When Pain Strikes, Trigger Points Take the Spotlight
Imagine waking up every morning with a nagging knot in your shoulder or a stubborn ache lurking in your lower back. It’s the kind of pain that sneaks up during your day-to-day hustle, turning simple tasks into a test of endurance. Enter the orthopedic trigger point injection—a clever, minimally invasive remedy that’s been quietly revolutionizing pain management for years.
Trigger Points: The Hidden Culprits Behind Chronic Orthopedic Pain
Trigger points, those tiny hypersensitive knots in your muscles, are often the villains behind mysterious aches and stiffness. Orthopedic specialists have long recognized these sore spots as prime targets for injection therapies that deliver fast, effective relief. By injecting a small amount of anesthetic — sometimes combined with steroids — directly into these knots, the muscle relaxes, and pain diminishes, often dramatically.
Is This the Magic Bullet for Your Muscle Pain?
That’s the million-dollar question. While orthopedic trigger point injections are far from a one-size-fits-all cure, they offer a powerful option in the pain relief arsenal, especially when conservative treatments like physical therapy hit a wall. Patients often report feeling like they’ve hit the “reset” button on their muscle pain after just one session.
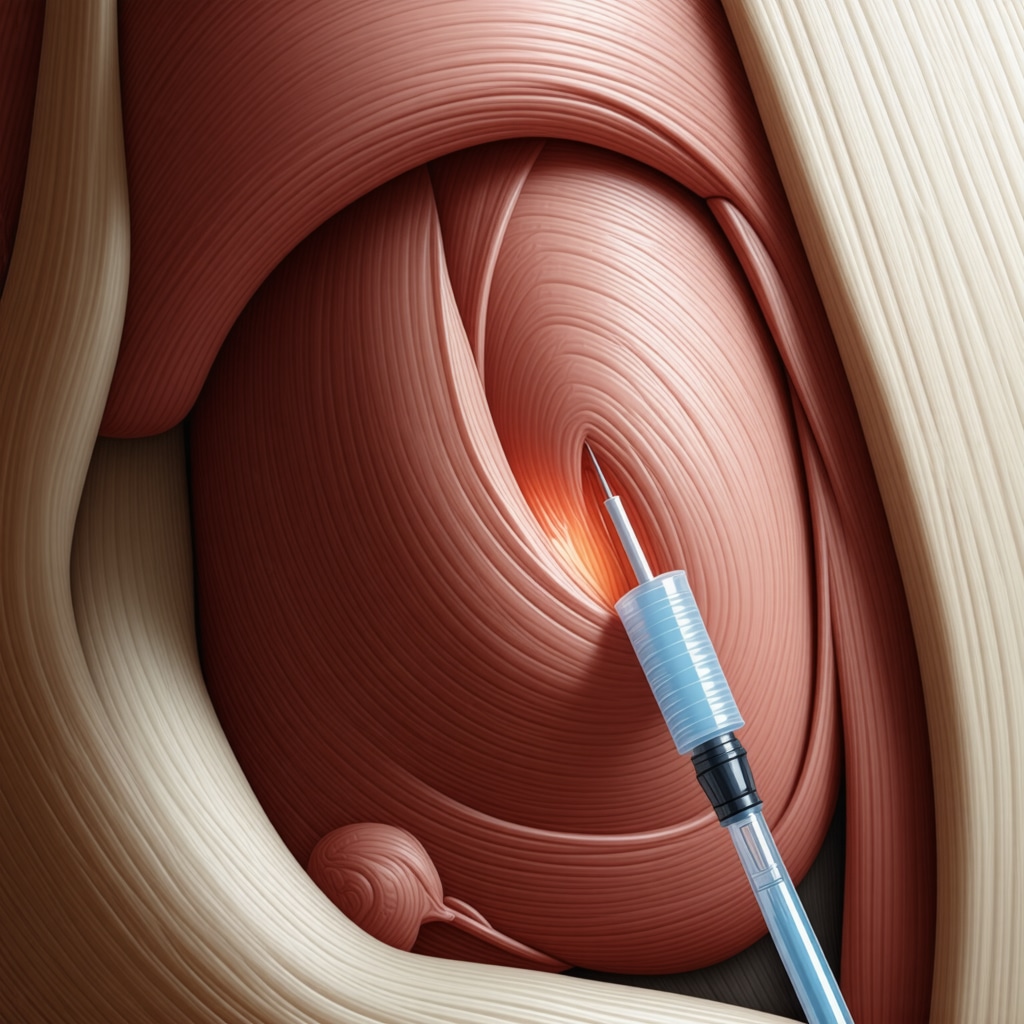
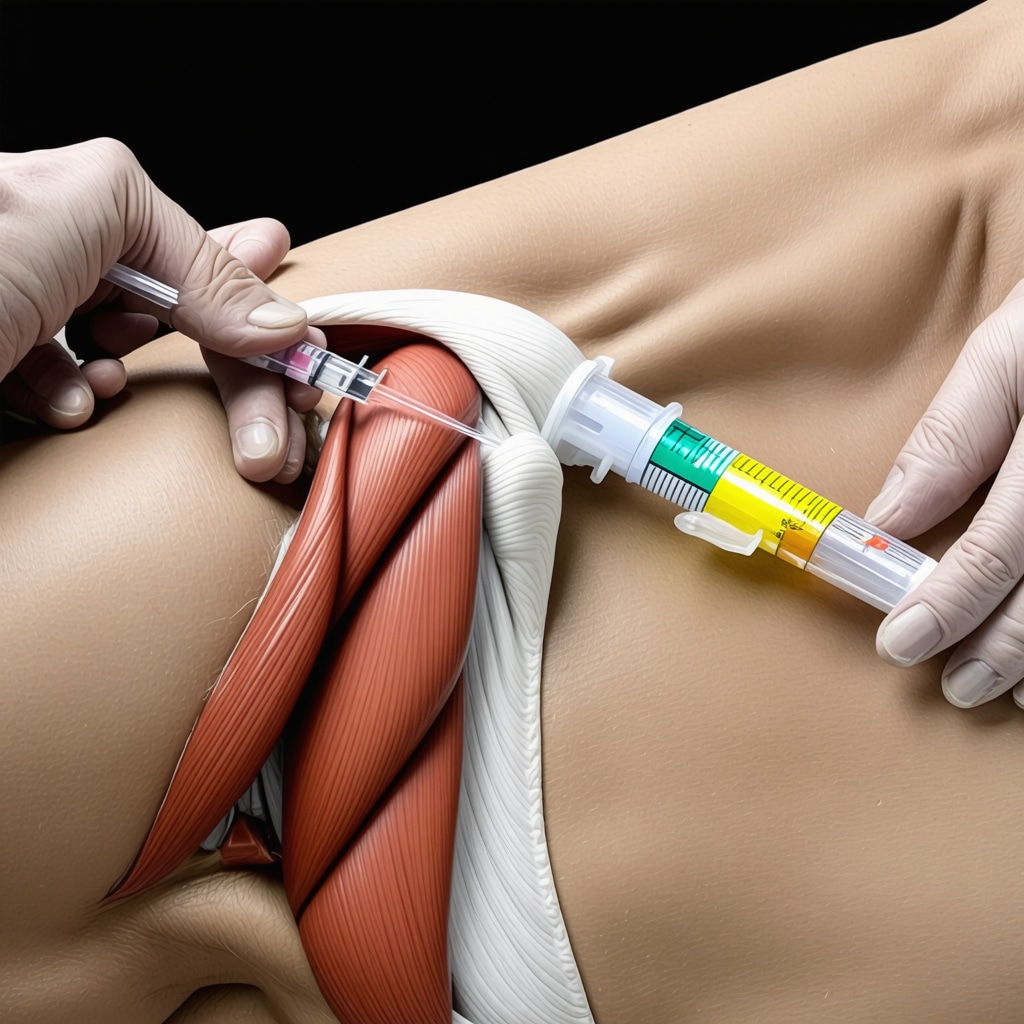
Behind the Scenes: What to Expect During Your Injection
Curious about the process? The procedure is typically quick and performed in a comfortable outpatient setting. Your orthopedic doctor will palpate the muscle to locate the trigger point, cleanse the skin, and then deliver the injection with precision. Some patients feel a brief sting, followed by a sense of loosened muscle tension. It’s a straightforward approach that can be repeated as needed, with minimal downtime.
Trigger Point Injections in the Bigger Picture of Orthopedic Care
Of course, injections aren’t the entire story. They work best as part of a comprehensive treatment plan, including rehabilitation exercises and lifestyle adjustments. For those navigating complex conditions like herniated discs or back pain, combining injections with expert orthopedic advice can be transformative. If you’re interested in exploring non-surgical options for back pain, check out this insightful guide on effective non-surgical care for herniated discs.
