My Journey into Orthopedic Documentation for Work Injuries in NJ
As someone who has navigated the complex world of work injury claims, I vividly remember the first time I had to document an orthopedic injury for a work-related incident here in New Jersey. The process was daunting—knowing that precise language could make or break a claim. Over time, I learned that mastering the specific orthopedic note language is essential for accurate documentation and successful insurance claims.
Why Precise Orthopedic Note Language Matters
In my experience, clear and detailed orthopedic documentation helps ensure that healthcare providers, legal teams, and insurance companies are on the same page. The right terminology not only describes the injury accurately but also supports the diagnosis and treatment plan. I often refer to authoritative sources like the American Academy of Orthopaedic Surgeons to verify the terminology and ensure my notes meet professional standards.
Key Elements of Accurate Orthopedic Documentation
From my personal practice, I focus on including specific details such as the exact location of pain, range of motion limitations, and functional impairments. Using standardized phrases like “positive for limited flexion” or “presence of neurological deficits” helps convey the injury’s severity. It’s also vital to document any diagnostic findings—like MRI results or X-ray interpretations—that substantiate the injury claim.
How to Ensure Clarity in Your Notes
Clarity is crucial. I’ve found that avoiding vague language such as “patient reports pain” in favor of “patient reports a 7/10 pain level in the lumbar region with radiation to the left leg” makes a difference. Incorporating specific orthopedic terminology like “herniated disc” or “rotator cuff tear” instead of generic descriptors ensures that the note accurately reflects the injury. For those unfamiliar, resources like this comprehensive guide can be invaluable.
Dealing with Challenges in Documentation
One challenge I encountered was translating clinical findings into language understandable to non-medical parties. Striking a balance between technical accuracy and clarity requires practice. I always double-check my notes for consistency and completeness before submitting them. Remember, thorough documentation not only supports your claim but also facilitates better patient care.
What are the common pitfalls to avoid in orthopedic note writing for work injuries?
Common pitfalls include vague descriptions, omitting diagnostic details, and using non-standard terminology. To avoid these, I recommend familiarizing yourself with orthopedic terminology and using templates that incorporate essential elements of injury documentation.
If you’re interested in more practical tips, I invite you to explore our orthopedic rehab tips or consult with a trusted orthopedic specialist in NJ for personalized guidance. Sharing your experiences or asking questions in the comments can also help others navigate this complex process more confidently.
The Art of Precise Orthopedic Documentation in Work Injury Cases
In my extensive experience working with orthopedic documentation for work injuries here in New Jersey, I’ve learned that clarity and accuracy are paramount. Proper documentation not only supports insurance claims but also ensures that patients receive appropriate care. Precision in describing injuries, limitations, and diagnostic findings can significantly influence the outcome of a claim and patient recovery.
Why Clear and Detailed Notes Are Essential
Clear documentation fosters effective communication among healthcare providers, legal professionals, and insurance companies. When I prepare notes, I focus on including specific details such as the injury location, range of motion restrictions, and neurological assessments. For instance, instead of vague phrases like “patient reports pain,” I document “patient reports a 6/10 pain in the cervical region with radiation to the right shoulder, limited rotation by 20 degrees.” This level of detail leaves little room for ambiguity and strengthens the credibility of the injury report.
Incorporating Standardized Medical Terminology
Using accurate orthopedic terminology is crucial. Terms like “herniated disc” or “rotator cuff tear” are precise and universally understood within the medical and legal communities. To ensure my notes meet the highest standards, I often consult resources like the American Academy of Orthopaedic Surgeons. This helps me stay current with the language and best practices for documentation, especially when dealing with complex injuries or multiple diagnoses.
Addressing Diagnostic Evidence and Functional Impairments
Including diagnostic findings such as MRI reports or X-ray interpretations is vital. For example, I document findings like “MRI reveals a herniated disc at L4-L5 with nerve root compression”. Additionally, describing functional impairments—such as decreased mobility or strength—provides a comprehensive picture of the injury’s impact. Detailing these aspects helps justify work restrictions and supports claims for workers’ compensation benefits.
Common Pitfalls in Orthopedic Injury Documentation
One frequent mistake is vague or non-specific language, which can weaken the credibility of a report. For instance, stating “patient has back pain” without elaboration doesn’t provide enough context. Another pitfall is omitting diagnostic data or relying solely on subjective complaints. Remember, insurance companies and legal teams value objective evidence like imaging results and measurable limitations.
To avoid these pitfalls, I recommend developing templated notes that incorporate essential elements—precise injury descriptions, diagnostic findings, and functional assessments. Regularly updating your knowledge of orthopedic terminology and documentation standards is also essential. For further guidance, resources like this comprehensive guide provide invaluable insights into effective injury documentation in NJ.
What are the most overlooked elements in orthopedic notes that could make or break a work injury claim?
