How I Learned the Real Difference Between Orthopedic Surgeons and Neurosurgeons for Spine Care
When I first started experiencing persistent back pain that radiated down my leg, I was overwhelmed by the choices of specialists. Should I consult an orthopedic surgeon or a neurosurgeon? The distinction wasn’t clear to me initially, and the decision felt daunting because I wanted the best care for my spine.
After several consultations, personal research, and some trial and error, I finally grasped the crucial differences between orthopedic and neurosurgical spine care. This understanding helped me make informed choices and ultimately find the right treatment path.
Why My Experience With Spine Issues Made Me Dive Deeper Into Specialist Roles
My experience showed me that orthopedic surgeons specialize in the musculoskeletal system, focusing on bones, joints, ligaments, and muscles, including the spinal column. Neurosurgeons, on the other hand, focus more extensively on the nervous system — the brain, spinal cord, and nerves. Both can treat spine problems, but their approaches and expertise differ significantly.
For example, when I was diagnosed with a herniated disc compressing a nerve root, my orthopedic doctor emphasized structural correction and stability, often incorporating physical therapy and minimally invasive techniques. This approach aligned well with what I read in trusted sources like the American Academy of Orthopaedic Surgeons (AAOS), which clarified many of my doubts about orthopedic spine care.
So, How Do You Decide Between an Orthopedic Surgeon and a Neurosurgeon for Spine Issues?
This is a question I asked myself repeatedly. My takeaway is that if your spine condition primarily involves the bones, discs, or ligaments — especially if you’re considering joint replacement or spinal fusion — an orthopedic surgeon might be the best fit. If your problem centers more on nerve decompression, spinal cord tumors, or complex neurological issues, a neurosurgeon’s expertise is invaluable.
That said, many specialists now collaborate across these disciplines to provide comprehensive care. I found it helpful to check out detailed guides like this article that explain the nuances, which made my decision easier.
What I Wish I Knew Before Choosing My Spine Specialist
One insight I gained is that the best spine care often depends on the specific condition and the surgeon’s experience rather than the specialty alone. I recommend patients ask potential doctors about their spine surgery volume, success rates, and their preferred treatment methods. It’s also crucial to consider non-surgical options first — I found excellent resources on non-surgical herniated disc treatments that helped me manage pain without rushing into surgery.
If you’re navigating similar challenges, I encourage you to share your experiences or questions below. Your story might help others decide on the right path for their spine health.
Understanding Collaborative Approaches in Modern Spine Care
One aspect I discovered during my journey is the increasing collaboration between orthopedic surgeons and neurosurgeons. Complex spine issues often require a multidisciplinary approach that blends the strengths of both specialties. For example, in cases of severe spinal deformities or trauma, a team involving both types of specialists can optimize outcomes by addressing both the structural and neurological components.
This synergy is highlighted in clinical practices where combined surgical teams plan and execute interventions, ensuring comprehensive care. If you want to learn more about the nuances of choosing your spine doctor, consider reading this guide, which offers practical tips tailored for patients navigating such complex choices.
