My Journey with Orthopedic Trigger Point Injections: What I Wish I Knew
When I first started experiencing persistent muscle pain that just wouldn’t quit, I felt overwhelmed and unsure about my treatment options. After trying various therapies, my orthopedic specialist recommended trigger point injections. At first, I was skeptical about this minimally invasive procedure, but learning about its benefits and what to expect truly changed my perspective.
Understanding Trigger Point Injections Through My Eyes
Trigger point injections target tight knots or “trigger points” in muscles that cause referred pain and discomfort. Personally, I found it fascinating how a small injection of anesthetic and corticosteroid could bring such noticeable relief. My doctor explained that these injections help relax the muscle fibers and reduce inflammation, which aligns with what Mayo Clinic describes as the primary purpose of this treatment.
What Should You Expect During the Procedure? Insights from My Experience
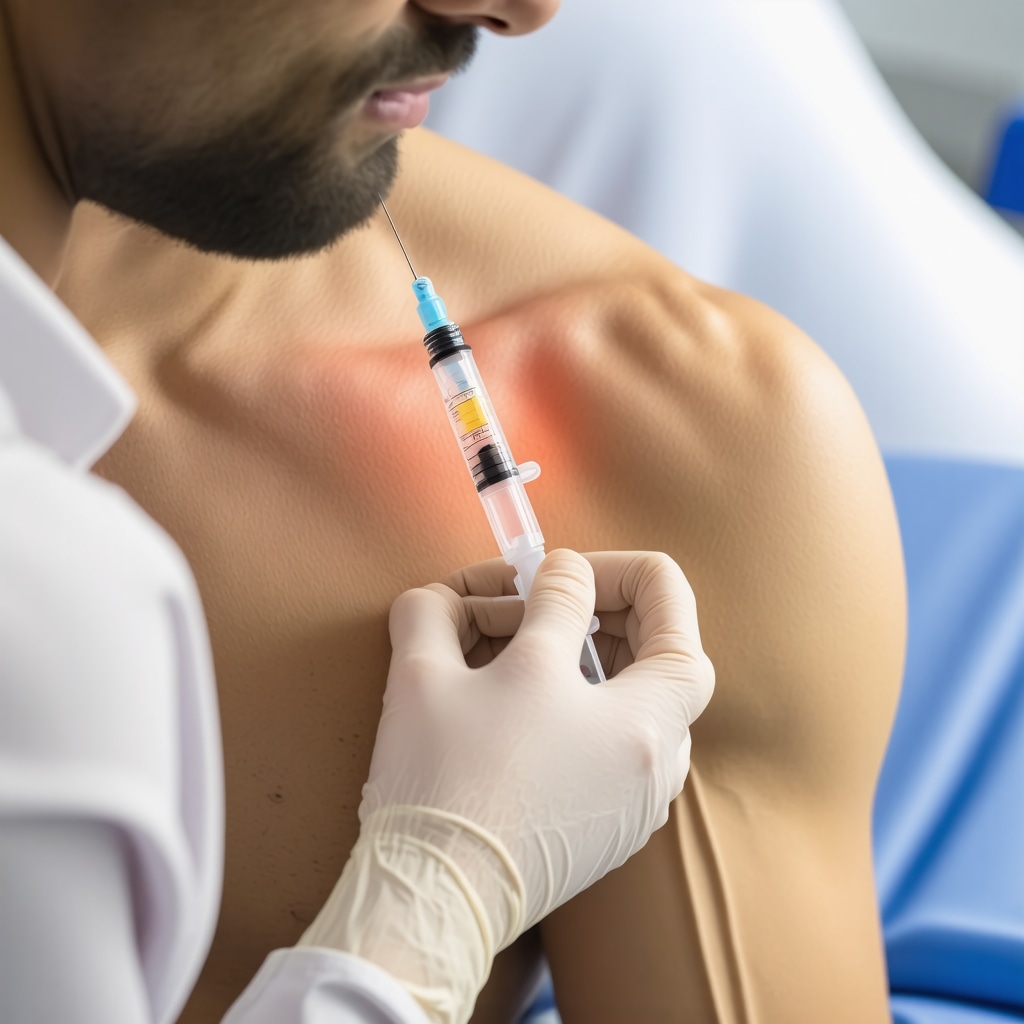
The procedure itself was relatively quick and straightforward. After cleaning the site, the doctor used a fine needle to inject the medication directly into the painful trigger points. I appreciated that the discomfort was minimal, just a slight sting. The key takeaway for me was the importance of communicating openly with your orthopedic doctor about your pain levels during the injection.
