My Personal Encounter with Chronic Back Pain and the First Questions I Had
It all started a few years ago when I began experiencing persistent lower back pain after a long day at work. At first, I thought it was just muscle strain, but as weeks went by, the discomfort worsened, affecting my daily activities. Like many, I was faced with the crucial decision: should I consult an orthopedic specialist or a neurologist? This dilemma led me on a journey to understand how these two types of doctors can help with back pain.
Understanding the Roles: Orthopedic vs Neurologist
From my research and conversations with healthcare professionals, I learned that orthopedic doctors specialize in the musculoskeletal system, including bones, joints, ligaments, tendons, and muscles. They are often the go-to experts for structural issues like herniated discs, spinal stenosis, or fractures.
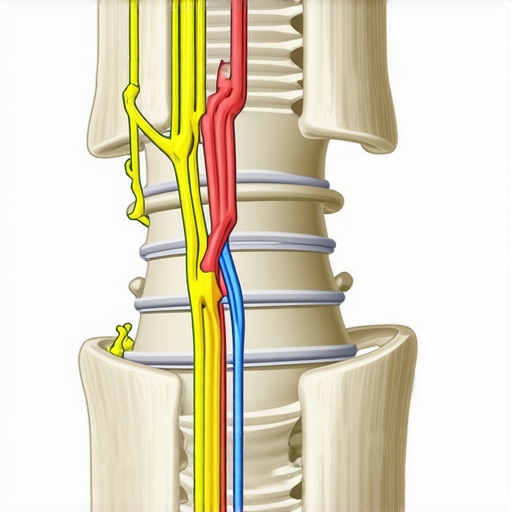
On the other hand, neurologists focus on the nervous system—brain, spinal cord, and peripheral nerves. If your back pain involves nerve compression, nerve pain, or symptoms like numbness or weakness, a neurologist might be the right specialist to see.
My Experience: When to See an Orthopedic Specialist
In my case, the pain was localized and seemed related to my posture. After visiting an orthopedic surgeon, I underwent diagnostic imaging, which confirmed I had a herniated disc. The orthopedic specialist recommended non-invasive treatments like physical therapy and spinal support braces, which proved effective. The expertise of orthopedic doctors in diagnosing and managing structural problems was invaluable during my recovery.
When Do I Need a Neurologist? Recognizing Nerve-Related Symptoms
If your symptoms include shooting pain, numbness, tingling, or weakness radiating down your legs, a neurologist’s assessment becomes essential. They can perform nerve conduction studies or MRI scans focused on nerve health. For example, I found that understanding nerve involvement is crucial for targeted treatment, as explained by reputable sources like the American Academy of Neurology.
Is It Better to See Both? My Take on Comprehensive Care
Sometimes, a multidisciplinary approach is best. I was advised that consulting both specialists might be necessary if the cause of back pain is complex or not clearly diagnosed. This collaborative care ensures all aspects—skeletal and nerve health—are addressed.
What Should You Consider Before Choosing a Specialist?
Think about your symptoms, the severity of pain, and whether structural or nerve issues seem predominant. Visiting a trusted provider for an initial assessment can guide your next steps. For guidance on finding top-rated specialists, I recommend exploring this resource.
If you’re unsure where to start, don’t hesitate to contact a reputable clinic like the one at this link. Remember, timely care can make a significant difference in recovery and quality of life.
Share your experiences or questions in the comments below! I believe that understanding your options empowers you to make the best decision for your health.
Deciphering the Nuances: Is Your Back Pain Structural or Nerve-Related?
Understanding the root cause of back pain is crucial for effective treatment. Structural issues like herniated discs or spinal stenosis often require a different approach than nerve-related problems such as pinched nerves or radiculopathy. As an orthopedic specialist, I emphasize the importance of accurate diagnosis through detailed imaging and clinical evaluation to determine the primary source of your discomfort.
Advanced Diagnostic Techniques for Precise Identification
Modern diagnostic tools like MRI scans and nerve conduction studies allow us to differentiate between skeletal abnormalities and nerve impairments. For example, an MRI can reveal disc herniation pressing on nerve roots, while nerve conduction tests assess the functional status of the nervous system. Consulting with a multidisciplinary team ensures that both aspects are thoroughly evaluated for comprehensive care.
Practical Approach: When to Opt for an Orthopedic Surgeon vs a Neurologist
If your pain is localized, persistent, and worsens with movement, an orthopedic consultation is often appropriate initially. However, if symptoms include shooting pain, numbness, weakness, or tingling radiating down the limbs, a neurologist’s expertise becomes invaluable. Sometimes, these symptoms overlap, and a collaborative approach between both specialists can optimize recovery outcomes. To explore top-rated providers, visit this resource.