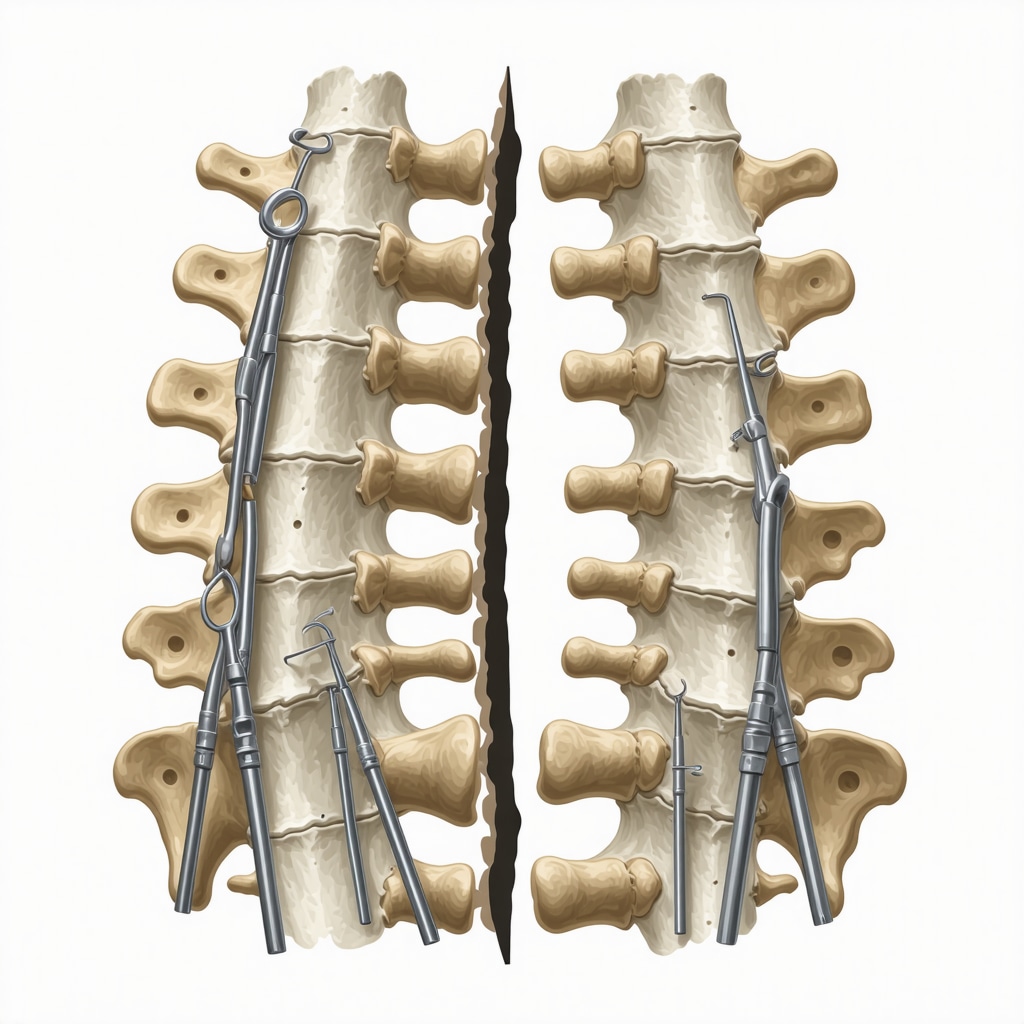
The Role of Minimally Invasive Techniques in Bridging Specialty Boundaries
Advancements in minimally invasive spine surgery have reshaped how both orthopedic surgeons and neurosurgeons treat spinal conditions. These methods aim to reduce tissue damage, shorten recovery times, and improve postoperative outcomes. During my research, I found that many orthopedic surgeons utilize minimally invasive approaches for lumbar fusion and decompression, which aligns with my own experience. These procedures often mean less pain and faster rehabilitation.
For those curious about these techniques, this resource explains the benefits and considerations of minimally invasive back pain treatments in detail.
How Do Surgeons Decide Between Surgical and Non-Surgical Spine Treatments?
This question intrigued me deeply, especially as I weighed my treatment options. The decision depends on various factors including the severity of symptoms, underlying pathology, patient health status, and response to conservative therapies. Orthopedic surgeons often emphasize starting with non-surgical care such as physical therapy, anti-inflammatory medications, or injections before recommending surgery. If symptoms persist or worsen, surgical intervention may then be considered.
Evidence-based guidelines from sources like the American Academy of Orthopaedic Surgeons affirm this stepwise approach to spine care, underscoring the importance of personalized treatment plans.1 This balanced perspective helped me understand that surgery is not always the immediate answer but rather part of a broader treatment continuum.
If you have insights or questions about how to navigate treatment choices, please share your thoughts in the comments. Engaging with others can provide valuable perspectives and support.
Reflecting on the Emotional Side of Choosing Your Spine Specialist
One thing that isn’t often discussed openly is the emotional rollercoaster involved in deciding between an orthopedic surgeon and a neurosurgeon for spine care. When I was in the thick of it, the stress wasn’t just about understanding medical jargon or weighing risks — it was also about trusting someone to intervene in such a sensitive part of my body. The spine isn’t just structural; it’s intimately tied to our sense of mobility, independence, and even identity.
