Understanding the Complexity of Shoulder Injuries: An Expert’s Perspective
Shoulder injuries are among the most intricate musculoskeletal conditions, often involving multiple structures such as the rotator cuff tendons, labrum, and acromioclavicular joint. As an orthopedic specialist, I recognize that effective recovery hinges on a nuanced understanding of injury mechanisms, biomechanical factors, and patient-specific variables. Recent advances in imaging modalities like MRI and ultrasound have enhanced diagnostic precision, enabling tailored treatment plans that optimize outcomes.
Biopsychosocial Factors Influencing Shoulder Injury Rehabilitation
The recovery process is not solely about addressing structural damage. Psychological resilience, patient adherence, and social support play pivotal roles. For example, a patient’s motivation significantly impacts physiotherapy engagement, which in turn influences healing trajectories. An interdisciplinary approach integrating physical therapy, pain management, and psychological support is often necessary for complex cases.
Innovative Non-Surgical Interventions: Beyond Conventional Therapy
Emerging modalities such as platelet-rich plasma (PRP) injections and low-level laser therapy have shown promise in accelerating tissue regeneration. Moreover, minimally invasive arthroscopic procedures now allow for precise debridement and repair with reduced recovery time. For instance, a recent study in the Journal of Shoulder and Elbow Surgery highlights improved outcomes with biologic treatments combined with structured rehabilitation.
Addressing Chronic Shoulder Pain: When to Consider Advanced Interventions
Chronic shoulder pain persisting beyond six months warrants a comprehensive re-evaluation. Arthroscopic interventions, such as subacromial decompression or rotator cuff repair, are considered when conservative measures fail. Furthermore, emerging evidence suggests that regenerative medicine techniques may delay or obviate the need for surgery in select patients, especially those with partial-thickness tears or tendinopathies.
What Are the Latest Advances in Shoulder Injury Management That Can Improve Patient Outcomes?
Recent developments in biologic therapies, such as stem cell injections, are pushing the boundaries of shoulder injury treatment. These approaches aim to harness the body’s innate healing potential, offering hope for faster recovery and reduced reliance on traditional surgical methods.
For optimal recovery, I recommend patients consult with a multidisciplinary team that includes orthopedic surgeons, physiotherapists, and pain specialists. If you’re interested in exploring advanced treatment options or need a comprehensive assessment, consider visiting our contact page.
To deepen your understanding of spine-related orthopedic concerns, you can explore top spine specialists for 2025.
Revolutionizing Shoulder Injury Management: What Are the Latest Biologic Breakthroughs?
In recent years, the field of orthopedic medicine has witnessed a paradigm shift with the advent of biologic therapies, particularly in the treatment of shoulder injuries. These innovations leverage the body’s natural healing mechanisms to promote tissue regeneration, reduce recovery times, and potentially delay or eliminate the need for surgical intervention. For example, stem cell injections and platelet-rich plasma (PRP) therapies have gained widespread attention for their promising results in managing rotator cuff tendinopathies and partial tears.
How Do These Cutting-Edge Treatments Challenge Traditional Approaches and What Are Their Practical Implications?
Traditionally, persistent shoulder injuries required invasive surgeries such as arthroscopic repairs or decompression procedures, which often involve lengthy rehabilitation. Now, with biologic therapies, patients can explore minimally invasive options that aim to stimulate the body’s intrinsic repair processes. According to a recent review in the Journal of Shoulder and Elbow Surgery, biologic treatments combined with structured physical therapy can significantly improve healing times and functional outcomes, especially in early-stage tendinopathies and partial tears.
Furthermore, these therapies open new avenues for personalized medicine. By analyzing patient-specific factors such as age, tissue quality, and injury chronicity, orthopedic specialists can tailor biologic interventions for maximum efficacy. This approach aligns with the broader trend in orthopedics towards less invasive, more patient-centered care, improving overall satisfaction and long-term outcomes.
