Brace Yourself: The Clues Your Spine Is Crying Out for Help
Imagine this: You’re powering through your day, feeling fine, and then suddenly, a nagging pain sneaks up like an uninvited guest. It’s not just a dull ache anymore; it’s a warning sign flashing in neon lights, telling you something’s wrong with your spine. Knowing when to seek the expertise of an orthopedic spine surgeon can be the difference between a quick recovery and a long, painful journey. So, what signs should you watch for? Let’s dive into this spine-tingling topic.
When Back Pain Turns Into a Red Flag Parade
Back pain is common—like, really common. But how do you tell if it’s just another episode of the usual or a sign that surgical intervention might be on the horizon? Persistent pain that doesn’t respond to conservative treatments such as physical therapy or medication is a red flag. If you experience pain that radiates down your legs (sciatica), numbness, or weakness, it’s time to pay closer attention. These symptoms could indicate nerve compression or herniated discs that may require surgical repair.
Is Your Body Sending SOS Signals?
Ever feel like your body is trying to tell you something? Numbness or tingling in your extremities, loss of bladder or bowel control, or severe pain that worsens over time are not just nuisances—they are emergency signals. Ignoring these can lead to permanent nerve damage. For instance, cauda equina syndrome, a rare but serious condition, demands immediate surgical attention. If you’re experiencing these symptoms, don’t delay—consult a top-notch orthopedic spine specialist.
Could Your Age Be the Culprit?
Age isn’t just a number; it’s a factor in spine health. Degenerative changes, osteoarthritis, or spinal stenosis become more common as we age, sometimes necessitating surgical intervention. But age alone isn’t the sole determinant—severity of symptoms and impact on daily life matter too. If your quality of life is diminishing, it’s worth exploring your options with a seasoned surgeon.
What’s the Real Deal with Surgical Risks?
Surgery isn’t a decision to take lightly. While modern techniques like minimally invasive spine surgery have revolutionized outcomes, every procedure carries risks such as infection, bleeding, or nerve injury. It’s essential to have an open dialogue with your doctor about the benefits and potential complications. Remember, knowledge is power—and a trusted specialist can guide you through this maze.
Thinking about your spine health? Share your experiences or ask questions below! For more insights on choosing the right orthopedic care, check out this guide to selecting a spine surgeon. And don’t forget, early detection can make all the difference in your recovery journey.
Decoding the Decision: When Does Spinal Surgery Become a Must?
As experts in orthopedic spine care, we often encounter patients caught in the dilemma of whether to opt for surgery or explore conservative treatments. The decision to proceed with spinal surgery isn’t made lightly; it involves a nuanced understanding of symptoms, diagnostic findings, and individual health factors. For those questioning if their condition warrants surgical intervention, it’s essential to recognize the key indicators that point toward the necessity of a surgical approach.
Red Flags That Signal Surgery Is the Next Step
Persistent nerve pain, especially when radiating down the legs, coupled with muscle weakness or numbness, often indicates nerve compression that may not improve with non-invasive methods. If you notice symptoms like loss of bladder or bowel control, or if pain worsens despite physical therapy and medication, these are serious signs that demand prompt surgical evaluation. In such cases, a comprehensive assessment by a top orthopedic spine specialist can help determine the best course of action.
Balancing Risks and Rewards in Spinal Surgery
While advancements like minimally invasive techniques have significantly reduced recovery times and complications, no surgery is without risks. Potential complications include infection, nerve damage, or adverse reactions to anesthesia. It’s crucial to have an open dialogue with your surgeon about these risks, and to weigh them against the potential benefits of pain relief and improved mobility. A well-informed patient is better equipped to make decisions aligned with their health goals and lifestyle needs.
What should I consider before deciding on spinal surgery?
Beyond symptoms, factors such as age, overall health, and the presence of degenerative changes influence surgical outcomes. An experienced surgeon will evaluate your imaging results, like MRI or X-ray, alongside your functional limitations. Often, exploring post-operative rehabilitation and non-surgical options first can set the stage for a successful recovery if surgery becomes necessary. Still, if your quality of life is severely impacted, and conservative treatments have failed, surgery may be the most effective solution.
