Unlocking the Secrets of Slipped Disc Treatment: What Orthopedic Experts Recommend
Slipped discs, medically known as herniated discs, can disrupt everyday life with persistent pain, limited mobility, and nerve-related symptoms. Orthopedic doctors bring a wealth of experience and cutting-edge techniques to the table, blending conservative care with advanced interventions to restore function and comfort. Understanding their best practices not only empowers patients but also fosters more effective recovery journeys.
Innovative Non-Surgical Approaches That Orthopedic Specialists Trust
Before considering surgery, orthopedic specialists often emphasize non-invasive treatments tailored to the individual’s condition. Physical therapy focused on strengthening core muscles and improving spinal flexibility is a cornerstone. Techniques such as targeted exercises, traction therapy, and ergonomic adjustments can alleviate pressure on the affected nerve roots. Additionally, advanced pain management strategies—like corticosteroid injections—offer temporary relief that facilitates participation in rehabilitation.
These methods align closely with recommendations from the American Academy of Orthopaedic Surgeons, which highlights the importance of personalized, conservative care before surgical options are explored (AAOS).
When Surgery Becomes Necessary: Orthopedic Criteria and Techniques
Orthopedic surgeons carefully evaluate when operative treatment is warranted—typically when symptoms persist beyond 6 weeks despite conservative care, or when neurological deficits worsen. Minimally invasive procedures like microdiscectomy are preferred to reduce tissue damage and speed recovery. Surgeons employ high-definition imaging and precision tools to excise the herniated portion of the disc while preserving spinal integrity.
How Do Orthopedic Doctors Determine the Best Treatment Path for a Slipped Disc?
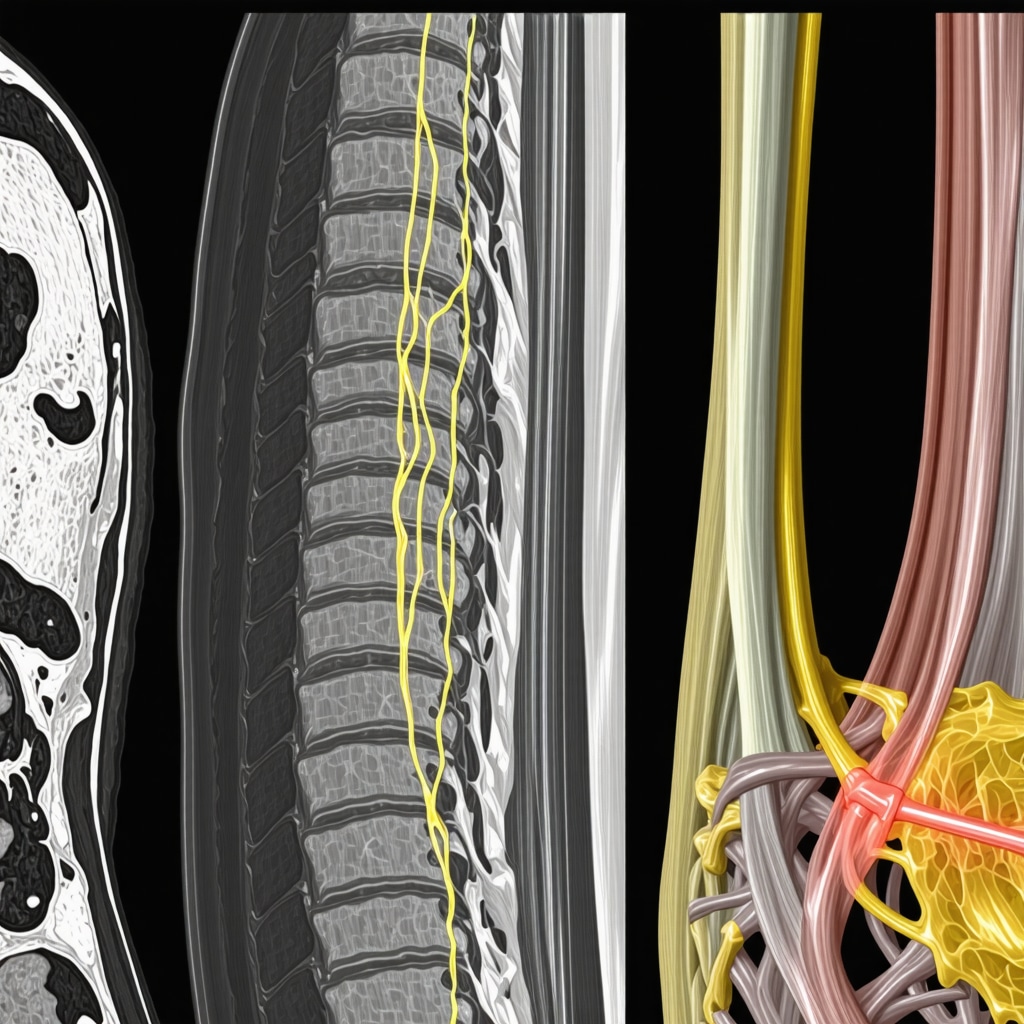
Deciding on a treatment plan involves a nuanced assessment of symptom severity, imaging results, and patient lifestyle. Orthopedic doctors integrate MRI findings with clinical evaluation, considering factors such as the extent of nerve compression and muscle weakness. Shared decision-making is key—doctors discuss risks, benefits, and expected outcomes with patients to tailor a plan that balances efficacy and quality of life.