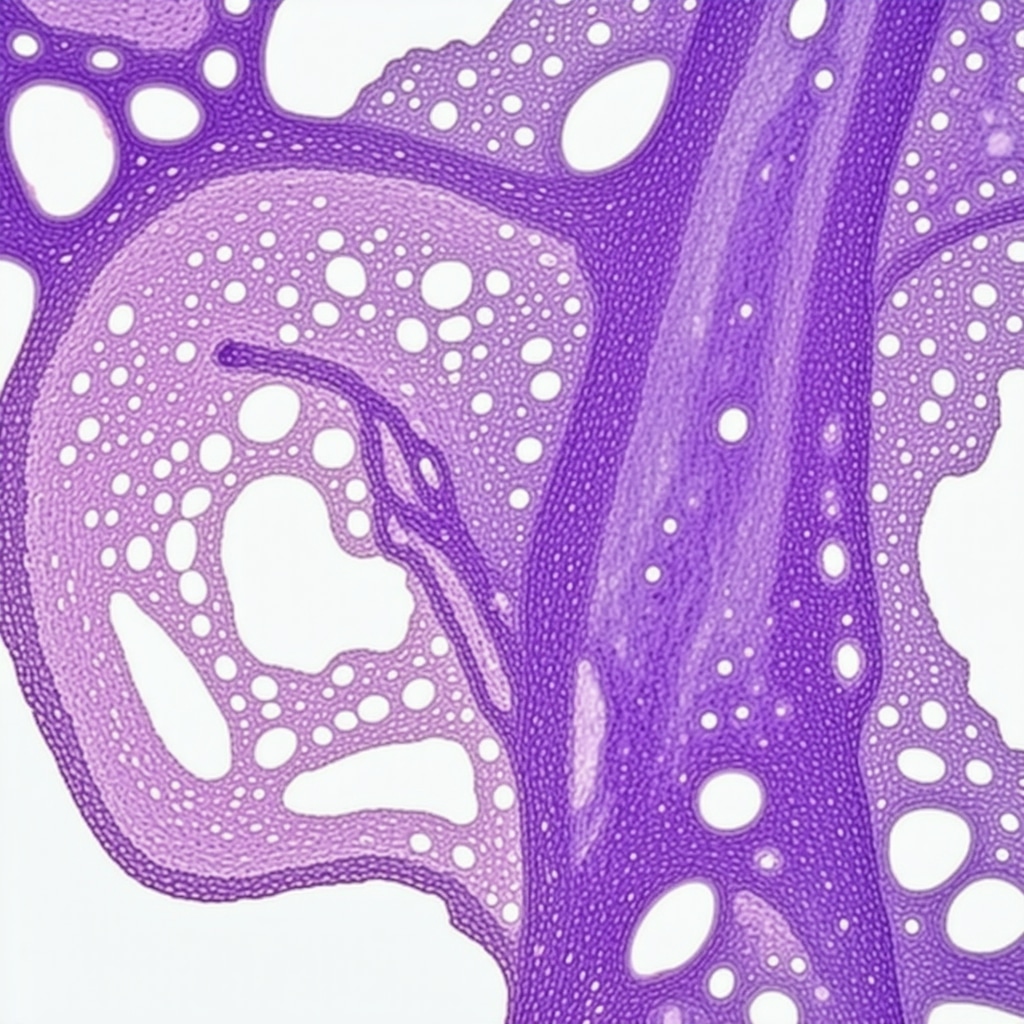
The Role of Advanced Imaging and Biomarkers in Optimizing Biologic Therapies
To ensure precise application of these novel treatments, advanced imaging techniques like high-resolution MRI and ultrasound are indispensable. They enable clinicians to assess tissue quality, monitor healing progress, and adjust treatment plans accordingly. Moreover, emerging research emphasizes the potential of biomarkers—biochemical indicators of tissue repair—to predict treatment responsiveness and guide therapy customization.
For patients considering biologic options, consulting with a multidisciplinary team that includes orthopedic surgeons, radiologists, and regenerative medicine specialists can be highly beneficial. If you’re interested in exploring these advanced treatment modalities, visit our contact page for a comprehensive assessment.
To deepen your understanding of how integrative approaches enhance shoulder injury recovery, check out our guide on non-surgical care options that complement biologic therapies.
Harnessing the Power of Regenerative Medicine: The Future of Shoulder Injury Treatment
As orthopedic medicine continues to evolve, regenerative therapies such as stem cell injections and platelet-rich plasma (PRP) are transforming the landscape of shoulder injury management. These biologic approaches aim to stimulate intrinsic healing mechanisms, offering patients less invasive options with promising outcomes. Recent research in high-impact journals like Stem Cells Translational Medicine highlights the potential for these treatments to not only accelerate recovery but also improve the quality of tissue repair, especially in complex or chronic cases.
Precision Medicine Meets Biologics: Tailoring Treatment to Individual Needs
One of the most exciting developments in this field is the move toward personalized regenerative strategies. Factors such as patient age, tissue health, injury chronicity, and genetic markers influence the effectiveness of biologic therapies. Advanced diagnostic tools, including high-resolution MRI and specific biomarkers, enable clinicians to customize interventions with greater accuracy. This personalized approach maximizes therapeutic efficacy and reduces unnecessary procedures, aligning with the broader shift toward precision medicine in orthopedics.