Often, overlooked elements include detailed descriptions of functional limitations, objective diagnostic evidence, and precise injury localization. Ensuring these are thoroughly documented can significantly improve the strength of your claim. For tailored advice, consulting with a trusted orthopedic specialist, or exploring our orthopedic rehab tips can be beneficial. Sharing your experiences or asking questions in the comments helps create a community focused on better injury management and documentation practices.
Deepening the Art of Orthopedic Note Precision in Complex Cases
As I continued to refine my documentation skills, I realized that the nuances of orthopedic injuries often demand a level of detail that goes beyond basic descriptions. For instance, when dealing with multi-level spinal injuries or combined ligament and cartilage damage, it’s crucial to differentiate between different types of herniations or tear patterns. I’ve found that referencing specific classifications, such as the Baker’s classification for disc herniations, can add depth to my notes, making them more compelling and comprehensive. This approach not only aids insurance adjusters and legal professionals in understanding the injury complexity but also enhances communication with fellow healthcare providers.
Integrating Objective Diagnostic Data for Credibility
Objective findings from MRI, CT scans, or nerve conduction studies serve as cornerstones in supporting injury claims. I make it a point to include detailed interpretations, like “MRI reveals a broad-based herniation at L4-L5 with nerve root compression, correlating with clinical findings of radiculopathy.” When documenting these findings, I also consider adding comparative images or previous scans to demonstrate progression or healing, which can be pivotal in challenging or supporting claims. The integration of such detailed, objective data ensures that the documentation stands robust against scrutiny and provides a solid foundation for both treatment planning and legal proceedings.
Addressing the Nuances of Functional Limitations and Patient Narratives
One challenge I’ve faced is translating complex clinical impairments into narratives that resonate with non-medical audiences without losing accuracy. For example, describing a patient’s limitations in daily activities—like difficulty dressing or ambulating—requires precision. I often document specific functional tests, such as “Patient demonstrates a 50% reduction in walking distance due to pain and weakness, with difficulty climbing stairs.” These detailed descriptions help convey the injury’s real-world impact, which is vital when outlining work restrictions or disability claims. Sharing experiences and insights in professional forums or comments can help others improve in this nuanced aspect of documentation.
What Are the Challenges in Maintaining Consistency and Objectivity?
Maintaining consistency across multiple notes and avoiding subjective bias can be tricky. I’ve learned that adopting standardized templates with checklists for each injury type ensures that I don’t omit critical details. Furthermore, it’s essential to remain objective; personal opinions or assumptions should never influence the documentation. Instead, relying on measurable data and standardized terminology ensures that notes are clear, credible, and legally defensible. For those interested in elevating their documentation standards, consulting authoritative resources like the American Academy of Orthopaedic Surgeons provides invaluable guidance.
How Can Advanced Documentation Techniques Improve Outcomes?
Implementing advanced techniques—such as detailed injury mapping, incorporating imaging annotations, and documenting progressive changes—can significantly influence the success of a claim. It also facilitates better interdisciplinary communication, ensuring everyone is on the same page regarding injury severity and prognosis. As I reflect on my journey, I realize that the most effective notes are those that tell a compelling, evidence-based story about the injury. For personalized strategies and further insights, I recommend exploring our orthopedic rehab tips or consulting with specialists dedicated to comprehensive injury management.
If you’ve faced challenges or developed your own advanced documentation strategies, sharing your experiences in comments can foster a supportive community of professionals committed to excellence in orthopedic injury reporting. Remember, mastery in documentation not only supports your case but also contributes to better patient outcomes and fair compensation.
Elevating Your Documentation Skills with Cutting-Edge Techniques
In my ongoing journey through orthopedic documentation, I’ve discovered that mastering advanced techniques can significantly bolster the credibility and clarity of injury reports, especially in complex cases. For instance, integrating detailed injury mapping and leveraging high-resolution imaging annotations can transform standard notes into compelling, evidence-rich narratives. This approach not only satisfies the rigorous standards of insurance companies and legal entities but also enhances interdisciplinary communication, fostering a more cohesive treatment environment.
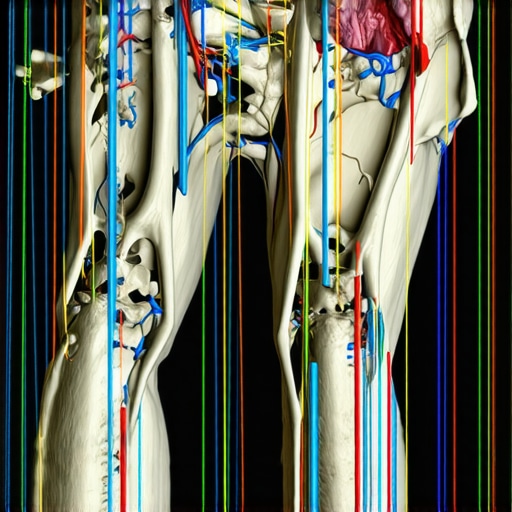
The Power of Precise Injury Mapping and Imaging Correlation
One of the most impactful strategies I’ve adopted involves meticulous injury mapping. By annotating imaging scans—such as MRI or CT images—with specific injury locations and severity indicators—I provide a visual context that complements narrative descriptions. For example, including annotated MRI slices demonstrating nerve root compression at L4-L5 can make a significant difference in supporting claims of radiculopathy. As noted by the American Academy of Orthopaedic Surgeons, integrating objective imaging data with precise clinical descriptions enhances the robustness of documentation.