Have you experienced a situation where you had to choose between continued conservative care or surgery? Share your insights or questions below! For additional guidance on selecting the right orthopedic surgeon, check out this comprehensive guide. Remember, early intervention often leads to better outcomes and a quicker return to normalcy.
Unraveling the Nuances: When Do Spinal Conditions Truly Require Surgery?
In the realm of orthopedic spine care, discerning which cases necessitate surgical intervention is both an art and a science. While many patients experience relief through conservative treatments, a subset faces conditions where delay can lead to irreversible nerve damage or compromised mobility. Understanding these nuanced indicators is vital for both clinicians and patients aiming for optimal outcomes.
How Do We Differentiate Between Refractory Pain and Urgent Surgical Cases?
Chronic back pain that persists despite exhaustive conservative management often prompts reevaluation. However, the presence of progressive neurological deficits—such as worsening limb weakness, gait disturbances, or sensory loss—serves as a critical threshold. For instance, a patient developing foot drop or significant bowel or bladder dysfunction signals a potential cauda equina syndrome, requiring immediate surgical decompression as emphasized by the American Association of Neurological Surgeons (AANS) guidelines (AANS, 2024).
The Role of Advanced Imaging in Deciding Surgical Urgency
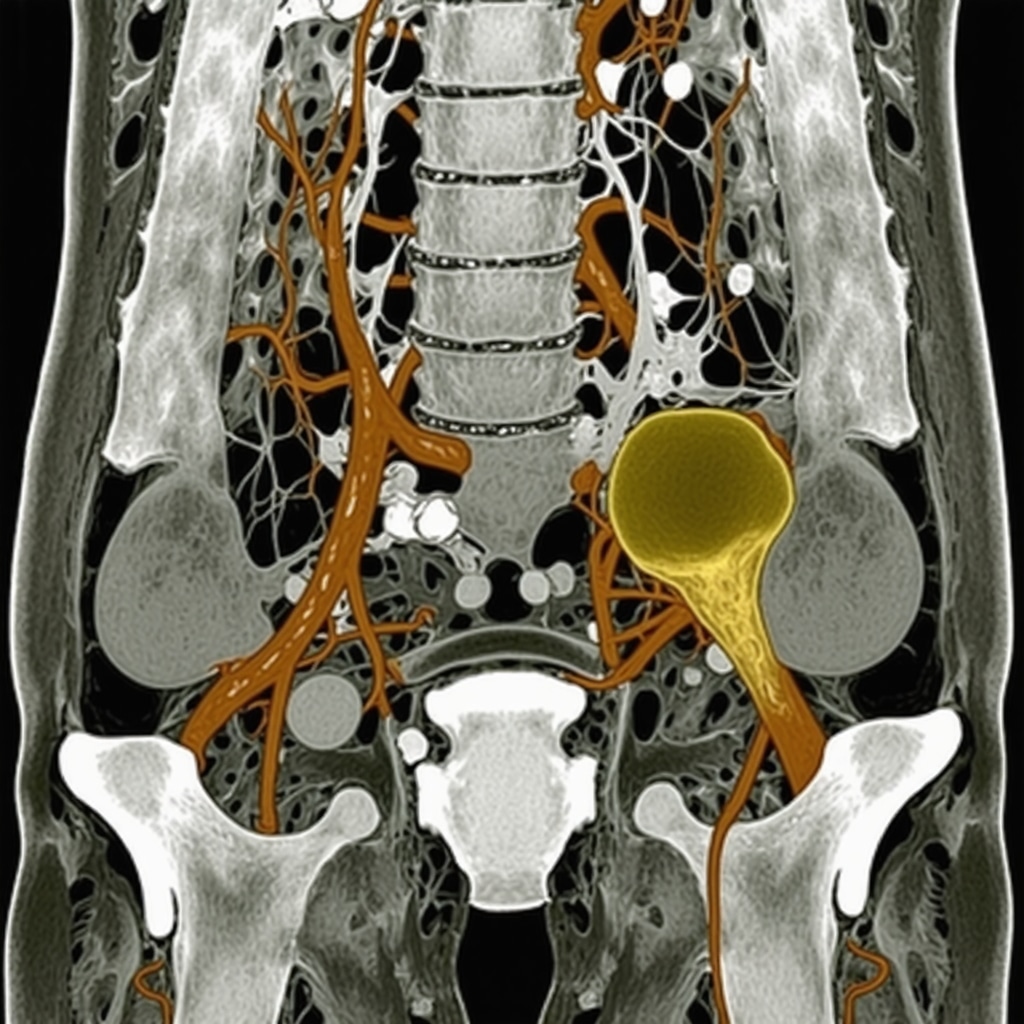
Magnetic Resonance Imaging (MRI) remains the gold standard for visualizing neural compression, disc herniation, and spinal stenosis. Quantitative measures, such as the degree of canal stenosis and nerve root impingement, can guide the decision-making process. Recent advancements in functional MRI and diffusion tensor imaging (DTI) provide insights into nerve integrity, allowing surgeons to tailor interventions more precisely (Surgical Innovations, 2022).