Addressing the Nuanced Challenges of Regenerative Therapies
Despite their promise, biologic treatments are not without challenges. Variability in preparation protocols, the quality of biologic products, and patient-specific biological responses can affect outcomes. For example, the concentration and activation methods of platelet-rich plasma can differ significantly between clinics, impacting healing potential. Moreover, understanding the long-term effects of stem cell therapies requires ongoing research, as current data is often limited to short-term follow-ups. Experts emphasize the importance of standardized protocols and rigorous clinical trials to validate these approaches and optimize their application.
What are the key factors influencing the success of biologic therapies in shoulder injury recovery?
Factors include the timing of intervention, injury type and severity, patient biological response, and the quality of biologic preparation. Early application in acute or subacute phases often yields better results, whereas chronic degenerative conditions may require adjunctive therapies or combined approaches. Additionally, integrating biologics with physical therapy and biomechanical optimization enhances overall healing and functional restoration.
For those interested in cutting-edge treatments, collaborating with multidisciplinary teams that include orthopedic surgeons, radiologists, and regenerative medicine specialists is crucial. Exploring these options through comprehensive assessment can significantly improve your recovery trajectory. If you’re eager to learn more or consider personalized biologic treatments, visit our contact page.
The Role of Advanced Imaging and Biomarkers in Optimizing Regenerative Strategies
Implementing biologic therapies effectively depends on precise diagnostics. Advanced imaging modalities like 3T MRI and ultrasound provide detailed insights into tissue quality, tear size, and inflammation. Additionally, emerging research on biomarkers—biochemical indicators of tissue repair—offers the potential to predict treatment responsiveness and tailor interventions dynamically. For instance, elevated levels of specific cytokines may signal a favorable environment for biologic augmentation, guiding clinicians to optimize timing and choice of therapy.
Incorporating these diagnostic tools into clinical practice requires a nuanced understanding of tissue pathology and healing pathways. As research progresses, integrating biomarker profiling with imaging data will become standard practice, enhancing personalized care and improving long-term outcomes.
If you’re considering regenerative options for your shoulder injury, consulting with specialists experienced in these advanced diagnostics and therapies is essential. Discover more about how integrative, personalized approaches can elevate your recovery by visiting our comprehensive care guide.
Exploring the Nuanced Mechanisms Behind Biologic Regeneration in Shoulder Repair
Recent advancements in biologic therapies have unveiled complex cellular and molecular pathways that facilitate tissue regeneration in shoulder injuries. Stem cell injections, for instance, leverage mesenchymal stem cells’ ability to differentiate into various tissues, promoting intrinsic healing processes. These therapies modulate inflammatory responses, enhance angiogenesis, and stimulate extracellular matrix production, fundamentally altering traditional treatment paradigms. Understanding these mechanisms allows clinicians to optimize therapeutic timing and select suitable candidates for biologic interventions.
Multidisciplinary Approaches: Integrating Biologics, Biomechanics, and Rehabilitation Science
Successful shoulder injury management increasingly depends on a holistic, multidisciplinary approach. Integrating biologic treatments with biomechanical correction—such as optimizing joint kinematics and muscular balance—amplifies healing potential. Cutting-edge rehabilitation protocols now incorporate neuromuscular electrical stimulation, proprioceptive training, and biofeedback techniques, which synergistically enhance biologic tissue repair. This convergence fosters a personalized recovery pathway, minimizing downtime and maximizing functional restoration.
Which Advanced Diagnostic Tools Are Critical for Personalizing Shoulder Regenerative Therapies?
Accurate diagnostics are essential for tailoring biologic treatments. High-resolution MRI and ultrasound provide detailed assessments of tissue integrity, tear morphology, and inflammatory status, informing precise intervention strategies. Moreover, emerging biomarker profiling—such as cytokine levels and tissue-specific genetic markers—offers predictive insights into treatment responsiveness. For example, elevated levels of vascular endothelial growth factor (VEGF) may indicate a conducive environment for angiogenic therapies, guiding clinicians toward specific biologic modalities.