Can You Trust This Treatment? The Expert Verdict
Research backs up the anecdotal success. A 2022 review published in The Journal of Pain Research confirms that trigger point injections can significantly reduce localized musculoskeletal pain with a favorable safety profile. However, as with any procedure, patient selection and technique are crucial to outcomes. That’s why partnering with a top-notch orthopedic specialist is key.
Curious about how trigger point injections might fit into your pain management journey? Share your experiences or questions below—we’d love to hear your story and help you find relief that sticks.
Integrating Trigger Point Injections with Holistic Orthopedic Care
While trigger point injections serve as a potent tool against muscular pain, their success is amplified when synchronized with broader orthopedic strategies. Incorporating physical therapy tailored specifically to address the affected muscle groups helps reinforce the benefits of injections. Strengthening exercises, posture correction, and ergonomic adjustments form the foundation for sustained recovery and prevention of re-injury.
Moreover, understanding the biomechanics and lifestyle factors that contribute to trigger point formation can empower patients to actively participate in their healing journey. For instance, patients suffering from chronic back pain may benefit from exploring minimally invasive options as detailed in our comprehensive guide on minimally invasive back pain treatments.
What Are the Potential Risks and How Are They Managed?
As with any medical procedure, trigger point injections carry some risks, albeit generally minimal. Common side effects include temporary soreness at the injection site, minor bruising, or slight bleeding. More rarely, patients may experience allergic reactions or infections, which necessitate prompt medical attention. An experienced orthopedic specialist employs sterile techniques and patient screening to mitigate these risks effectively.
Importantly, setting realistic expectations is vital. Trigger point injections may need to be part of a recurring treatment schedule, especially for chronic conditions, and are rarely a permanent cure alone. Combining injections with therapies like nerve block management or comprehensive rehabilitation can enhance long-term outcomes.
Could Trigger Point Injections Replace Surgery for Certain Orthopedic Conditions?
This question often arises among patients exploring their pain relief options. While injections offer a valuable alternative to more invasive surgeries, they are generally recommended as part of conservative management rather than a complete replacement. The decision depends on several factors including the severity of the condition, the patient’s overall health, and response to initial treatments.
Orthopedic experts emphasize the importance of thorough diagnosis and personalized care plans. For example, patients with herniated discs might first attempt trigger point injections combined with physical therapy before considering surgical interventions. To gain more insight into this approach, visit our effective non-surgical care guide.
Evidence-Based Support for Trigger Point Therapy
According to a systematic review published in The Journal of Pain Research, trigger point injections demonstrate significant efficacy in reducing localized musculoskeletal pain, with a favorable safety profile when administered properly. The review highlights the importance of combining injections with physical therapy and lifestyle modifications to achieve the best functional outcomes.
Furthermore, emerging studies are investigating novel injectates such as botulinum toxin and platelet-rich plasma (PRP), which may offer enhanced therapeutic benefits, though these require further validation.
Engage with Us: Share Your Orthopedic Pain Management Experiences
Have you undergone trigger point injections or integrated them into your orthopedic treatment plan? Your insights can be invaluable to others navigating similar pain challenges. We invite you to comment below with your questions, experiences, or tips for maximizing treatment benefits.
If you’re keen to deepen your understanding of orthopedic care options or want to explore expert advice on selecting the right spine specialist, consider visiting our detailed resource on choosing the right orthopedic surgeon for your spine.
Synergizing Trigger Point Injections with Cutting-Edge Orthopedic Rehabilitation Techniques
Delving deeper beyond the traditional scope, the integration of trigger point injections within advanced orthopedic rehabilitation protocols exemplifies a nuanced approach to pain management. Rather than viewing injections as isolated interventions, contemporary orthopedic specialists advocate for their incorporation alongside neuromuscular reeducation, proprioceptive training, and dynamic stabilization exercises. These modalities not only complement the immediate analgesic effects of trigger point injections but also facilitate long-term neuromuscular adaptations, minimizing recurrence of muscle hypersensitivity.
For instance, combining injections with electromyographic (EMG) biofeedback enables patients to gain real-time insight into muscle activation patterns, enhancing voluntary control of affected muscle groups. This sophisticated synergy underscores the importance of interdisciplinary collaboration between orthopedic physicians, physical therapists, and pain specialists to tailor individualized treatment plans that address both symptom relief and functional restoration.