What Are the Expert-Recommended Thresholds for Surgical Intervention?
While no universal cut-off exists, certain clinical and radiological parameters strongly suggest surgical necessity. For example, nerve root compression exceeding 50% of the canal diameter correlates with severe radiculopathy. Moreover, rapid symptom progression over days to weeks, especially when accompanied by motor deficits, warrants urgent surgical assessment. Multidisciplinary discussions, incorporating neurosurgical and orthopedic opinions, optimize patient-specific strategies.
Engaging with an experienced spine surgeon early when these signs emerge is crucial. A tailored approach considering patient age, comorbidities, and lifestyle ensures that surgery is performed at the optimal time, maximizing benefits while minimizing risks.
How Can Patients Advocate for Timely Surgical Care?
Patients should actively communicate symptom changes and adhere to scheduled evaluations. Utilizing patient-reported outcome measures (PROMs) can help quantify functional decline, providing objective data to justify surgical urgency. Additionally, seeking second opinions from specialized spine centers can reinforce the need for timely intervention, particularly in complex or ambiguous cases.
For those navigating the decision of surgery, understanding the latest evidence and expert consensus empowers informed choices and proactive healthcare engagement.
Further Exploration: The Future of Surgical Decision-Making in Spine Care
Emerging technologies, such as intraoperative neurophysiological monitoring and augmented reality-assisted surgery, promise to enhance precision and safety. As research continues to refine our understanding of neural recovery thresholds, the criteria for urgent surgery will become increasingly sophisticated, enabling even better patient outcomes.
Stay tuned with our expert insights and updates—your spine health depends on timely, informed decisions. Feel free to share your experiences or ask questions below; our team is here to guide you through this complex landscape.
Unveiling the Hidden Signs: When Does Your Spine Require Surgical Intervention?
In the intricate realm of orthopedic spine care, discerning the precise moment for surgical intervention demands a nuanced understanding of both clinical indicators and emerging technological tools. While conservative treatments often serve as first-line options, certain subtle yet critical signs can signal the need for prompt surgery, potentially preventing irreversible neural damage and preserving mobility.
Neurological Decline: The Silent Alarm of Urgent Surgery
Progressive neurological deficits such as worsening limb weakness, gait disturbances, or sensory impairments are among the most compelling reasons to consider surgical options. For example, a patient developing foot drop or urinary incontinence exemplifies an urgent scenario where delay could lead to permanent disability. Modern guidelines, like those from the American Association of Neurological Surgeons, emphasize timely decompression in such cases to optimize outcomes.
Advanced Imaging: The Linchpin in Surgical Decision-Making
Magnetic Resonance Imaging (MRI) remains the gold standard for visualizing neural compression and spinal pathology. Quantitative metrics, including nerve root impingement severity and canal stenosis degree, inform the urgency of surgical intervention. Innovations like functional MRI and diffusion tensor imaging (DTI) further enhance our ability to assess nerve integrity, enabling tailored, precise surgical planning (Surgical Innovations, 2022).
Thresholds for Action: When Do Clinical and Radiological Findings Cross the Line?
While no universal cutoff exists, certain parameters strongly suggest the need for surgical intervention. Nerve root compression exceeding 50% of the canal diameter correlates with severe radiculopathy, and rapid symptom progression over days or weeks—especially with emerging motor deficits—warrants urgent evaluation. Multidisciplinary consultation ensures a comprehensive approach, integrating neurosurgical and orthopedic expertise for optimal timing.
