Understanding the Complexity of Shoulder Injuries and the Need for Specialized Care
Shoulder injuries represent a multifaceted challenge within orthopedic medicine, often demanding nuanced diagnosis and tailored treatment strategies. As an experienced orthopedic professional, I recognize that selecting the right shoulder injury specialist is pivotal to achieving optimal recovery outcomes. An expert with a deep understanding of shoulder biomechanics, advanced imaging modalities, and minimally invasive procedures can significantly influence the trajectory of healing.
The Critical Role of Subspecialization in Shoulder Orthopedics
Within the orthopedic domain, subspecialization—such as shoulder and sports medicine—offers distinct advantages. Specialists trained in these niches possess a refined skill set, encompassing the latest surgical techniques like arthroscopic repairs and rotator cuff reconstructions, supported by evidence-based protocols. For instance, a dedicated shoulder surgeon employed top-tier orthopedic spine specialists and shoulder experts ensures a comprehensive approach to complex cases.
Evaluating Experience and Niche Expertise in Shoulder Injury Management
Experience is a cornerstone of expert care. A specialist’s procedural volume, success rates, and ongoing participation in clinical research serve as key indicators of proficiency. Particularly, the management of acute injuries versus chronic degenerative conditions requires tailored expertise. For example, complex labral tears benefit from surgeons who have extensively performed arthroscopic repairs, leveraging cutting-edge techniques documented in peer-reviewed journals.
Integrating Advanced Diagnostic and Surgical Technologies
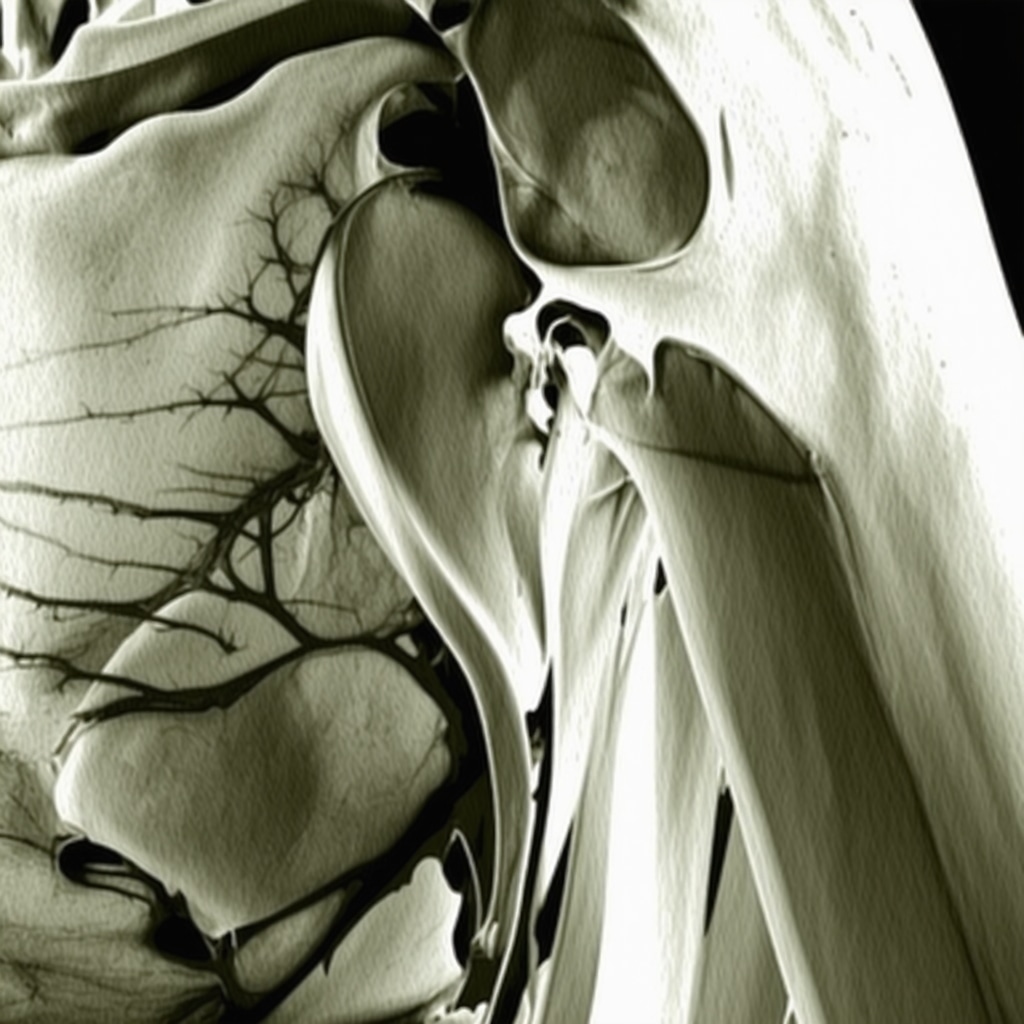
Modern shoulder specialists utilize state-of-the-art diagnostic tools such as 3D imaging, MRI arthrograms, and ultrasound-guided injections. These modalities enhance diagnostic accuracy, facilitate minimally invasive interventions, and reduce recovery times. An expert’s familiarity with these technologies translates into more precise treatment plans—crucial for athletes and active individuals aiming for swift return to function.
Questions to Ask When Selecting Your Shoulder Injury Expert
What specific training and experience do you have in shoulder arthroscopy and complex reconstructions?
Seeking detailed information about a surgeon’s subspecialty training, procedural volume, and outcomes provides insight into their expertise. Ensuring they maintain ongoing education and participate in clinical research further solidifies their authority in shoulder care.
Leveraging Trusted Resources and Building a Collaborative Care Network