The Power of a Multidisciplinary Team in Complex Cases
Complex back pain cases benefit from multidisciplinary care, integrating orthopedic and neurological expertise. This approach not only ensures accurate diagnosis but also tailors treatment plans that address both structural and nerve issues. For example, a patient with a herniated disc causing nerve compression may undergo minimally invasive procedures complemented by targeted physical therapy, enhancing recovery and reducing recurrence risk. Discover more about advanced treatments at this link.
How Can I Tell If My Back Pain Warrants Urgent Medical Attention?
Recognizing red flags such as sudden weakness, loss of bladder or bowel control, or severe pain unrelieved by rest is critical. These symptoms may indicate urgent conditions like cauda equina syndrome, requiring immediate intervention. If you experience any of these signs, consult an orthopedic or neurosurgeon promptly. For guidance on when to seek urgent care, check this resource.
If you’re navigating the complex landscape of back pain, sharing your questions or experiences can be invaluable. Comment below or reach out to a trusted specialist to ensure you receive the most appropriate care for your situation.
Unraveling the Complexity: My Personal Reflection on Structural and Nerve-Related Back Pain
Having navigated the labyrinth of back pain myself, I realize how deceptively simple it can seem at first—just a dull ache or sharp twinge. But as I delved deeper into my diagnosis and treatment options, I uncovered a world where structural abnormalities and nerve issues intertwine in ways that can either complicate or clarify one’s path to recovery.
The Hidden Layers: Beyond the Surface Pain
Often, I found that what appears as a straightforward herniated disc or spinal stenosis isn’t just a matter of bones or discs alone. It’s the nerve roots, the intricate nervous pathways that amplify pain or cause numbness. For instance, a herniated disc pressing on a nerve root can mimic or exacerbate nerve-related symptoms, making the diagnostic process a delicate puzzle. This is why modern imaging techniques, like MRI scans, are invaluable—they let us see the structural damage and the nerve impingement simultaneously, guiding more targeted treatments.
My Deep Dive: The Intersection of Structural and Nerve Issues
One of the most profound lessons I learned is that a holistic approach—considering both the skeletal and nervous systems—is crucial when dealing with complex back pain. For example, even after structural interventions like minimally invasive surgeries, some patients experience lingering nerve symptoms if nerve health isn’t directly addressed. This insight isn’t just theoretical; it’s backed by authoritative sources like the American Academy of Neurology, emphasizing the importance of nerve assessments in persistent cases.
Is It Possible to Overlook One While Focusing on the Other?
This question haunted me during my journey—how often do we focus solely on correcting structural issues, ignoring nerve health, or vice versa? The truth is, overlooking one aspect can lead to incomplete recovery or chronic pain. I’ve seen patients who underwent successful spinal surgeries yet continued to suffer from nerve pain because nerve problems weren’t fully evaluated or treated. It’s a reminder that an integrated diagnostic and treatment plan is often the best route, especially for stubborn cases.
What Can You Do When Both Issues Are Present?
If you suspect your back pain involves both structural and nerve components, seeking a multidisciplinary team’s expertise is wise. This might include orthopedic surgeons, neurologists, and physiatrists working together. Besides imaging, nerve conduction studies can reveal nerve dysfunctions that might not be evident on scans alone. The goal is a comprehensive plan—combining structural repairs, nerve-specific therapies, and rehabilitative strategies—that addresses all facets of your condition.
Personal Wisdom: Listening to Your Body’s Subtle Signals
From my experience, paying attention to your body’s subtle signals can make all the difference. Numbness, tingling, or weakness often indicate nerve involvement, signaling that structural solutions alone won’t suffice. If you’re navigating this complex terrain, don’t hesitate to consult specialists who understand the nuanced interplay of bones, discs, and nerves. Find trusted providers at this resource.
Sharing and Learning from Personal Stories
Ultimately, my journey—and yours—may benefit from sharing experiences. If you’re confronting similar challenges, I invite you to comment below or reach out. Your story might resonate with someone else and inspire a more comprehensive, compassionate approach to back pain management. Remember, understanding these deep nuances isn’t just about alleviating pain; it’s about reclaiming your quality of life and confidence in your body’s resilience.
Keep exploring, stay curious about your health, and never settle for less than a full understanding of what your body is telling you. The road to recovery is often complex, but with the right knowledge and support, it’s also navigable.
Decoding the Subtle Interplay Between Structural and Nerve Pain: My Deep Dive
Throughout my extensive journey in orthopedic care, I have come to recognize that the boundary between structural and nerve-related back pain is often blurred, yet understanding their nuanced relationship is vital for effective treatment. It’s akin to deciphering a complex code where bones, discs, and nerves form an intricate network, each influencing the other in ways that require a sophisticated, layered approach to diagnosis and intervention.