I found that beyond medical expertise, the surgeon’s communication style and willingness to involve me in the decision-making process deeply influenced my confidence and peace of mind. Sometimes, it’s the subtle human qualities that make a big difference in healing, not just the credentials or the technical approach.
How Can You Assess a Spine Specialist’s Approach Before Surgery?
This question kept me up at night. I wanted to know if the surgeon would consider my lifestyle, pain tolerance, and personal goals — not just treat an X-ray finding. What helped me was preparing a list of questions centered on their treatment philosophy, typical patient outcomes, and how they handle complications. For example, many orthopedic surgeons today emphasize minimally invasive techniques to minimize recovery hurdles, as detailed in this insightful resource. Such approaches reflected my values of avoiding prolonged downtime and preserving as much natural function as possible.
What’s more, understanding how a surgeon collaborates with other specialists — like pain management experts or physical therapists — gave me reassurance that care would be holistic, not fragmented. If you’re curious about selecting a specialist who aligns well with your needs, exploring guides such as how to choose the right orthopedic surgeon for your spine can be invaluable.
The Subtle Nuances of Non-Surgical Care in Spine Issues: What I Learned
Throughout my journey, I realized that surgery is just one chapter in a broader narrative. Non-surgical options often serve as the foundation for lasting spine health. I delved into physical therapy regimes, lifestyle modifications, nerve blocks, and even alternative treatments recommended by orthopedic experts. For instance, understanding the role of orthopedic nerve blocks in managing chronic spine pain helped me navigate difficult flare-ups without immediately resorting to invasive measures (learn more here).
These strategies require patience and commitment, but they empower patients to be active participants in their healing. The American Academy of Orthopaedic Surgeons and other authorities emphasize this patient-centered, stepwise approach, which I found echoed in my own experience and research.1
Can Integrative Spine Care Change Outcomes for Complex Cases?
This was a question I pondered deeply, especially when conventional treatments plateaued. The answer, based on my encounters and recent studies, is often yes. Integrative approaches that combine orthopedic, neurosurgical, and rehabilitative expertise alongside pain management can tailor treatments to the subtleties of each patient’s condition — a concept I encourage every patient to explore.
If you’ve experienced or are considering integrative spine care, I invite you to share your stories or questions below. Your insights might illuminate paths for others facing similar challenges.
Delving Into the Complex Intersection of Orthopedic and Neurosurgical Spine Expertise
As my understanding of spine care deepened, I encountered scenarios where the boundaries between orthopedic surgery and neurosurgery blur, especially in complex cases involving both structural and neurological elements. This fusion of expertise became crucial when managing conditions such as severe spinal stenosis combined with nerve root impingement, where neither specialty alone could fully address the multifaceted challenges.
In these intricate situations, multidisciplinary teams often employ a hybrid approach, leveraging orthopedic surgeons’ proficiency in reconstructive techniques alongside neurosurgeons’ nuanced knowledge of neural tissue preservation. This collaborative model not only enhances surgical precision but also improves long-term functional outcomes. For patients navigating similar complexities, resources like guides on choosing the right orthopedic surgeon for spine care can provide invaluable insights into selecting specialists who prioritize integrative strategies.
How Do Advanced Imaging and Diagnostic Tools Influence Treatment Decisions Between Orthopedic Surgeons and Neurosurgeons?
This question became central to my journey as I grappled with understanding the rationale behind various diagnostic tests. Advanced imaging modalities such as high-resolution MRI, CT myelography, and diffusion tensor imaging (DTI) offer detailed visualization of both bony anatomy and neural pathways. Orthopedic surgeons often focus on the biomechanical implications seen in these images, assessing spinal stability and alignment, while neurosurgeons interpret neural compression and cord integrity to tailor decompression strategies.
Understanding the deliberate integration of these imaging techniques illuminated how treatment plans are customized. For example, a study published in the Journal of Neurosurgery: Spine highlights how combined radiological assessment guides decisions for minimally invasive versus open surgical approaches, ensuring patient-specific optimization.