Rehabilitation and Long-Term Care: Orthopedic Insights for Sustained Recovery
Post-treatment rehabilitation is pivotal. Orthopedic experts recommend structured physical therapy programs emphasizing gradual reintroduction of activity and core stabilization. Patient education on posture, ergonomics, and lifestyle modifications reduces recurrence risks. Moreover, ongoing monitoring through follow-up consultations ensures that recovery progresses optimally and complications are promptly addressed.
For those interested in detailed rehabilitation strategies after spine procedures, resources like orthopedic rehab tips after lumbar fusion surgery provide invaluable guidance.
Facing a slipped disc challenge? Share your experiences or questions below to engage with experts and fellow patients navigating this journey.
Listening to Your Body: Early Signs and Preventive Measures
From my own experience and countless stories shared by others, one lesson stands out clearly: paying attention to early warning signs can make a world of difference. I remember when I first noticed a dull ache in my lower back after a long day of work. Rather than dismissing it, I decided to take a step back and adjust my daily habits. Simple changes like improving my sitting posture and incorporating gentle stretching helped me avoid worsening symptoms. Orthopedic specialists often emphasize this proactive approach, encouraging patients to recognize subtle discomfort before it escalates into a slipped disc or herniation requiring intensive treatment.
What daily habits can you adopt to protect your spine from disc problems?
Reflecting on this question helped me embrace small yet effective lifestyle adjustments. Ergonomic seating, regular breaks to stand and move, and mindful lifting techniques are not just buzzwords—they’re practical tools that support spinal health. If you’re curious, exploring back pain treatment options and orthopedic approaches can offer you detailed insights tailored to your needs.
Integrating Orthopedic Expertise with Holistic Wellness
While orthopedic interventions focus on the mechanical aspects of slipped discs, integrating holistic wellness can accelerate recovery and improve overall quality of life. During my recovery, I found that combining physical therapy with mindfulness practices helped manage the stress and frustration that often accompany chronic pain. According to a study published by the National Institutes of Health, mindfulness-based stress reduction programs can effectively reduce pain perception and improve function in patients with chronic back pain (NIH Study on Mindfulness and Back Pain).
This blend of conventional orthopedic care and complementary therapies highlights a more comprehensive path to healing. If you’re interested in exploring this balance further, resources like effective non-surgical care for herniated discs can provide a wealth of information.
Real-Life Stories: How People Overcame Their Slipped Disc Challenges
Hearing from others who have navigated slipped disc issues is incredibly inspiring. One friend shared how targeted physical therapy and patience helped her avoid surgery altogether. Another colleague’s journey involved minimally invasive surgery followed by dedicated rehabilitation, which restored his active lifestyle. These personal narratives remind me that while medical expertise guides the way, individual commitment and resilience are equally vital.
Have you faced similar challenges or found unique strategies that worked for your slipped disc recovery? I’d love to hear your story—drop a comment below or share this article with someone who might benefit from these insights.