How Long Does Relief Last and Are There Risks I Should Know About?
Relief varies from person to person. In my case, I felt significant improvement within a few days, and the effects lasted several weeks. However, it’s important to be aware of potential side effects like soreness, bruising, or infection, though these are uncommon. Discussing these risks candidly with your provider ensures you feel confident and prepared.
Why I Believe Orthopedic Trigger Point Injections Are Worth Considering
From my journey, these injections are a valuable option when conservative treatments fall short. They offer targeted relief without the need for surgery or prolonged medication use. If you’re navigating chronic muscle pain, learning about minimally invasive options like this could be empowering. For those interested in accompanying therapies, exploring orthopedic physical therapy can complement injection benefits remarkably well.
If you’ve undergone trigger point injections or are considering them, I’d love to hear your thoughts and experiences. Sharing our stories can help others facing similar challenges feel less alone and more informed. Feel free to leave a comment below or reach out for more personalized advice.
When to Consider Repeat Orthopedic Trigger Point Injections: An Expert’s Perspective
While many patients experience significant relief after a single trigger point injection, it’s important to recognize that chronic muscle pain may require a series of treatments. Orthopedic specialists often recommend repeat injections spaced several weeks apart to maintain symptom control and facilitate long-term muscle relaxation. However, timing and frequency must be individualized, considering factors such as the patient’s response, underlying condition, and any concurrent therapies.
Understanding this nuanced approach can help patients set realistic expectations and collaborate effectively with their orthopedic care team. For example, if you’re undergoing orthopedic physical therapy, combining it with trigger point injections may optimize outcomes by addressing both muscular tightness and functional mobility.
How Do Trigger Point Injections Compare With Other Orthopedic Pain Management Techniques?
From an expert viewpoint, it’s crucial to differentiate trigger point injections from other pain management modalities such as steroid injections for joint inflammation or nerve block injections. Trigger point injections specifically target myofascial pain sources, whereas other injections may address different pain etiologies. This targeted approach often results in faster relief for muscle-related pain but may not address joint or nerve pathology effectively.
Understanding these distinctions assists patients in navigating treatment options wisely. If you’re unsure whether trigger point injections are appropriate for your pain, consulting an orthopedic specialist can clarify the best path forward. Exploring related treatments like steroid injections or nerve block injections may also be valuable depending on your diagnosis.
Can the Effectiveness of Orthopedic Trigger Point Injections Be Enhanced by Integrating Advanced Imaging Techniques?
Recent advances in musculoskeletal medicine have incorporated ultrasound guidance to precisely locate trigger points before injection, enhancing accuracy and potentially improving outcomes. Ultrasound-guided injections allow orthopedic specialists to visualize muscle anatomy in real time, ensure the needle targets the exact painful area, and avoid adjacent structures.
Studies published in journals like The Journal of Orthopaedic & Sports Physical Therapy highlight that ultrasound guidance can reduce procedural discomfort and increase the efficacy of trigger point injections, especially in complex or deep muscle groups. This technique is becoming a gold standard in orthopedic pain management, underscoring the importance of seeking specialists proficient in these advanced methods.
