Advanced Understanding of Spondylolisthesis and Its Therapeutic Challenges
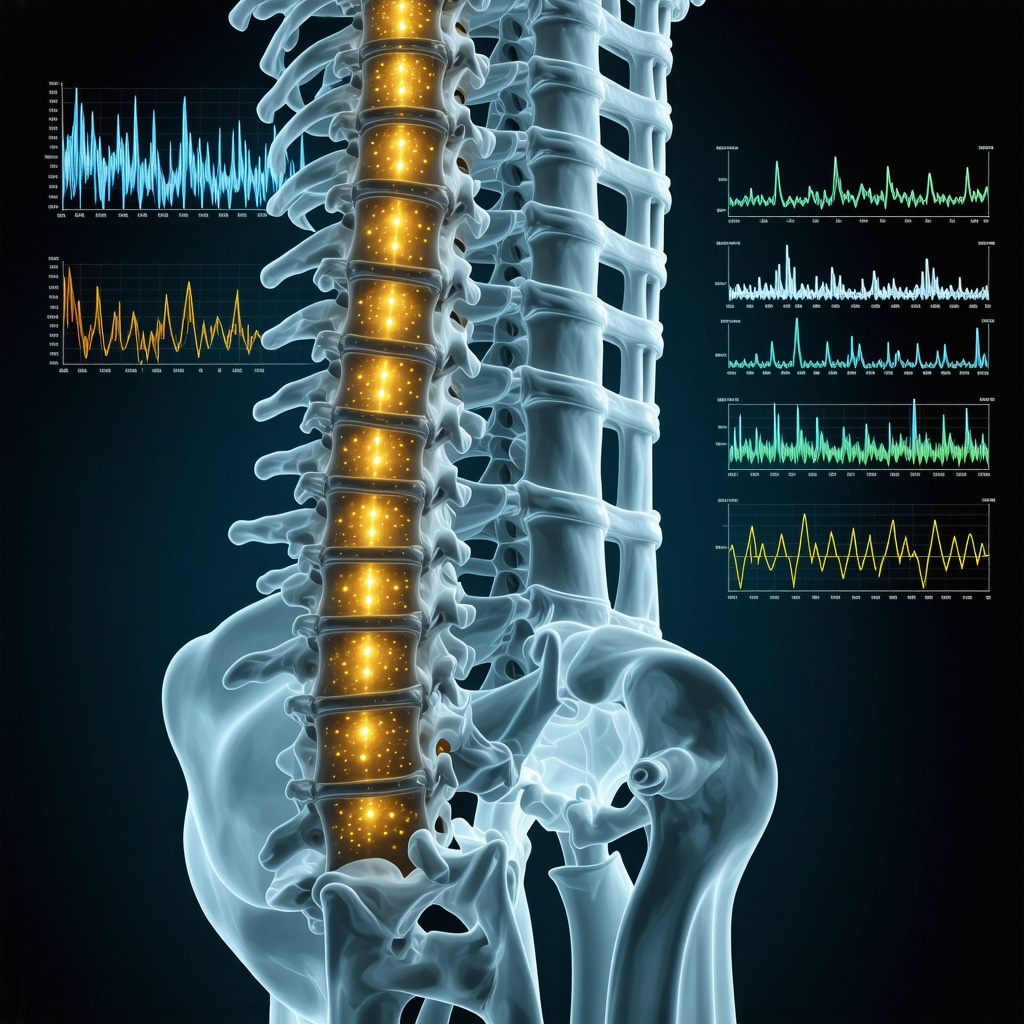
Spondylolisthesis, characterized by the anterior displacement of a vertebra relative to the one beneath it, presents a nuanced challenge to orthopedic specialists. Effective treatment requires an intricate balance of biomechanical insight, patient-specific factors, and evolving therapeutic modalities. As an orthopedic expert, it is critical to evaluate not only the grade of vertebral slippage but also the symptomatic profile, neurological involvement, and overall spinal stability before determining the optimal intervention strategy.
Multimodal Treatment Paradigms Rooted in Biomechanical Precision
Contemporary management of spondylolisthesis extends beyond conventional pain mitigation. Orthopedic protocols now emphasize a multimodal approach incorporating precise physical rehabilitation, pharmacologic adjuncts, and, when indicated, surgical innovation. Non-surgical interventions often include tailored core stabilization exercises to enhance segmental spinal support and reduce dynamic instability, coupled with orthopedic bracing to offload stress on vulnerable vertebral segments. This conservative approach aligns with findings from peer-reviewed clinical studies on spinal stability.
When Does Surgical Intervention Become Imperative in Spondylolisthesis?