This nuanced diagnostic interplay underscored the importance of seeking specialists who utilize comprehensive imaging protocols to craft personalized treatment pathways, rather than applying one-size-fits-all solutions.
Embracing Rehabilitation as an Integral Component of Spine Recovery and Long-Term Health
One of the most profound realizations during my recovery was the pivotal role of post-operative and conservative rehabilitation in restoring function and preventing recurrence. Both orthopedic and neurosurgical teams emphasize tailored physical therapy plans, but the nuances differ based on the surgical approach and individual patient goals.
My own rehabilitation journey involved a combination of core strengthening, flexibility exercises, and proprioceptive training, which were continuously adjusted by therapists in close communication with my surgical team. This dynamic, patient-centered rehab model is crucial for regaining mobility and minimizing complications such as adjacent segment disease.
For those interested in expert-backed rehab strategies, I found detailed protocols like the orthopedic lumbar fusion recovery tips invaluable for understanding the timeline and expectations of spine rehabilitation.
The Subtle Art of Surgeon-Patient Communication in Complex Spine Care Decisions
Beyond the technical expertise, the subtlety of effective communication profoundly shaped my treatment experience. Complex spine care involves high-stakes decisions where risk-benefit analyses can be daunting. Surgeons who demonstrated empathy, transparency, and willingness to engage in shared decision-making fostered a therapeutic alliance that reduced my anxiety and empowered me.
It became clear that evaluating a specialist’s interpersonal skills is as vital as assessing their clinical credentials. Observing how they addressed my concerns, explained uncertainties, and discussed alternative options helped me feel respected and informed.
If you’re navigating similar choices, I encourage you to explore resources such as this patient-focused guide on choosing a spine doctor to better understand how to evaluate these crucial communication factors.
Engaging in conversations here or sharing your experiences can deepen our collective understanding of the human side of spine care — your insights might illuminate paths for others facing these challenging decisions.
Things I Wish I Knew Earlier (or You Might Find Surprising)
The Subtle Power of Listening to Your Own Body
Early on, I underestimated how much my personal experience of pain and mobility mattered in guiding treatment choices. Specialists often rely on imaging and tests, but tuning in to how you feel day-to-day reveals nuances that no scan can capture. Trusting my instincts helped me advocate better for non-surgical options before jumping into more invasive treatments.
Not All Surgeries Are Created Equal
When surgery became an option, I learned that minimally invasive techniques can make a huge difference in recovery and long-term outcomes. Orthopedic surgeons and neurosurgeons alike are advancing these approaches, but not all surgeons offer them. Asking about surgical methods early changed my expectations and eased my fears.
The Emotional Weight of Choosing Your Surgeon
Decision-making wasn’t just clinical — it was deeply emotional. The spine is so central to our identity and independence that surrendering control feels scary. I wish I had known how crucial a surgeon’s empathy and communication style would be in helping me feel supported throughout the process.
Collaboration Beats Competition
I was surprised how often orthopedic surgeons and neurosurgeons collaborate rather than compete, especially on complicated cases. This teamwork ensures you get comprehensive care addressing both structure and nerves. It’s worth seeking specialists who prioritize this integrative approach rather than focusing solely on their own specialty.
Rehab Is Where the Real Healing Happens
Surgery or not, the rehabilitation phase proved to be where I truly reclaimed function. Customized physical therapy and ongoing adjustments made all the difference. I recommend not skipping on rehab and choosing providers who emphasize long-term recovery strategies, like those shared in orthopedic lumbar fusion recovery tips.
Don’t Underestimate the Value of a Second Opinion
Getting another perspective helped me clarify options and feel confident in my choices. Spine care is complex, and sometimes different specialists see things differently. If you feel uncertain, seeking a second or even third opinion can be empowering.
Resources I’ve Come to Trust Over Time
American Academy of Orthopaedic Surgeons (AAOS): Their patient-friendly guides, like on herniated discs, provided clear, evidence-based information that helped demystify spine care fundamentals. I often recommend their site for anyone starting the journey.