How Do Emerging Injectates Like Botulinum Toxin and Platelet-Rich Plasma Elevate Trigger Point Therapy?
The landscape of trigger point therapy is evolving with promising injectates such as botulinum toxin (BoNT) and platelet-rich plasma (PRP), which introduce novel mechanisms of action. BoNT, a neurotoxin that inhibits acetylcholine release at the neuromuscular junction, induces prolonged muscle relaxation, thereby attenuating trigger point activity beyond transient anesthetic effects. Clinical trials have demonstrated BoNT’s efficacy in refractory myofascial pain syndromes, particularly when traditional anesthetic injections fail to deliver sustained relief.
Similarly, PRP harnesses autologous growth factors to potentiate tissue healing and modulate inflammation within muscular trigger points. Early-phase studies suggest that PRP injections may accelerate recovery by promoting muscle regeneration and reducing nociceptive sensitization. However, these innovative approaches necessitate further robust clinical evidence to delineate optimal dosing protocols, patient selection criteria, and long-term safety profiles.
According to a 2023 systematic review published in The Clinical Journal of Pain, both BoNT and PRP represent promising adjuncts to conventional trigger point injections but must be contextualized within comprehensive multimodal pain management frameworks.
Personalizing Trigger Point Injection Strategies: The Role of Precision Medicine in Orthopedic Pain Management
Recent advances in biomarker research and musculoskeletal imaging have catalyzed a paradigm shift toward precision medicine in orthopedic care. Tailoring trigger point injection strategies based on individual patient profiles—including genetic predispositions, inflammatory markers, and muscle tissue characteristics—enables clinicians to optimize therapeutic efficacy and minimize adverse effects.
For example, ultrasound-guided injection techniques afford unparalleled accuracy in targeting deep-seated trigger points while avoiding neurovascular structures. Moreover, integrating elastography can quantify muscle stiffness to objectively identify pathological trigger points, enhancing diagnostic precision.
Personalized approaches also extend to pharmacological considerations, where metabolic profiles and comorbidities inform the choice of injectates and dosing schedules. These advances underscore a move away from the conventional “one-size-fits-all” mindset toward nuanced, patient-centric care paradigms that maximize functional outcomes and quality of life.
As we continue to unravel the complexities of musculoskeletal pain, it becomes evident that trigger point injections are not merely symptom modulators but integral components of sophisticated, multifactorial orthopedic treatment algorithms. Staying abreast of emerging evidence and technological innovations will be pivotal for clinicians striving to deliver state-of-the-art care.
Why Precision Medicine Is Transforming Trigger Point Injection Outcomes
In the evolving field of orthopedic pain management, the shift toward precision medicine is reshaping how trigger point injections are administered. Gone are the days of generic protocols; today’s specialists leverage individualized patient data—ranging from genetic markers to detailed musculoskeletal imaging—to customize treatment. This approach not only enhances the accuracy of injections but also optimizes therapeutic efficacy and minimizes adverse events.
Ultrasound guidance, for instance, has become indispensable, enabling clinicians to visualize the exact location and depth of trigger points, especially those embedded in deep or complex muscle groups. Incorporation of elastography further refines this targeting by quantifying muscle stiffness, thereby objectively differentiating pathological trigger points from normal muscle tissue. Such technological advancements ensure that injections are delivered with pinpoint precision, enhancing patient comfort and outcomes.
Can Integrating Novel Injectates Like Botulinum Toxin and PRP Revolutionize Chronic Myofascial Pain Management?
Emerging injectates such as botulinum toxin (BoNT) and platelet-rich plasma (PRP) are heralding a new frontier in trigger point therapy. BoNT impedes acetylcholine release at neuromuscular junctions, inducing sustained muscle relaxation beyond the transient effects of local anesthetics. This mechanism has shown promise in refractory myofascial pain syndromes where conventional injections have limited success.
Similarly, PRP delivers concentrated autologous growth factors that facilitate tissue regeneration and modulate inflammatory responses within trigger points. Preliminary clinical trials suggest that PRP may accelerate muscle healing and reduce nociceptive sensitization, although standardized protocols and long-term data remain under investigation.