Patient Empowerment Through Knowledge and Communication
As with any orthopedic intervention, patient education and open communication with your healthcare provider are paramount. Discussing your full medical history, current medications, and prior treatment experiences helps tailor trigger point injection protocols appropriately. Moreover, understanding the potential side effects, post-procedure care, and realistic expectations for pain relief fosters a collaborative therapeutic relationship.
If you’re curious about integrating minimally invasive treatments or want to learn more about comprehensive orthopedic care for muscle pain, exploring resources like minimally invasive back pain treatments can provide valuable insights.
Have you tried trigger point injections or other orthopedic pain management techniques? Sharing your experience in the comments can create a supportive community and guide others navigating similar challenges. Feel free to reach out for personalized consultation or recommendations.
Reflections on the Subtleties of Post-Injection Care and Long-Term Success
One aspect of trigger point injections that often gets overlooked in initial consultations is the nuanced aftercare and how it plays a crucial role in the overall success of the treatment. From my personal experience and discussions with orthopedic specialists, the days following the procedure are a delicate balance of rest and gentle movement. Too much inactivity can cause the muscles to stiffen again, while overexertion risks aggravating the injection site. This subtlety highlighted for me the importance of individualized guidance, which is why orthopedic physical therapy often becomes an essential adjunct to injections, helping maintain muscle flexibility and optimize healing.
Can Orthopedic Trigger Point Injections Address Complex Myofascial Pain Syndromes Effectively?
This question came up frequently in my conversations with patients facing chronic, multifocal muscle pain. While trigger point injections provide targeted relief, they are not a panacea for widespread myofascial pain syndromes, which often involve central sensitization and overlapping nerve dysfunction. Orthopedic experts emphasize that in such cases, injections should be integrated into a multimodal approach including physical therapy, pain management, and sometimes behavioral health support. The comprehensive care model ensures that both the peripheral muscle tightness and central pain processing abnormalities are addressed. For those intrigued by the science behind these approaches, peer-reviewed literature sheds light on the complex interplay of factors that influence treatment outcomes.
From my viewpoint, understanding these complexities transforms a simple injection from a quick fix into a meaningful step within a broader therapeutic journey.
How I Learned the Importance of Patient Advocacy and Asking the Right Questions
During my treatment course, I realized that being an active participant rather than a passive recipient of care made a significant difference. Asking my orthopedic doctor about alternative therapies, possible side effects, and realistic timelines helped set clear expectations. It also empowered me to track my progress more effectively and report any new symptoms promptly.
For anyone embarking on this journey, I recommend preparing questions in advance and seeking providers who welcome open dialogue. Resources like connecting directly with orthopedic specialists can facilitate this process, offering tailored advice beyond general information.
Exploring Advanced Techniques: Ultrasound Guidance and Beyond
As I delved deeper into the subject, I discovered how ultrasound-guided injections, as mentioned earlier, significantly improve precision and patient comfort. But innovations continue to emerge, including combined therapies with platelet-rich plasma (PRP) or botulinum toxin for refractory cases. While these are not standard first-line treatments, awareness of evolving options can be valuable for patients whose pain persists despite conventional care.
Keeping informed through reputable sources and ongoing conversations with your orthopedic team is key. For example, reviewing insights on minimally invasive back pain treatments can broaden understanding of how orthopedic care adapts to patient needs.
Have you encountered advanced injection techniques or integrated therapies in your pain management? Sharing your story helps build a nuanced community where knowledge and experience enrich everyone’s healing path.
Delving Deeper Into Post-Injection Recovery: Strategies Beyond the Basics
My journey with orthopedic trigger point injections revealed that the immediate aftermath is just as critical as the procedure itself. Beyond the standard advice to rest and avoid strenuous activity, I learned the value of subtle movement and muscle activation exercises tailored to my condition. These nuanced post-injection strategies, often overlooked in general consultations, can significantly influence recovery trajectory and long-term relief. Engaging in carefully guided orthopedic physical therapy, as detailed in this comprehensive resource, helped me maintain flexibility and prevent re-tightening of muscles while minimizing inflammation.