Determining the threshold for surgery demands an expert appraisal of progressive neurological deficits, intractable pain refractory to conservative care, and substantial mechanical instability. Minimally invasive spine surgery techniques have revolutionized the therapeutic landscape, reducing perioperative morbidity and accelerating recovery times. Techniques such as transforaminal lumbar interbody fusion (TLIF) or posterior lumbar interbody fusion (PLIF) are preferred for their biomechanical efficacy in restoring vertebral alignment and neural decompression.
How Do Orthopedic Experts Customize Treatment Plans Based on Spondylolisthesis Type and Patient Profile?
Orthopedic specialists differentiate treatment strategies by spondylolisthesis etiology—whether isthmic, degenerative, traumatic, or dysplastic. Patient age, activity level, comorbidities, and spinal morphology critically influence therapeutic decisions. For instance, younger patients with isthmic spondylolisthesis may benefit from aggressive rehabilitation and selective surgical fusion, whereas older adults with degenerative forms might prioritize conservative care to maintain function. These tailored approaches underscore the necessity for comprehensive orthopedic evaluation, such as outlined in specialized spondylolisthesis treatment plans.
Integrating Emerging Technologies and Non-Invasive Modalities in Treatment
Emerging non-invasive options, including advanced spinal decompression therapy and regenerative medicine applications, are progressively integrated into orthopedic care frameworks to complement established treatments. These modalities aim to enhance tissue healing and modulate pain pathways without surgical risks. Expert practitioners continuously evaluate the evidence base for these technologies to optimize patient-centered outcomes.
For a deeper dive into minimally invasive back pain treatments and recovery strategies, explore this expert resource and consider consulting with top orthopedic spine specialists recommended here.
Are you an orthopedic professional with insights or case studies on spondylolisthesis treatment? Join the conversation to advance expert knowledge and improve patient care outcomes.
Optimizing Rehabilitation: The Role of Neuromuscular Re-education in Spondylolisthesis Recovery
Neuromuscular re-education has emerged as a pivotal component in post-treatment rehabilitation for spondylolisthesis patients. This technique focuses on retraining the central nervous system to improve muscle coordination and spinal stability, particularly after surgical interventions such as lumbar fusion. By enhancing proprioception and motor control, neuromuscular re-education mitigates compensatory movement patterns that may otherwise exacerbate vertebral instability. Incorporating this strategy into rehabilitation protocols aligns with advancements highlighted in physiotherapy research, underscoring its efficacy in optimizing functional outcomes for spinal disorders.
Exploring Biomechanical Innovations: How 3D Modeling Enhances Surgical Planning
Orthopedic surgeons now leverage sophisticated 3D biomechanical modeling to simulate vertebral displacement and predict post-surgical spinal dynamics. This technological innovation enables precise customization of surgical approaches based on individual patient anatomy and spondylolisthesis severity. By visualizing stress distributions and potential fusion outcomes preoperatively, surgeons can minimize intraoperative risks and enhance the durability of corrective procedures. Such advancements contribute to the growing body of evidence supporting personalized medicine in orthopedic spine care.
Addressing Comorbidities: Integrating Osteoporosis Management with Spondylolisthesis Treatment
Given the frequent coexistence of osteoporosis in patients with degenerative spondylolisthesis, comprehensive care must include strategies to improve bone quality before and after surgical intervention. Pharmacologic agents such as bisphosphonates and anabolic therapies can bolster vertebral strength, reducing the risk of hardware failure and adjacent segment disease post-fusion. Orthopedic specialists advocate for routine bone density assessment and coordinated management with endocrinologists to optimize surgical outcomes and long-term spinal health.
What Are the Emerging Biomarkers and Imaging Techniques That Could Revolutionize Early Detection and Monitoring of Spondylolisthesis Progression?
Current research is investigating biochemical markers of cartilage degradation and inflammation alongside advanced imaging modalities like dynamic MRI and quantitative CT to identify early micro-instability and predict slippage progression. These innovations promise to refine diagnostic precision and inform timely intervention. Staying abreast of these developments is crucial for orthopedic experts aiming to integrate cutting-edge diagnostics into clinical practice.
For those interested in advancing their understanding of non-surgical treatment alternatives and comprehensive care models, reviewing the latest expert recommendations can be highly beneficial.
Engage with our professional community by sharing your experiences or case studies related to spondylolisthesis management. Your insights are invaluable in shaping future standards of care.