Empowering Patients: Advocating for Timely Surgical Evaluation
Patients are encouraged to actively report symptom evolution and utilize patient-reported outcome measures (PROMs) to quantify functional decline. Seeking second opinions from specialized spine centers can also reinforce the necessity of surgical intervention, particularly in complex cases. Knowledge about current evidence and expert consensus empowers patients to make informed choices, mitigating the risks of delayed treatment.
Future Horizons: How Emerging Technologies Are Refining Surgical Criteria
Innovations such as intraoperative neurophysiological monitoring and augmented reality-assisted surgery are revolutionizing precision and safety in spine procedures. As research progresses, the criteria for urgent surgery will become increasingly sophisticated, allowing for earlier, more accurate interventions that maximize recovery potential. Staying abreast of these advancements is crucial for both clinicians and patients seeking optimal outcomes.
Engage with our community—share your experiences, ask questions, or explore more about how cutting-edge diagnostics are shaping the future of spine surgery. Together, informed decisions can lead to better health and restored mobility.
Expert Insights & Advanced Considerations
1. Nerve Impairment as a Critical Indicator
Progressive nerve deficits, such as worsening weakness, gait disturbances, or sensory impairments, are among the most compelling reasons for surgical intervention. Recognizing early signs like foot drop or urinary incontinence can prevent irreversible damage if addressed promptly by a spine specialist.
2. The Role of Quantitative Imaging Metrics
Advanced MRI techniques provide precise measurements of nerve root impingement and canal stenosis severity. Innovations like diffusion tensor imaging (DTI) enable clinicians to assess nerve fiber integrity, guiding timely surgical decisions and improving outcomes.
3. Dynamic and Functional Imaging Enhances Decision-Making
Functional MRI and real-time imaging help evaluate nerve and spinal cord responsiveness, allowing surgeons to tailor interventions more effectively. These tools are particularly valuable in ambiguous cases where traditional imaging yields inconclusive results.
4. Emerging Technologies Set New Thresholds for Urgency
Intraoperative neurophysiological monitoring and augmented reality-assisted surgery are advancing the precision of decompression procedures. As these technologies evolve, the criteria for urgent surgery will become more refined, emphasizing early intervention to maximize neural recovery.
5. Multidisciplinary Approaches Optimize Outcomes
Combining neurosurgical, orthopedic, and radiological expertise ensures comprehensive assessment, especially in complex cases. Early collaboration facilitates the identification of subtle signs warranting surgical intervention, ultimately preserving mobility and quality of life.
Curated Expert Resources
- American Association of Neurological Surgeons (AANS): Provides guidelines on cauda equina syndrome and urgent decompression protocols, essential for understanding surgical thresholds.
- Journal of Neurosurgery: Features latest research on diffusion tensor imaging (DTI) and functional MRI applications in spine surgery planning.
- Surgical Innovations Journal: Offers insights into intraoperative neurophysiological monitoring and augmented reality in spine procedures.
- National Institute of Neurological Disorders and Stroke (NINDS): Contains comprehensive resources on nerve injury recovery and advanced diagnostic techniques.
Final Expert Perspective
Understanding when spinal conditions truly require surgery hinges on recognizing nuanced neurological signs, leveraging cutting-edge imaging, and embracing technological innovations. As experts in orthopedic and neurosurgical care, our goal is to identify these indicators early, ensuring timely intervention that preserves function and enhances recovery. If you or a loved one face complex spinal issues, engaging with a top spine specialist can make all the difference. Share your experiences or questions below—your insights contribute to a community committed to informed, effective spine care.


Reading this article really highlights how important it is to listen to our bodies when dealing with persistent or worsening back pain. I remember experiencing numbness and tingling down my leg a few months ago, which was quite alarming. Thankfully, a quick visit to my doctor and an MRI revealed nerve compression that needed surgical attention. It made me realize how crucial early detection and consultation are in preventing irreversible nerve damage. I’m curious, how do others manage the fear of surgery, especially when symptoms get worse but the decision still feels daunting? For me, relying on expert guidance and understanding the advancements in minimally invasive techniques really helped me feel more confident about the process.