Choosing the Right Orthopedic Surgeon for Your Spine: This guide helped me understand what questions to ask and how to evaluate a surgeon’s approach beyond just credentials.
Minimally Invasive Back Pain Treatments Explained: The insights here on surgical and non-surgical options gave me hope for less disruptive therapies and shaped my conversations with doctors.
Effective Non-Surgical Care for Herniated Discs: I leaned heavily on this resource when exploring conservative treatments and it reinforced the value of patience and persistence with therapy.
How Orthopedic Nerve Blocks Help Manage Chronic Spine Pain: When flare-ups hit hard, understanding this pain management tool was a game changer in controlling symptoms without immediate surgery.
Parting Thoughts from My Perspective
Reflecting on my spine care journey, I realize that choosing between an orthopedic surgeon and a neurosurgeon isn’t just a medical decision — it’s a deeply personal one shaped by your unique condition, values, and goals. Both specialties bring invaluable expertise, but what truly matters is finding a provider who listens, communicates openly, and collaborates to tailor care just for you.
Don’t rush the process. Explore non-surgical options, ask about minimally invasive techniques, and consider rehabilitation as an integral part of healing. Embrace the emotional complexity of these choices and seek support when needed.
If this resonated with you, I’d love to hear your thoughts or experiences. Feel free to share in the comments below or reach out through contact. Your journey could be the beacon someone else needs.

I completely relate to the confusion the author felt when trying to decide whether to see an orthopedic surgeon or a neurosurgeon for spine issues. When my father was diagnosed with spinal stenosis, we had a tough time figuring out which specialist to consult. It wasn’t until we understood that orthopedic surgeons mainly treat structural problems like bones and joints while neurosurgeons focus on the nervous system that we started to feel more confident. What really helped was meeting doctors who emphasized collaborative care, especially for complex cases requiring both structural correction and nerve decompression. That multidisciplinary approach made all the difference in his recovery. Also, it’s interesting how minimally invasive techniques have evolved to bridge these specialties, reducing recovery times significantly. I wonder how many patients are aware of the importance of these advances when choosing their surgeon? Does anyone else feel that having transparent conversations about a surgeon’s experience with minimally invasive methods should become a standard part of initial consultations? It seems to me that empowering patients with this type of detailed information could alleviate much of the anxiety around surgical decisions. I’d be curious to hear how others approached these choices and managed to balance their hopes for recovery with the stress of decision-making.
Reading through the author’s detailed experience really resonated with me. As someone who also faced the daunting task of choosing between an orthopedic surgeon and a neurosurgeon, I found that understanding the specific nature of my condition made a huge difference. I had a herniated disc but also nerve impingement, which blurred the lines between the specialties. What helped me was seeking a multidisciplinary team approach, where both specialists collaborated to create a tailored treatment plan. This not only improved the surgical outcome but also made me feel more confident in the process.
I’m curious if others have had experience with such integrated care teams, especially in complex spine cases. Do you think hospitals should routinely offer combined consultations with both specialists before deciding on a surgical plan? I believe that transparent communication about a surgeon’s experience with minimally invasive techniques was vital in my decision, as recovery time was a significant concern. Perhaps standardizing such discussions could help reduce patient anxiety and improve satisfaction with the care process. Would love to hear more about how others navigated these complex choices and whether they found multidisciplinary approaches more reassuring.
This article shed light on the nuanced differences between orthopedic surgeons and neurosurgeons for spine care, which I think many patients overlook initially. I personally experienced a herniated disc that wasn’t resolving with conservative treatments. When I started exploring specialists, I realized that asking about their experience with minimally invasive techniques was crucial, especially since my priority was a quick recovery and less postoperative pain. It’s interesting how collaboration between the two disciplines can enhance outcomes, especially for complex cases. I wonder, though, how often patients are encouraged to seek multidisciplinary evaluations before deciding on surgery? In my experience, a comprehensive assessment that includes imaging, physical exams, and a clear discussion of treatment options really helps in making an informed choice. Have others found that early multi-specialty consultations helped them feel more confident and less anxious about the decision-making process? I believe that empowering patients with detailed information about their surgeon’s expertise can significantly improve their overall experience.