Precision Diagnostics: Leveraging Cutting-Edge Imaging and Biomarkers in Slipped Disc Evaluation
Beyond conventional MRI and CT scans, orthopedic experts are increasingly utilizing advanced imaging modalities to gain a more nuanced understanding of slipped disc pathology. Diffusion tensor imaging (DTI) and functional MRI (fMRI) provide insights into nerve fiber integrity and inflammation, which can critically inform prognosis and treatment customization. Additionally, emerging research into biochemical markers in serum and cerebrospinal fluid holds promise for quantifying disc degeneration and inflammatory status, potentially enabling earlier detection and monitoring of therapeutic response.
These sophisticated diagnostic tools are reshaping patient assessment paradigms, allowing orthopedic specialists to tailor interventions with unprecedented precision and potentially reduce unnecessary surgeries. Integration of artificial intelligence algorithms further enhances image interpretation accuracy, helping identify subtle changes that might escape traditional evaluation.
What role do advanced imaging techniques play in predicting treatment outcomes for slipped discs?
Advanced imaging, such as diffusion tensor imaging, offers valuable prognostic information by revealing the extent of nerve root involvement and microstructural damage. This data assists orthopedic clinicians in stratifying patients who may benefit from conservative care versus those requiring surgical intervention. Studies published in the Journal of Orthopaedic Research demonstrate that preoperative DTI metrics correlate strongly with postoperative functional recovery, enhancing shared decision-making quality.
Personalized Orthopedic Care: Integrating Patient-Specific Biomechanics and Lifestyle Factors
Recognizing that no two slipped disc cases are identical, modern orthopedic management increasingly emphasizes personalized biomechanical assessments. Using dynamic motion analysis and wearable sensor data, clinicians can evaluate how individual movement patterns and spinal loading contribute to disc pathology. This data-driven approach enables crafting highly individualized rehabilitation programs that address not only anatomical deficits but also functional behaviors perpetuating symptoms.
Moreover, patient lifestyle, occupational demands, and psychosocial factors are meticulously incorporated into treatment planning. Multidisciplinary collaboration involving physiatrists, pain specialists, and psychologists ensures comprehensive care addressing the biopsychosocial nature of slipped disc disorders. Such integration improves adherence to therapy and optimizes long-term outcomes.
Emerging Therapeutic Innovations: Biologic Treatments and Regenerative Medicine in Orthopedics
Orthopedic research is actively exploring biologic therapies aimed at promoting disc regeneration and modulating inflammation. Platelet-rich plasma (PRP) injections and mesenchymal stem cell therapies have shown preliminary efficacy in reducing pain and enhancing disc matrix repair. Although still considered investigational, these modalities represent a paradigm shift from purely symptomatic relief to disease modification.
Clinical trials published in Stem Cells Translational Medicine highlight promising safety profiles and functional improvements, warranting further investigation. Orthopedic specialists are cautiously optimistic, advocating for patient selection criteria refinement and standardized protocols to maximize therapeutic benefit while minimizing risks.
Curious about cutting-edge diagnostics or regenerative options for slipped disc care? Connect with our orthopedic experts to explore personalized strategies tailored to your unique condition.
Harnessing AI-Powered Diagnostics to Revolutionize Slipped Disc Evaluation
In recent years, the integration of artificial intelligence (AI) into orthopedic diagnostics has dramatically enhanced the precision of slipped disc assessments. Machine learning algorithms analyze complex imaging datasets—such as high-resolution MRIs and diffusion tensor imaging—to identify subtle patterns of nerve impingement and disc degeneration that might elude even seasoned clinicians. This technological leap not only expedites diagnosis but also refines prognostic accuracy, enabling more personalized and timely interventions.
Furthermore, AI-driven predictive models synthesize patient demographics, biomechanical data, and clinical history to forecast recovery trajectories, supporting shared decision-making processes and optimizing resource allocation in clinical settings.
Incorporating Psychosocial Dynamics: The Hidden Dimension in Orthopedic Care
Orthopedic specialists increasingly recognize the profound influence of psychosocial factors—such as stress, anxiety, and patient expectations—on slipped disc outcomes. Cognitive-behavioral therapy (CBT) and pain neuroscience education are being integrated alongside physical treatments to address these dimensions. This multi-modal approach mitigates chronic pain amplification and enhances patient engagement in rehabilitation.
By embracing a biopsychosocial model, clinicians can tailor interventions that transcend mechanical correction, fostering holistic resilience and sustained functional improvement.