Consulting reputable sources like the American Shoulder and Elbow Surgeons (ASES) or peer-reviewed publications can aid in identifying qualified specialists. Establishing a collaborative relationship with your healthcare team—integrating physical therapists, radiologists, and primary care—enhances treatment success.
For additional insights into selecting orthopedic specialists, explore this comprehensive guide. Your active participation in decision-making fosters trust and aligns your treatment with best practices.
Conclusion: Prioritizing Expertise for Effective Shoulder Recovery
The pathway to shoulder injury recovery is intricately linked to the expertise of your chosen specialist. Emphasizing subspecialty training, technological proficiency, and clinical experience ensures a strategic approach tailored to your unique injury profile—ultimately optimizing functional restoration and quality of life.
The Impact of Subspecialized Shoulder Care on Long-Term Outcomes
When considering shoulder injury treatment, the significance of subspecialized care cannot be overstated. Specialists trained specifically in shoulder and sports medicine are equipped with nuanced understanding of complex biomechanics, enabling them to tailor interventions that address both the injury and the patient’s activity goals. For instance, a surgeon with extensive experience in arthroscopic rotator cuff repairs not only improves surgical success rates but also reduces recovery time, facilitating quicker return to daily activities or sports.
How Do Cutting-Edge Diagnostic Technologies Enhance Shoulder Injury Management?
Modern diagnostic tools like 3D imaging, MRI arthrograms, and ultrasound-guided injections significantly improve accuracy in identifying injury specifics. These technologies allow for minimally invasive procedures, decreasing postoperative pain and speeding up rehabilitation. Mastery of these tools is often reflected in higher procedural success and better functional outcomes, especially for complex cases such as labral tears or multidirectional instability. To explore how these innovations translate into clinical practice, consider reviewing peer-reviewed research from reputable sources like the Journal of Shoulder and Elbow Surgery.
Can Your Shoulder Specialist Help You Avoid Surgery Through Non-Invasive Options?
Contrary to the common perception that surgery is inevitable for severe shoulder injuries, many cases benefit from advanced non-surgical treatments. Techniques such as platelet-rich plasma (PRP) injections, physical therapy, and targeted rehabilitation programs can often restore function without invasive procedures. An expert assessment that combines detailed imaging and functional testing can determine if your injury is amenable to these conservative approaches, which often result in shorter downtime and fewer risks. For more on effective non-surgical options, visit this resource.