Integrating Multidisciplinary Approaches for Complex Orthopedic Pain Management
Trigger point injections are powerful tools, yet their full potential is unlocked when integrated within a multidisciplinary framework. During my treatment, collaborating with pain specialists, physical therapists, and sometimes behavioral health professionals allowed for a holistic approach addressing both peripheral muscle issues and central sensitization phenomena. Such synergy is particularly vital for patients with multifaceted myofascial pain syndromes, where isolated interventions often fall short.
How Does Emerging Research on Neuromodulation Influence Orthopedic Trigger Point Injection Protocols?
Recent investigations into neuromodulation techniques provide an exciting frontier that could redefine trigger point injection efficacy. Modalities such as transcutaneous electrical nerve stimulation (TENS) and peripheral nerve stimulation, when combined with injections, have shown promise in modulating pain pathways and enhancing muscular relaxation. According to a detailed review in The Journal of Orthopaedic & Sports Physical Therapy, these integrative approaches may reduce the frequency of injections needed and improve patient satisfaction. Exploring these options with your orthopedic team could open new doors in personalized pain management.
Understanding these advanced therapies demands an empowered patient mindset. I encourage readers to actively inquire about cutting-edge treatments and how they might fit into their individualized care plans. If you’re navigating chronic muscle pain and eager to explore sophisticated orthopedic care options, don’t hesitate to connect with experienced specialists who can tailor these innovations to your unique needs.
Things I Wish I Knew Earlier (or You Might Find Surprising)
The Subtle Art of Post-Injection Movement
One thing that caught me off guard was how important gentle movement was after the injection. Initially, I thought complete rest was best, but I learned that carefully guided, subtle exercises help prevent muscle stiffness and support lasting relief. This was a game-changer in how I approached recovery.
Not All Pain Is Created Equal
I used to lump all muscle pain together, but trigger point injections taught me the importance of pinpointing exact pain sources. Understanding that myofascial trigger points differ from joint or nerve pain helped me appreciate why targeted injections worked better than broader treatments.
Patient Advocacy Is More Than a Buzzword
Asking questions, sharing concerns, and staying proactive with my specialist made a huge difference. I realized that being an engaged patient—not just a passive recipient—can shape your treatment journey and outcomes significantly. Prepare your questions and don’t hesitate to seek clarity.
Advanced Imaging Really Matters
Discovering ultrasound-guided injections was eye-opening. Knowing that your doctor can visually confirm needle placement adds a level of precision that enhances comfort and effectiveness, especially for deep or tricky muscle areas.
Integrating Therapies Creates Synergy
I found that pairing injections with orthopedic physical therapy was far more beneficial than either alone. The injections ease muscle tightness, while therapy builds strength and flexibility. This combination helped me maintain results and avoid repeat procedures.
Chronic Pain Often Calls for a Team Approach
Trigger point injections helped, but for complex or widespread pain, I saw how combining pain specialists, therapists, and sometimes mental health support forms a comprehensive plan. Pain is multifaceted, and addressing it from multiple angles is often necessary for long-term success.
Resources I’ve Come to Trust Over Time
Mayo Clinic: Their clear, patient-friendly explanations on trigger point injections helped me understand the basics and feel more confident about the procedure. I recommend their pages for anyone starting their research.
The Journal of Orthopaedic & Sports Physical Therapy: For a deeper dive into ultrasound guidance and neuromodulation, their studies offer evidence-based insights that helped me appreciate evolving orthopedic techniques.
PubMed: When I wanted to explore the science behind complex myofascial pain syndromes and treatment outcomes, PubMed’s peer-reviewed articles were invaluable. It’s a go-to for credible, in-depth orthopedic research.
Orthopedic Physical Therapy Insights: I found this detailed guide particularly helpful in understanding how therapy complements injections and why it matters for recovery.