What are the latest evidence-based protocols for integrating regenerative medicine with traditional orthopedic care in slipped disc treatment?
Emerging protocols advocate for a synergistic combination of regenerative biologics—such as mesenchymal stem cells and platelet-rich plasma—with established surgical and conservative therapies. Recent clinical trials, including those summarized in Stem Cells Translational Medicine, suggest that timing of biologic administration post-decompression surgery can potentiate disc matrix restoration and attenuate inflammatory cascades.
Moreover, patient stratification based on molecular biomarkers and biomechanical profiling enhances treatment responsiveness. Multidisciplinary teams orchestrate these complex protocols, ensuring safety and maximizing functional recovery.
Advancing Postoperative Rehabilitation: Integrating Neuroplasticity and Functional Movement Retraining
Cutting-edge rehabilitation paradigms emphasize neuroplasticity to remodel maladaptive pain pathways and restore motor control. Techniques such as graded motor imagery, sensorimotor retraining, and virtual reality-assisted exercises complement conventional physical therapy to expedite recovery and reduce recurrence risk.
Orthopedic experts advocate for dynamic feedback mechanisms through wearable technology, enabling real-time adjustments and patient empowerment during rehabilitation.
Ready to explore these advanced orthopedic insights and innovate your slipped disc recovery? Connect with our specialists to develop a personalized, state-of-the-art treatment plan tailored to your unique needs.

Frequently Asked Questions (FAQ)
What are the earliest symptoms of a slipped disc that I should watch out for?
Early signs often include localized back pain, tingling, or numbness in limbs, and occasional muscle weakness. These subtle symptoms can precede more severe nerve compression, so prompt evaluation by an orthopedic specialist is recommended to prevent progression.
How effective are non-surgical treatments compared to surgery for slipped discs?
Non-surgical approaches, including physical therapy, pain management, and lifestyle modifications, successfully alleviate symptoms in approximately 80-90% of patients. Surgery is generally reserved for cases with persistent pain beyond 6 weeks or neurological deficits. An individualized approach ensures optimal outcomes.
What advanced imaging techniques provide better insights than standard MRI?
Diffusion tensor imaging (DTI) and functional MRI (fMRI) reveal microstructural nerve damage and inflammation not visible on standard MRI, aiding prognosis and treatment planning. AI-enhanced image analysis further increases diagnostic precision, allowing tailored interventions.
Can regenerative therapies like stem cells or PRP replace traditional treatments?
Regenerative medicine is promising as a complementary strategy to promote disc repair and reduce inflammation. However, these therapies are currently investigational and best used alongside conventional care within clinical trials or specialized centers under expert guidance.
How do psychosocial factors affect slipped disc recovery?
Stress, anxiety, and patient expectations significantly influence pain perception and rehabilitation adherence. Incorporating cognitive-behavioral therapy and pain education enhances recovery by addressing these psychosocial dimensions alongside physical treatment.
What role does personalized biomechanical assessment play in treatment?
Assessing individual movement patterns and spinal loading via dynamic analysis and wearable sensors enables customized rehabilitation programs that target specific functional deficits, improving efficacy and reducing recurrence risk.
How important is postoperative rehabilitation and what does it involve?
Postoperative rehabilitation is critical, focusing on gradual activity resumption, core stabilization, and neuroplasticity-based retraining techniques. Integrating technology such as virtual reality and real-time feedback optimizes motor control recovery and long-term spine health.
Are there risks associated with minimally invasive surgeries like microdiscectomy?
While minimally invasive surgeries reduce tissue damage and recovery time, risks include infection, nerve injury, and recurrence of herniation. Experienced orthopedic surgeons employ advanced imaging and techniques to minimize these risks and maximize safety.
How can I prevent future slipped discs after recovery?
Maintaining ergonomic posture, engaging in regular spinal-strengthening exercises, avoiding heavy lifting with improper technique, and managing body weight are key preventive measures. Ongoing education and lifestyle adjustment are essential for sustained spine health.
When should I seek a second opinion regarding my slipped disc diagnosis or treatment?
If symptoms persist despite treatment, if surgery is recommended prematurely, or if you desire more clarity on options, consulting another orthopedic expert can provide additional perspectives and ensure the best personalized care plan.
Trusted External Sources
- American Academy of Orthopaedic Surgeons (AAOS) – Offers evidence-based guidelines and patient education on slipped disc management and orthopedic best practices (aaos.org).