Harnessing Artificial Intelligence for Predictive Analytics in Spondylolisthesis Prognosis
Artificial Intelligence (AI) is rapidly transforming orthopedic diagnostics and treatment planning, particularly in the realm of spondylolisthesis. Machine learning algorithms trained on large datasets of imaging and clinical parameters can predict disease progression, surgical outcomes, and individualized rehabilitation responses with remarkable accuracy. This predictive capability enables clinicians to stratify patients based on risk profiles, tailoring interventions preemptively to optimize long-term spinal stability and function. Integrating AI into clinical workflows demands rigorous validation and multidisciplinary collaboration, ensuring models are both clinically relevant and ethically sound.
Biomechanical Engineering Advances: Customized Implants and Load Distribution Optimization
Recent progress in biomechanical engineering has yielded patient-specific spinal implants fabricated via additive manufacturing (3D printing). These implants are designed to match the unique vertebral morphology and biomechanical environment of each patient, enhancing fusion rates and reducing adjacent segment degeneration. Finite element analysis (FEA) simulations guide implant design by modeling load distribution and stress shielding effects, thereby mitigating complications related to implant failure or subsidence. Such innovations exemplify the convergence of engineering and orthopedic expertise, heralding a new era of precision spine surgery.
How Can AI-Driven Biomechanical Models Improve Postoperative Rehabilitation Protocols for Spondylolisthesis Patients?
AI-driven biomechanical models can analyze postoperative spinal mechanics dynamically, predicting potential areas of instability or excessive loading during rehabilitation exercises. By simulating various movement patterns, these models inform customized physical therapy regimens that maximize spinal support while minimizing re-injury risk. This approach fosters a feedback loop wherein real-time patient data refines model accuracy, allowing continuous adjustment of rehabilitation strategies. Such integration enhances functional recovery and expedites return to daily activities, demonstrating the transformative potential of AI in postoperative care.
Integrating Genomic and Molecular Insights to Personalize Spondylolisthesis Treatment
Emerging research exploring the genomic and molecular underpinnings of spondylolisthesis reveals potential biomarkers linked to connective tissue integrity, inflammatory response, and bone remodeling. Identification of single nucleotide polymorphisms (SNPs) associated with increased vertebral slippage susceptibility could pave the way for genetic screening, enabling early detection and targeted preventive interventions. Furthermore, molecular therapies aimed at modulating extracellular matrix synthesis or inhibiting catabolic enzymes hold promise as adjuncts to traditional orthopedic treatments. These cutting-edge developments underscore the necessity for orthopedic clinicians to engage with translational research and precision medicine paradigms.
For a comprehensive exploration of AI applications in spine surgery and rehabilitation, consult the detailed analysis in this authoritative review published in the Journal of Orthopaedic Research.
Are you pioneering AI or biomechanical innovations in spondylolisthesis care? Share your findings with our professional network to catalyze advancements in orthopedic spine treatment.
Revolutionizing Spondylolisthesis Prognosis Through Machine Learning Analytics
Orthopedic experts are increasingly harnessing advanced machine learning techniques to decode complex datasets encompassing radiographic metrics, patient-reported outcomes, and biomechanical assessments. These AI-driven predictive models offer unprecedented granularity in forecasting spondylolisthesis progression, enabling stratification of patients into nuanced risk categories that inform personalized intervention timelines. By integrating longitudinal clinical parameters with high-resolution imaging data, practitioners can anticipate destabilization events and optimize surveillance protocols accordingly.
What Role Do Integrative AI Platforms Play in Enhancing Surgical Decision-Making and Postoperative Monitoring?
Integrative AI platforms synthesize multi-modal data streams, including intraoperative navigation feedback, preoperative imaging, and real-time physiological monitoring, to refine surgical planning and enhance postoperative care pathways. These systems utilize reinforcement learning to adapt recommendations based on patient-specific variables such as bone quality, neurological status, and functional baseline. Consequently, they facilitate dynamic adjustment of rehabilitation regimens and early detection of complications, thereby improving outcomes and reducing readmission rates.
Genomic Profiling: Pioneering Precision Medicine in Spinal Disorder Management
Cutting-edge genomic investigations have identified polymorphisms within genes regulating collagen synthesis, inflammatory cascades, and osteogenic pathways that correlate with heightened susceptibility to vertebral slippage. Integrating these molecular insights into clinical practice allows orthopedic specialists to stratify patients beyond conventional radiological criteria, tailoring prophylactic strategies and therapeutic modalities accordingly. Emerging pharmacogenomic approaches targeting matrix metalloproteinases and pro-inflammatory cytokines promise adjunctive benefits when combined with standard surgical and rehabilitative protocols.