My Reflection on the Complexity of Diagnostic Precision
One of the most eye-opening realizations in my practice is how modern imaging techniques, such as high-resolution MRI scans, have revolutionized our ability to pinpoint the exact origin of pain. For instance, when a herniated disc compresses a nerve root, the clinical presentation can mimic other nerve entrapments or musculoskeletal issues. The challenge lies in correlating imaging findings with clinical symptoms, especially when nerve impingement is subtle or multi-faceted. This is where a comprehensive evaluation—combining radiological data with nerve conduction studies—becomes indispensable, as highlighted by authoritative sources like the American Academy of Neurology.
Is It Possible to Overlook One Aspect While Focusing on the Other?
Absolutely. In my experience, a common pitfall is overly emphasizing structural correction—such as spinal fusion or discectomy—without fully addressing nerve health. Conversely, focusing purely on nerve decompression without considering the structural integrity can lead to incomplete relief. This dual oversight can prolong recovery or result in persistent symptoms. An integrated, multidisciplinary approach, involving both orthopedic and neurological expertise, ensures that both components are managed harmoniously, fostering a more durable resolution of pain and dysfunction.
How Can Specialized Nerve-Targeted Therapies Complement Structural Interventions?
Emerging therapies, like nerve blocks and neuromodulation techniques, serve as adjuncts to structural procedures, offering symptom relief and functional restoration. These methods are particularly effective when nerve irritation persists despite structural correction. For example, epidural steroid injections can mitigate inflammation around compressed nerve roots, providing a bridge to physical therapy and rehabilitation. Such integrated strategies are supported by recent innovations documented in the latest orthopedic innovations.
Personal Invitation to Share Your Journey
If you’ve navigated similar complexities, I encourage you to share your experiences or questions. Engaging with a community of informed individuals can be empowering, and exchanging insights often reveals overlooked nuances that can refine treatment choices. Remember, your body’s signals are a rich source of diagnostic clues—trust them, and seek expert guidance to decode the messages accurately. Feel free to connect for a personalized assessment or to explore tailored treatment options that address both structural and nerve components of your back pain.
Future Directions: Embracing a Multidimensional Approach
As the field advances, the integration of regenerative medicine, biologics, and personalized rehabilitation protocols promises to revolutionize how we approach complex back conditions. Staying informed about these innovations and collaborating across specialties ensures that patients benefit from holistic, cutting-edge care. My journey continues to be one of learning and adaptation, driven by a commitment to restoring health through nuanced, expert-driven strategies that recognize the intricate dance between bones, discs, and nerves.
Things I Wish I Knew Earlier (or You Might Find Surprising)
The Hidden Role of Nerves
Early in my journey with back pain, I underestimated how much nerves could be involved. I used to think that structural issues like herniated discs were the sole culprits, but I later learned that nerve impingement can amplify pain and cause numbness, making diagnosis trickier and treatment more nuanced.
The Power of Modern Imaging
When I finally got an MRI, I realized how critical detailed imaging is. It’s like seeing inside your body in high definition, revealing exactly where the problem lies—be it bones, discs, or nerves. This clarity can save you from unnecessary treatments and guide targeted therapy.
Listening to Your Body
Over the years, I’ve become more attuned to subtle signals—tingling, weakness, or shooting pains. These clues often indicate nerve involvement and shouldn’t be ignored. Recognizing these signs early can lead to prompt specialist visits and better outcomes.
The Value of a Multidisciplinary Approach
Sometimes, combining the expertise of orthopedic surgeons and neurologists provides the best results. I’ve seen cases where collaboration led to comprehensive care, addressing both structural and nerve issues for lasting relief.
Preventive Care Matters
Maintaining good posture, staying active, and seeking early assessment when symptoms start can prevent chronic issues. I wish I had prioritized prevention sooner, as it could have saved me from prolonged discomfort.
Resources I’ve Come to Trust Over Time
- American Academy of Neurology: Their guidelines helped me understand nerve-related symptoms better. It’s a reputable source used by many neurologists.
- National Institute of Neurological Disorders and Stroke: Offers comprehensive info on nerve and spinal conditions. I recommend it for trustworthy, up-to-date research.
- Harvard Health Publishing: Their articles on back pain and nerve health are clear and practical, perfect for patients seeking reliable advice.
Parting Thoughts from My Perspective
Dealing with back pain taught me that understanding whether the root cause is structural or nerve-related makes all the difference in treatment. Don’t hesitate to seek a thorough evaluation—modern diagnostics and a multidisciplinary team can offer the clarity you need. If this resonates with you, I’d love to hear your thoughts or experiences. Sharing our stories can empower us all to make better health decisions and find relief sooner. Remember, your body communicates in subtle ways—trust it and seek the expert help that suits your unique situation.