- National Institutes of Health (NIH) – National Center for Complementary and Integrative Health – Provides research data on mindfulness and integrative therapies relevant to back pain and orthopedic recovery (PMC3679190).
- Journal of Orthopaedic Research – Publishes peer-reviewed studies on advanced imaging techniques and orthopedic treatment outcomes (pubmed.ncbi.nlm.nih.gov/31077167/).
- Stem Cells Translational Medicine – Features clinical trial reports on regenerative therapies such as stem cells and PRP for orthopedic applications (PMC6945676).
- Orthopaedic Research Society (ORS) – A leading organization providing updates on biomechanics, regenerative medicine, and innovations in orthopedic care (ors.org).
Conclusion
Slipped disc treatment is a dynamic field where orthopedic expertise combines traditional methods with emerging technologies to optimize patient outcomes. From early detection and conservative management to advanced diagnostics and regenerative medicine, personalized care tailored to individual biomechanics and psychosocial contexts is paramount. Integrating rehabilitation strategies that leverage neuroplasticity and functional retraining further enhances recovery and prevents recurrence.
Empowering patients with knowledge about their condition and involving them actively in shared decision-making ensures treatments align with their lifestyle and goals. As orthopedic research progresses, cutting-edge diagnostics and biologic therapies hold promise for transforming slipped disc care into a more precise and holistic discipline.
If you found these insights valuable, please share this article, leave your questions or experiences in the comments, and explore our related expert content to deepen your understanding and support your journey to spinal health.


I really appreciate the comprehensive insights shared about slipped disc treatment in this article. One aspect that struck me was the emphasis on personalized, conservative care before jumping to surgery. In my own experience with a herniated disc, engaging in a structured physical therapy program focused on core strengthening and posture correction made a noticeable difference in managing pain and preventing further damage. It’s interesting how advanced imaging techniques like diffusion tensor imaging (DTI) can provide deeper understanding beyond standard MRIs—this probably explains why some patients respond better to conservative treatments while others need surgical intervention. The integration of AI and wearable sensor data in tailoring rehab approaches sounds very promising for enhancing recovery precision. I also found the mention of psychosocial factors particularly relevant; dealing with the emotional toll of chronic pain shouldn’t be overlooked, and combining therapies like cognitive-behavioral therapy with physical rehab could be a game-changer. For those who have undergone treatment for slipped discs, I’d love to hear if integrating mindfulness or other holistic practices alongside traditional orthopedic care has improved your outcomes or helped with pain management? It seems like blending these approaches offers a more rounded recovery process.
Diana, I really resonate with your point about the importance of combining cognitive-behavioral therapy (CBT) and mindfulness with physical rehabilitation for managing slipped disc pain. From my own experience, while physical therapy addressed the mechanical pain and improved my posture, it was the mindfulness practices that helped me cope with the chronic discomfort and anxiety associated with recovery. This holistic approach made the rehabilitation process less daunting and more sustainable. I also find the advancements in AI-driven personalized rehab fascinating—being able to track real-time progress and adjust exercises feels like a significant step forward in patient-centered care. On the topic of early prevention, I’ve found that consistent daily habits, like ergonomic workstation setups and regular micro-breaks, have been invaluable in reducing flare-ups. However, navigating the emotional toll of chronic pain is often less talked about but equally crucial. Have others found specific mindfulness techniques or mental health strategies particularly effective alongside traditional orthopedic treatments? I’m curious to learn what has genuinely helped people maintain both their physical and emotional well-being during recovery.
This article offers a thorough overview of the current best practices in treating slipped discs and emphasizes the importance of personalized care. I particularly appreciated the focus on conservative treatments like targeted physical therapy and ergonomic adjustments before considering surgery. From my own experience dealing with a herniated disc, I found that incorporating core strengthening exercises and maintaining good posture significantly alleviated my symptoms. What I find intriguing is the expanding role of advanced imaging techniques such as diffusion tensor imaging (DTI). These tools could potentially help us better understand nerve involvement and tailor treatments more precisely, possibly even predicting which patients might recover with conservative care versus those who may need surgical interventions. I wonder how widespread the adoption of such technology is in everyday clinical practice. Also, integrating psychosocial factors like stress management and mindfulness seems to be gaining traction. Has anyone here experienced improvement by combining physical rehab with mental health strategies? It seems that addressing both the physical and emotional aspects of recovery could lead to more sustainable outcomes.