According to a 2023 systematic review published in The Clinical Journal of Pain, these novel injectates represent promising adjuncts to traditional therapies but must be integrated thoughtfully within comprehensive, multimodal orthopedic pain management plans.
Maximizing Recovery: How Multidisciplinary Collaboration Enhances Injection Therapy Success
Trigger point injections achieve their highest value when embedded within a multidisciplinary framework. Collaboration among orthopedic surgeons, physical therapists, pain specialists, and rehabilitation experts creates a synergistic environment that addresses both symptom relief and functional restoration. Techniques such as neuromuscular reeducation, proprioceptive training, and biofeedback complement the pharmacological effects of injections, fostering durable neuromuscular adaptations and minimizing recurrence.
For patients recovering from complex procedures or chronic conditions, integrating injection therapy with targeted orthopedic rehabilitation—such as protocols outlined in our rehabilitation tips after lumbar fusion surgery—can substantially improve outcomes and quality of life.
Patient Empowerment: The Role of Education and Lifestyle Modification in Sustaining Pain Relief
Ultimately, patient engagement remains pivotal in harnessing the full benefits of trigger point injections. Educating patients on biomechanics, ergonomic practices, and lifestyle factors that predispose them to trigger point formation empowers proactive participation in their recovery journey. Regular exercise, posture optimization, and stress management strategies can reduce muscular overload and prevent the reemergence of painful knots.
Those interested in exploring comprehensive non-surgical options for spinal health can benefit from resources like our guide on minimally invasive back pain treatments, which complements trigger point therapies with broader orthopedic care insights.
We invite you to share your experiences or questions about advanced trigger point injection therapies and integrated orthopedic care in the comments below. Your insights help build a community dedicated to informed, patient-centric pain management.
Expert Insights & Advanced Considerations
Precision Medicine is Elevating Trigger Point Injection Outcomes
Incorporating patient-specific factors such as genetic markers and musculoskeletal imaging advances trigger point injections from a generic treatment to a precision-guided therapy. Techniques like ultrasound and elastography enable clinicians to target pathological trigger points with unparalleled accuracy, improving efficacy and minimizing complications.
Multidisciplinary Collaboration Enhances Long-Term Pain Management
Trigger point injections achieve superior outcomes when integrated within a multidisciplinary framework. Orthopedic surgeons, physical therapists, and pain specialists working together facilitate neuromuscular reeducation, proprioceptive training, and biofeedback, which complement injection therapy and reduce recurrence rates.
Emerging Injectates Offer Promising Adjuncts but Require Careful Integration
Novel injectates such as botulinum toxin and platelet-rich plasma show potential for sustained relief and tissue regeneration in refractory myofascial pain syndromes. However, these require further clinical validation and must be incorporated thoughtfully into comprehensive multimodal treatment plans.
Patient Empowerment Through Education and Lifestyle Modification Is Crucial
Educating patients on biomechanics, ergonomic practices, and stress management empowers them to prevent trigger point recurrence and sustain pain relief. Active patient participation is essential for maximizing the benefits of injection therapy and overall orthopedic recovery.
Curated Expert Resources
- The Journal of Pain Research: A peer-reviewed source providing comprehensive reviews on trigger point injection efficacy and safety, essential for evidence-based practice.
- The Clinical Journal of Pain: Offers systematic reviews on emerging injectates like botulinum toxin and PRP, highlighting novel therapeutic avenues.
- Complete Guide to Orthopedic Trigger Point Injections: An authoritative resource detailing procedure techniques, patient selection, and integration with rehabilitation.
- Understanding the Multidisciplinary Orthopedic Care Model Today: Explores collaborative approaches that optimize injection therapy outcomes.
- Guide on Minimally Invasive Back Pain Treatments: Complements trigger point injection knowledge with broader orthopedic care insights.
Final Expert Perspective
Trigger point injections stand at the intersection of evolving orthopedic pain management strategies, blending precision medicine, innovative injectates, and multidisciplinary rehabilitation. Their role transcends simple symptom relief, becoming a vital component of personalized, comprehensive care plans that prioritize functional restoration and patient empowerment. Staying informed about the latest evidence and emerging technologies enables both clinicians and patients to harness the full potential of trigger point therapies.
We encourage you to engage further—explore expert resources like our comprehensive injection guide or connect with specialists listed in Top Orthopedic Spine Specialists to Trust in 2025. Your insights and questions enrich this evolving conversation and help shape the future of orthopedic pain management.