Comprehensive Pain Management Resources: Exploring minimally invasive back pain treatments expanded my view on how orthopedic care integrates various modalities beyond injections.
Parting Thoughts from My Perspective
Reflecting on my experience with orthopedic trigger point injections, what stands out most is how these treatments, while seemingly simple, are part of a nuanced journey. The injections provide targeted relief that can feel almost like a reset for stubborn muscle pain, but the real magic happens when combined with informed aftercare, physical therapy, and open communication with your care team. If you’re navigating chronic muscle discomfort, understanding the role of trigger point injections within a broader orthopedic plan can be empowering and hopeful.
If this resonated with you, I’d love to hear your thoughts or experiences. Sharing stories creates community and can guide others through similar challenges. Feel free to drop your insights in the comments or reach out for personalized advice. Remember, your journey is unique, and informed choices make all the difference.

I really appreciated the detailed walkthrough of what to expect with orthopedic trigger point injections. Like the author, I was initially hesitant about this treatment, especially because I wasn’t sure how targeted injections could provide lasting relief for muscle pain. It was insightful to learn how the small doses of anesthetic and corticosteroids work together to relax muscle fibers and reduce inflammation. From my experience, one challenge following the injections was figuring out the right balance of rest and gentle movement—I found that too much inactivity made the muscles stiffen again, while pushing myself too hard caused discomfort at the injection site. Integrating orthopedic physical therapy after the injections truly made a difference for me in maintaining the relief and improving mobility. I’m curious how others have navigated this post-injection phase? Have you found particular exercises or movement routines that work best to prevent the return of muscle tightness? Also, for those who needed multiple treatments, how did you and your care team decide on the optimal timing between injections? It seems like open communication and personalized protocols are so crucial for success.
Reading about the experience with trigger point injections really resonated with me, especially the part about the importance of communication during the procedure. I remember feeling nervous initially, but knowing I could voice my pain levels and ask questions made a big difference. In my case, I found that gentle stretching and staying mobile after the injections helped prolong relief, similar to what the author described. However, I also struggled with balancing activity and rest, as I was tempted to push too hard early on. Has anyone had success with specific physical therapy routines to maintain muscle relaxation longer? On the topic of timing, I’m curious—what factors do others consider when determining how soon to undergo repeat treatments? It seems like each case requires a very personalized approach, which makes a lot of sense. Overall, I appreciate how this post emphasizes informed decision-making and working closely with your healthcare team. It reassures me that with proper guidance, trigger point injections can be a valuable tool in managing chronic muscle pain.
I found this personal account of trigger point injections very insightful, especially how the author emphasized the importance of communication during the procedure. In my experience, ensuring your doctor knows your pain levels in real-time can really influence the outcome and comfort level of the treatment. I agree that combining this with targeted physical therapy has helped many patients, including myself, maintain the relief longer. One challenge I faced was determining the optimal timing for repeat injections—sometimes it took a few adjustments to find the right interval. Has anyone else found that tracking symptoms diligently helped in planning these treatments more effectively? I also wonder about the role of emerging imaging techniques like ultrasound guidance—I’ve read they can improve accuracy and reduce discomfort. Have others had experiences with these advanced methods? Overall, this post underscores how a personalized and well-informed approach can make trigger point injections a highly effective component of managing chronic muscle pain.
Reading through this personal experience with trigger point injections really highlights the importance of patience and ongoing communication with your healthcare provider. It’s interesting how the relief can vary so much from person to person, and how critical timing and consistent follow-up are to manage chronic muscle pain effectively. I’ve found that incorporating gentle stretching and targeted physical therapy after injections can really help prolong the benefits, much like what’s described here. I also wonder, for those who’ve undergone repeated treatments, how do you decide on the frequency? Do you track your symptoms or rely on your doctor’s input? Overall, this post is a great reminder that personalized care and staying engaged in your treatment plan are key to success.