What are the critical questions you should ask your shoulder specialist to ensure they are the right fit for your needs?
Asking about their specific training in advanced arthroscopic techniques, their success rates with similar injuries, and their approach to integrating new technologies can provide valuable insights. Additionally, inquire about their participation in ongoing research or clinical trials, which indicates a commitment to staying at the forefront of shoulder care. Building a collaborative relationship with your specialist, supported by transparent communication and shared decision-making, is essential for optimal outcomes.
To find a top-rated shoulder specialist near you, consult trusted sources like the Top Orthopedic Spine Specialists list. Remember, choosing a provider with proven expertise and cutting-edge technology access can significantly influence your recovery trajectory.
If you found this article insightful, please share your experiences or questions in the comments below. For personalized guidance, don’t hesitate to contact our team.
Innovative Diagnostic Modalities: Elevating Shoulder Injury Precision
In the realm of shoulder orthopedics, technological advancements continue to revolutionize diagnostic accuracy. Techniques like high-resolution 3D MRI reconstructions, dynamic ultrasound assessments, and intraoperative navigation systems provide clinicians with unparalleled insights into complex injuries such as multidirectional instability or subtle labral tears. These modalities not only facilitate precise injury localization but also enable tailored surgical planning, reducing the likelihood of revision procedures.
For instance, 3D MRI enhances visualization of soft tissue pathology, allowing surgeons to strategize minimally invasive repairs with confidence. Moreover, the integration of real-time intraoperative imaging assists in confirming the adequacy of repairs during arthroscopic procedures, ensuring optimal outcomes. As a result, patients benefit from shorter recovery times and improved functional restoration, particularly in high-demand athletes or labor-intensive workers.
Addressing Complex Cases: Multidisciplinary Approaches and Biomechanical Considerations
Managing intricate shoulder injuries often necessitates a multidisciplinary approach involving orthopedic surgeons, radiologists, physical therapists, and biomechanical engineers. Understanding the biomechanical forces at play, especially in cases of anterior dislocations compounded by rotator cuff or labral damage, guides the development of comprehensive treatment strategies. Advanced computational modeling can simulate post-repair joint mechanics, predicting stability and informing rehabilitation protocols.
Recent research published in the Journal of Orthopaedic Research highlights the importance of load-sharing strategies in post-surgical shoulder stability, emphasizing the role of custom-designed rehabilitation programs that account for individual biomechanics. Such integrated efforts ensure that surgical interventions align with functional demands, optimizing long-term joint health and performance.
What are the emerging roles of regenerative medicine in shoulder injury management?
Regenerative therapies, including platelet-rich plasma (PRP), stem cell injections, and bioengineered scaffolds, hold promise in accelerating tissue healing and reducing the need for extensive surgical repairs. Evidence from peer-reviewed studies indicates that when applied appropriately, these modalities can enhance the regenerative capacity of damaged tissues, especially in degenerative conditions or partial tears. Expert clinicians are now assessing the timing, dosage, and delivery methods of these biologics to maximize their efficacy.
Incorporating regenerative medicine into comprehensive treatment plans requires careful patient selection and coordination with advanced imaging to monitor healing progress. As ongoing clinical trials shed light on optimal protocols, practitioners equipped with this knowledge can offer innovative, less invasive options that align with patient preferences and recovery goals.
Future Directions: Personalized Shoulder Care Through Data-Driven Insights
The future of shoulder injury management lies in personalized medicine, leveraging big data analytics, machine learning algorithms, and wearable sensor technology. These tools enable continuous monitoring of joint function, biomechanics, and patient activity levels, providing real-time feedback to clinicians. Such data-driven insights facilitate early detection of potential setbacks, allowing for timely intervention before significant deterioration occurs.
Moreover, predictive analytics can identify patients at higher risk of re-injury or chronic instability, prompting preemptive measures such as tailored strengthening programs or biomechanical adjustments. The integration of these technologies promises to shift shoulder care from reactive to proactive, ultimately enhancing patient outcomes and quality of life.