I appreciate how this article highlights the importance of combining conservative care with advanced techniques in treating slipped discs. From my own journey, I found that early intervention played a crucial role. I’d experienced nagging back discomfort but delayed seeking professional advice, which led to worsening symptoms and eventual diagnosis of a herniated disc. What struck me was how orthopedic doctors tailor non-surgical options, like individualized physical therapy and ergonomic adjustments, before considering surgery. The role of corticosteroid injections as a bridge to rehabilitation was something I hadn’t known about before. Moreover, the emphasis on shared decision-making resonates deeply; understanding the risks and benefits helped me feel empowered in my care choices.
Another important aspect I discovered is the value of patient education on posture and lifestyle modifications as preventive measures, which truly made a difference in sustaining my recovery and reducing flare-ups. The integration of emerging diagnostic technologies, such as diffusion tensor imaging and AI-powered assessments, seems promising for more precise treatment plans.
Has anyone else struggled to maintain motivation with long-term rehabilitation exercises? I’ve heard wearable sensor feedback helps some stay engaged—what are your experiences with such tech in managing slipped disc recovery?
Clara, I can definitely relate to your concerns about maintaining motivation during long-term rehabilitation. From my own recovery journey after a microdiscectomy, I found that incorporating wearable sensor feedback made a significant difference. Having real-time data on my posture and movement gave me tangible goals and helped me stay accountable. It was encouraging to see measurable progress, which kept my spirits up during the tougher days. That said, I also realized that motivation can wane, especially when progress seems slow. In these moments, having a supportive rehab team and setting small, achievable milestones was crucial. On the topic of wearable technology, I’m curious how others have integrated these tools alongside more traditional approaches like therapist-led sessions or mindfulness practices? Has anyone experienced challenges balancing tech reliance with personalized care? Also, given how the article highlights personalized biomechanics in treatment, I wonder how deeply rehab programs are tailoring exercises based not just on clinical findings but also patient lifestyle, work environment, and stress levels. Has anyone felt their therapy truly adapted to these factors, making recovery more holistic and sustainable? It would be great to hear diverse experiences or tips, especially around navigating the balance between advanced tech and human-centered care.
Reading through this comprehensive article really highlights how personalized and multi-faceted slipped disc treatment has become. I’ve experienced mild disc issues before, and what resonated with me was the emphasis on early recognition and lifestyle modifications—simple habits like proper lifting techniques and regular movement can make a big difference. I find the integration of advanced diagnostic tools like diffusion tensor imaging (DTI) fascinating because it helps tailor treatment plans more accurately. From my perspective, the role of patient education cannot be overstated; understanding how everyday activities influence spinal health encourages proactive behavior. I’m curious, though—has anyone found that combining traditional physical therapy with mindfulness or relaxation techniques has helped manage not only pain but also the emotional stress associated with recovery? Sometimes, the psychological aspect can be just as challenging as the physical, and holistic approaches seem promising. It would be great to hear how others are incorporating these complementary strategies into their recovery journey to foster resilience and improve outcomes.
Building on the discussion about non-surgical treatments and advanced diagnostics, I’ve noticed that patient education on lifestyle and ergonomic adjustments often gets less attention than it deserves. From my personal experience, early recognition of discomfort and proactive changes, such as investing in a proper ergonomic chair and integrating stretching breaks into daily routines, significantly eased my symptoms before any formal therapy began. The article’s mention of integrating psychosocial aspects like mindfulness strikes a chord; managing stress seemed to reduce my perception of pain alongside physical therapy.
Another point I find fascinating is the role of personalized biomechanics in treatment planning. It seems that when rehab programs consider not just the clinical imaging but also an individual’s daily movement patterns and work habits, patients may experience more sustainable recovery. I’m curious—have others found that rehab tailored to their specific lifestyle needs led to better adherence or prevented recurrence? Also, the emerging use of neuroplasticity techniques and wearable technology seems promising, but I wonder how accessible these advanced tools are outside specialized centers. Has anyone had experience with such innovations in their recovery journey? It would be great to hear thoughts on balancing cutting-edge tech with practical, everyday management strategies.