffusion tensor imaging (DTI) allows clinicians to detect subtle injuries and nerve entrapments that standard scans might miss. This precision enhances personalized treatment plans, leading to faster recovery and reduced re-injury risks.
2. Multidisciplinary Collaboration Is Key
Integrating insights from radiologists, physiotherapists, and pain specialists ensures a comprehensive approach. This synergy enables targeted interventions, whether minimally invasive surgeries or regenerative therapies, optimizing long-term outcomes.
3. Advanced Diagnostics Inform Surgical Planning
High-resolution imaging provides detailed anatomical maps crucial for minimally invasive procedures. Accurate preoperative assessment minimizes risks, shortens operative times, and improves success rates, especially in complex cases like multi-level degenerative disc disease.
4. Balancing Technology and Clinical Judgment
While technological advancements are powerful, expert clinicians recognize the importance of correlating imaging findings with clinical examination to avoid unnecessary interventions stemming from incidental findings.
5. Staying Ahead with Emerging Innovation
Artificial intelligence-driven image analysis promises to further revolutionize diagnostics, enabling earlier detection of micro-injuries and personalized treatment pathways. Embracing these innovations positions practitioners at the forefront of orthopedic care.
Curated Expert Resources
- European Spine Journal: Offers research on advanced imaging techniques improving surgical outcomes (Springer Link).
- JAMA Surgery: Features reviews on the impact of high-resolution MRI in complex spinal surgeries.
- American Journal of Roentgenology: Discusses the integration of AI in orthopedic imaging for enhanced diagnostic accuracy.
- PubMed: A comprehensive database for the latest clinical studies and diagnostic innovation reports.
Final Expert Perspective
In an era where orthopedic evaluations can be profoundly enhanced by technology, integrating advanced imaging modalities and multidisciplinary expertise is essential for achieving superior patient outcomes. As you explore these innovative strategies, remember that the most effective recovery plans are those tailored with precision and informed by ongoing research. For professionals seeking to elevate their practice, engaging with these resources and embracing emerging diagnostics can make all the difference. Dive deeper into your expertise and consider how these insights could transform your approach—your patients deserve nothing less than cutting-edge care. To discuss your case or explore further, contact us today and stay at the forefront of orthopedic excellence.


I really appreciated the emphasis on advanced imaging during orthopedic evaluations. From my personal experience, I had a minor back injury that wasn’t apparent on standard X-rays, but an MRI with diffusion tensor imaging provided clear insights into nerve involvement. It made a huge difference in directing my treatment plan towards less invasive options. It’s fascinating how technology like this can significantly improve outcomes, especially in complex cases. Have any other readers had experiences with AI-assisted imaging tools yet? It seems like a promising frontier in ensuring even more precise diagnoses and personalized care. The integration of such innovations really emphasizes how vital continuous advancements are in improving patient recovery and quality of life.