If you are seeking a cutting-edge approach to shoulder injury diagnosis and treatment, consult with a specialist who employs these advanced modalities. Staying informed about emerging techniques ensures you receive care aligned with the latest scientific evidence and technological innovations.
< >
>
Harnessing Biomechanical Insights for Tailored Shoulder Rehabilitation
Understanding the intricate biomechanics of the shoulder joint is paramount for devising effective, individualized treatment plans. Advanced biomechanical modeling, utilizing dynamic motion analysis and force plate technology, allows clinicians to identify abnormal movement patterns and compensations that may hinder recovery or predispose to re-injury. Incorporating these insights into rehabilitation protocols ensures targeted strengthening and flexibility exercises, optimizing functional restoration.
The Significance of Multimodal Imaging in Complex Shoulder Pathology
Modern diagnostic approaches leverage a combination of imaging modalities such as high-resolution MRI, CT arthrography, and ultrasonography to capture a comprehensive picture of soft tissue, bony, and cartilaginous integrity. This multimodal strategy enhances diagnostic precision, especially in subtle or multifaceted injuries like multidirectional instability or partial rotator cuff tears. The integration of 3D reconstructions and real-time intraoperative imaging further refines surgical planning and execution.
What Role Do Biologics Play in Enhancing Shoulder Tissue Regeneration?
Biologic therapies, including platelet-rich plasma (PRP), stem cell injections, and bioengineered scaffolds, have emerged as promising adjuncts to accelerate healing and reduce the need for invasive procedures. Peer-reviewed studies demonstrate their potential in promoting angiogenesis, reducing inflammation, and stimulating tissue regeneration, particularly in degenerative conditions or partial-thickness tears. Expert application of these modalities requires precise timing, delivery techniques, and patient selection, emphasizing the importance of clinical expertise.
How Can Wearable Technologies Revolutionize Postoperative and Rehabilitation Monitoring?
Wearable sensors capable of tracking joint kinematics, muscle activity, and load distribution provide real-time data to clinicians, enabling adaptive and personalized rehabilitation strategies. Machine learning algorithms analyze this data to predict potential setbacks, such as improper movement patterns or overload, allowing preemptive interventions. The continuous feedback loop fosters patient engagement, adherence, and ultimately, superior functional outcomes.
Why Is a Multidisciplinary Approach Essential for Complex Shoulder Injuries?
Managing complex shoulder injuries often demands a collaborative effort among orthopedic surgeons, physical therapists, radiologists, sports scientists, and biomechanical engineers. This multidisciplinary synergy ensures comprehensive assessment, precise surgical intervention, and tailored rehabilitation. Computational modeling of postoperative biomechanics guides rehabilitation to restore optimal joint stability and prevent re-injury, especially in high-demand athletes or laborers.
What are the emerging frontiers of regenerative medicine in shoulder repair?
Innovations in regenerative medicine, such as bioengineered tissue scaffolds, gene therapy, and local delivery of growth factors, hold transformative potential. Ongoing clinical trials focus on optimizing these technologies to promote durable tissue regeneration, minimize surgical invasiveness, and enhance long-term joint health. As these modalities mature, they promise to redefine standard care, offering less invasive, biologically integrated solutions for shoulder injuries.
Stay ahead by consulting specialists who incorporate cutting-edge regenerative techniques, advanced imaging, and biomechanical analysis into their practice. Embracing these innovations can significantly improve your recovery trajectory and long-term shoulder health.
Expert Insights & Advanced Considerations
1. Embrace Multidisciplinary Collaboration
Integrating orthopedic surgeons, radiologists, physical therapists, and biomechanical engineers enhances diagnostic precision and treatment outcomes. A multidisciplinary approach ensures comprehensive care, especially in complex shoulder injuries that require nuanced interventions.
2. Leverage Cutting-Edge Diagnostic Technologies
Utilize advanced imaging modalities such as 3D MRI reconstructions and intraoperative navigation systems. These tools provide unparalleled insights, enabling minimally invasive procedures that reduce recovery times and improve functional results.