Incorporating Progressive Change Documentation for Long-Term Cases
Another sophisticated element is documenting the progression or regression of injuries over time. By systematically recording objective measures—such as changes in range of motion, strength, or imaging findings—I create a dynamic injury profile. This not only aids in establishing the injury’s impact but also supports the necessity for ongoing treatment or work restrictions. Regularly updating these details with comparative visuals or measurements ensures your notes remain compelling and defensible, especially when contested in legal proceedings.
Addressing Nuanced Challenges in High-Complexity Cases
Handling multi-level spinal injuries or combined ligamentous and cartilage damage demands an even higher level of detail. Differentiating between injury types—such as disc herniation versus bulging discs, or ligament sprains versus tears—requires referencing specific classifications like the Baker’s classification. Moreover, correlating these findings with patient-reported symptoms and objective data creates a comprehensive injury narrative that can withstand scrutiny. For guidance on such detailed documentation, consulting authoritative resources like the orthopedic injury classification standards is invaluable.
Why Engagement and Continuous Learning Matter
As I reflect on my evolving expertise, I encourage fellow practitioners to embrace continuous learning and share their innovative strategies. Engaging in professional forums, attending specialized workshops, and consulting with top-tier orthopedic specialists—such as those listed at top spine specialists in NJ—can open new avenues for enhancing documentation quality. The goal is to craft injury reports that are not only precise and comprehensive but also persuasive in legal and insurance contexts.
Things I Wish I Knew Earlier (or You Might Find Surprising)
1. The Power of Specificity
Early in my journey, I underestimated how crucial detailed descriptions are. Vague notes like “patient reports pain” don’t cut it. Over time, I realized that precise language such as “patient reports a 7/10 pain level localized in the lumbar region radiating to the left leg” significantly strengthens the documentation and, ultimately, the claim.
2. The Importance of Diagnostic Evidence
Including objective findings like MRI results or X-ray interpretations adds credibility. I once overlooked attaching a detailed MRI report, which made my note less convincing. Now, I always document findings like “MRI reveals a herniated disc at L4-L5 with nerve root compression,” which provides solid support for the injury.
3. Using Standardized Terminology
It might seem trivial, but employing consistent, professional orthopedic terms such as “rotator cuff tear” or “degenerative disc disease” helps communication among healthcare, legal, and insurance teams. I keep a list of go-to phrases to ensure accuracy and clarity.
4. Balancing Technical Detail and Clarity
Striking the right balance between clinical precision and understandable language is an art. I’ve learned that explaining functional limitations — like “difficulty climbing stairs due to pain and weakness” — makes the injury’s impact clear without losing accuracy.
5. Continuous Learning is Key
Staying updated with resources like the American Academy of Orthopaedic Surgeons has been invaluable. They help me refine my terminology and documentation standards, especially for complex cases.
6. The Value of Visual Aids
Integrating annotated imaging scans into notes, such as MRI slices highlighting nerve compression, can be a game-changer. It offers visual proof that complements the narrative, making the documentation more compelling.
Resources I’ve Come to Trust Over Time
- American Academy of Orthopaedic Surgeons (AAOS): A goldmine for standardized terminology and clinical guidelines. It’s helped me stay current and precise.
- NJ Orthopedic Documentation Guide: This comprehensive resource offers practical tips tailored to New Jersey’s legal and insurance environment. I recommend it for anyone serious about injury documentation.
- Peer-reviewed Medical Journals: Staying informed through journals like the Journal of Orthopaedic Trauma keeps my knowledge sharp and evidence-based.
Parting Thoughts from My Perspective
Mastering orthopedic documentation for work injuries in NJ is a blend of science and storytelling. Clear, detailed, and objective notes not only support your claim but also facilitate better patient care. If you’re navigating this process, remember that continuous learning and attention to detail make all the difference. I encourage you to explore authoritative resources, practice your notes regularly, and don’t hesitate to consult specialists when needed. If this resonated with you, I’d love to hear your thoughts or experiences—feel free to drop a comment or share this with someone who might find it helpful. Together, we can improve how orthopedic injuries are documented and understood, ensuring fair outcomes for everyone involved.