Harnessing the Power of Precision Medicine: Customizing Regenerative Protocols
Personalized medicine now underpins biologic therapies, allowing treatments to be adapted to individual patient profiles. Factors such as age-related tissue degeneration, genetic predispositions, and injury chronicity influence therapeutic efficacy. Advanced computational models and machine learning algorithms analyze multi-modal data—imaging, biomarkers, patient history—to optimize treatment plans. This precision approach significantly improves outcomes, reduces adverse effects, and fosters long-term joint health.
Future Directions: Integrating Regenerative Medicine with Emerging Technologies
The future of shoulder injury management lies in the integration of biologics with emerging technologies like 3D bioprinting, nanomedicine, and gene editing. 3D bioprinting enables the creation of customized scaffolds infused with biologic agents, facilitating targeted tissue regeneration. Nanoparticle delivery systems enhance the localization and potency of biologics while minimizing systemic exposure. Gene editing tools, such as CRISPR-Cas9, hold promise for correcting genetic defects that impair healing, paving the way for truly personalized regenerative therapies.
How Will These Innovations Shape the Next Decade of Shoulder Injury Treatment?
As these technologies mature, we anticipate a shift toward fully integrated, minimally invasive regenerative platforms capable of restoring shoulder function with unprecedented precision. These approaches will likely reduce the need for traditional surgeries, shorten recovery times, and improve quality of life for patients with complex or chronic injuries. Engaging with ongoing clinical trials and research initiatives remains essential for clinicians and patients eager to embrace these transformative advancements.
Stay ahead in orthopedic innovation—consult with specialists knowledgeable in regenerative medicine and emerging technologies to explore personalized treatment options that align with your recovery goals. Visit our contact page for comprehensive assessments and tailored care plans.
Expert Insights & Advanced Considerations
Innovative Biologic Treatments Are Transforming Outcomes
Leading orthopedic specialists emphasize that biologic therapies like stem cell injections and platelet-rich plasma (PRP) are revolutionizing shoulder injury management by harnessing the body’s innate healing mechanisms, resulting in accelerated recovery times and reduced surgical interventions.
Personalized Medicine Is Now Central to Treatment Success
Advanced diagnostics, including high-resolution MRI and biomarker profiling, enable clinicians to tailor regenerative therapies to individual patient profiles, optimizing efficacy and minimizing unnecessary procedures.
Integration of Multidisciplinary Approaches Enhances Outcomes
Combining biologic treatments with biomechanical correction, targeted rehabilitation, and advanced imaging results in comprehensive care pathways that significantly improve long-term shoulder function and patient satisfaction.
Emerging Technologies Will Shape the Future of Shoulder Care
Innovations such as 3D bioprinting, nanomedicine, and gene editing are poised to further refine regenerative strategies, potentially reducing the need for invasive surgeries and enabling truly personalized treatment plans.
Key Factors for Success in Regenerative Shoulder Therapies
Optimal timing, injury assessment, patient biological response, and treatment standardization are critical for maximizing outcomes. Ongoing research and clinical trials continue to refine these protocols for better patient care.
Curated Expert Resources
- Journal of Shoulder and Elbow Surgery: Offers peer-reviewed research on biologic treatments and regenerative medicine advancements in shoulder injury management.
- Stem Cells Translational Medicine: Provides cutting-edge studies on stem cell applications and tissue engineering for musculoskeletal repair.
- National Institutes of Health (NIH) Regenerative Medicine Resources: Contains comprehensive information on emerging therapies, clinical trials, and future directions in regenerative orthopedics.
Final Expert Perspective
In the realm of shoulder injury management, embracing innovative biologic therapies and personalized regenerative approaches elevates patient outcomes by combining cutting-edge science with clinical expertise. As these treatments evolve, collaboration among multidisciplinary teams becomes essential to harness their full potential. For practitioners and patients eager to explore these advanced options, engaging with specialized centers and staying informed through reputable sources ensures access to the most effective, evidence-based care. To deepen your understanding or inquire about tailored treatment plans, visit our contact page.


This article provides a comprehensive overview of the latest approaches in shoulder injury management, especially the focus on biologic therapies like PRP and stem cell injections. I’ve personally seen how these treatments can significantly reduce recovery times when combined with targeted physical therapy. What I find particularly interesting is the emphasis on personalized medicine—tailoring treatments based on imaging and biomarkers. In my experience, early intervention with these innovative therapies offers the best results, but I wonder how accessible these advanced diagnostics and biologics are for patients in smaller clinics or rural areas. Do you think the future of shoulder care will become more decentralized as techniques become more standardized? It’s exciting to see how these emerging technologies could democratize access to high-quality orthopedic treatments, making them more available to a broader range of patients.