3. Prioritize Regenerative Medicine
Incorporate biologic therapies like PRP and stem cell injections to accelerate tissue healing. Evidence-based application of these modalities offers promising alternatives to traditional surgery, particularly in degenerative conditions or partial tears.
4. Utilize Data-Driven Personalized Care
Employ wearable sensors and machine learning algorithms to monitor joint biomechanics and activity levels. This approach facilitates early intervention, reduces re-injury risk, and tailors rehabilitation programs to individual needs.
5. Stay Informed on Emerging Frontiers
Follow peer-reviewed research and professional guidelines from authoritative sources such as the Journal of Shoulder and Elbow Surgery. Continuous education ensures adoption of innovative techniques that optimize patient outcomes.
Curated Expert Resources
- American Shoulder and Elbow Surgeons (ASES): A premier organization providing guidelines, research updates, and expert directories for shoulder specialists.
- Journal of Shoulder and Elbow Surgery: A peer-reviewed journal featuring cutting-edge research and clinical advancements in shoulder and elbow care.
- Orthopedic & Sports Physical Therapy Journals: Sources for evidence-based rehabilitation protocols and biomechanical insights.
- Advanced Imaging Technology Providers: Industry leaders offering the latest in MRI, ultrasound, and intraoperative navigation systems.
- Clinical Trials and Regenerative Medicine Forums: Platforms for staying current on innovative biologic treatments and their clinical applications.
Final Expert Perspective
In the realm of shoulder injury management, integrating multidisciplinary expertise with cutting-edge diagnostics and regenerative approaches represents the pinnacle of care. For those committed to excellence, continuous learning and collaboration are essential. If you’re a healthcare professional seeking to elevate your practice or a patient aiming for optimal recovery, engaging with authoritative resources and embracing innovation will position you at the forefront of shoulder care. Dive deeper into these topics and share your insights—your expertise can make a transformative difference in patient outcomes and clinical advancements. For personalized guidance or to connect with leading specialists, explore our contact page.


Reading through this comprehensive guide, I appreciate how much emphasis is placed on the importance of specialized knowledge and advanced technology in shoulder injury management. From my experience coaching athletes, I’ve often seen how timely, expert interventions utilizing cutting-edge diagnostics, like 3D MRI reconstruction, can make a noticeable difference in recovery speed and quality. It’s quite impressive how these innovations not only refine surgical precision but also minimize downtime, especially critical for high-performance individuals.
I’m curious about the practical steps patients can take to ensure their surgeons are well-versed in these advanced techniques. Do you recommend specific questions to ask during initial consultations or any particular credentials that indicate a surgeon’s proficiency in regenerative medicine or biomechanical modeling? Also, I wonder how these technological advances are being integrated into rehabilitation protocols—are physical therapists typically trained to work alongside surgeons in utilizing these diagnostics for personalized recovery plans? It seems like a multidisciplinary approach is essential for optimizing outcomes.
This article offers a solid overview of what to consider when choosing a shoulder specialist, emphasizing the importance of subspecialization, advanced diagnostics, and comprehensive care. From my experience working closely with orthopedic teams, I’ve seen firsthand how integrating technologies like 3D MRI reconstructions and intraoperative navigation can truly elevate surgical precision and outcomes. It’s also encouraging to see the focus on non-invasive options like PRP and targeted rehabilitation, which often help patients avoid or delay surgery altogether.
One thing I’d add is that patients should also consider the surgeon’s participation in ongoing research or clinical trials. This involvement often reflects a commitment to staying updated with the latest advancements. Additionally, asking about the surgeon’s collaborative approach with physiotherapists and radiologists can reveal how multidisciplinary the care will be—something I think is vital for complex cases.
In terms of rehabilitation, are there emerging training protocols for physical therapists to better utilize these technologies? I’d be interested to hear how integrated teams function in practice, especially for high-demand athletes or individuals with chronic shoulder issues.