Biomechanical Simulation and Custom Implant Fabrication: The Nexus of Engineering and Orthopedics
Advancements in finite element modeling and additive manufacturing have culminated in the creation of patient-specific implants that precisely replicate native vertebral geometry and biomechanical load distribution. This synergy mitigates deleterious stress concentrations and enhances osseointegration, reducing hardware failure risks. Furthermore, simulation-driven iterative design enables preoperative rehearsal of implant positioning and fusion strategies, fostering surgical precision and individualized care.
Integrating Multidisciplinary Expertise for Holistic Spondylolisthesis Management
Optimal management increasingly necessitates collaboration across orthopedic surgeons, biomechanical engineers, geneticists, and rehabilitation specialists. Such cross-disciplinary integration ensures comprehensive evaluation of patient-specific factors encompassing musculoskeletal integrity, genetic predisposition, and functional capacity. This paradigm fosters innovation in treatment algorithms that transcend traditional boundaries, aligning with evolving precision medicine frameworks.
For further exploration of AI-driven orthopedic innovations and genomic applications in spine care, consult this authoritative Journal of Orthopaedic Research review elucidating state-of-the-art methodologies and clinical implications.
Engage with the forefront of spondylolisthesis research: share your advanced clinical experiences or technological developments to propel the evolution of orthopedic spine care.
Expert Insights & Advanced Considerations
Precision in Patient-Specific Treatment Customization is Paramount
Recognizing the heterogeneity of spondylolisthesis presentations necessitates an individualized approach that integrates biomechanical assessment, genetic predisposition, and lifestyle factors. Orthopedic experts should prioritize comprehensive evaluations to tailor intervention strategies that optimally balance conservative care with timely surgical consideration.
Emerging Technologies Are Reshaping Diagnostic and Therapeutic Paradigms
The integration of AI-driven predictive analytics, 3D biomechanical modeling, and genomic profiling empowers clinicians to anticipate disease progression and personalize treatment. These technologies facilitate enhanced surgical planning, implant customization, and rehabilitation protocol optimization, ultimately improving long-term outcomes.
Multidisciplinary Collaboration Enhances Holistic Patient Outcomes
Effective management increasingly depends on coordinated efforts among orthopedic surgeons, biomechanical engineers, rehabilitation specialists, and geneticists. Such synergy fosters innovation, ensuring that therapeutic decisions incorporate advances in molecular biology and engineering, which are critical for addressing complex spinal pathologies like spondylolisthesis.
Proactive Osteoporosis Management is Integral to Surgical Success
Addressing bone quality through pharmacologic and nutritional strategies before and after spinal fusion reduces hardware complications and adjacent segment degeneration. Orthopedic specialists should advocate for routine bone density assessments and interdisciplinary management to fortify vertebral integrity.
Neuromuscular Re-education is Essential for Sustained Functional Recovery
Postoperative rehabilitation protocols that emphasize neuromuscular control and proprioceptive training mitigate compensatory movement patterns and enhance spinal stability. Incorporating these evidence-based techniques is vital for optimizing patient mobility and preventing recurrence.
Curated Expert Resources
Journal of Orthopaedic Research – Special Issue on AI and Biomechanics in Spine Surgery: A comprehensive review elucidating cutting-edge methodologies in AI applications and biomechanical simulations, essential for staying abreast of innovations in spine care.
Physiopedia – Neuromuscular Re-education in Spinal Disorders: An authoritative resource detailing evidence-based rehabilitation strategies that enhance functional outcomes post lumbar fusion and other spinal interventions.
NCBI PMC Article on Spinal Stability and Surgical Techniques: Peer-reviewed clinical studies offering in-depth analysis of surgical approaches like TLIF and PLIF, emphasizing biomechanical efficacy and patient selection criteria.
Specialized Treatment Plans for Spondylolisthesis at NJOrthopedicDoctor: Detailed protocols and expert recommendations tailored to spondylolisthesis subtypes and patient profiles, available at this link.
Comprehensive Review on Minimally Invasive Back Pain Treatments: Practical insights into non-invasive modalities and recovery optimization strategies, accessible via this resource.
Final Expert Perspective
In the evolving landscape of spondylolisthesis management, the convergence of precision medicine, advanced biomechanical engineering, and integrative rehabilitation paradigms marks a transformative era. Orthopedic clinicians must embrace these multifaceted innovations to refine diagnostic accuracy, customize therapeutic approaches, and enhance functional recovery tailored to each patient’s unique anatomy and pathology. For those seeking to elevate their practice or deepen their understanding, engaging with expert communities and exploring specialized resources such as recommended orthopedic spine specialists can provide invaluable guidance. Continuing dialogue and shared expertise remain pivotal in advancing the standards of care for spondylolisthesis patients worldwide. To initiate collaborative discussions or access further expert consultation, visit NJ Orthopedic Doctor’s contact page.


The detailed explanation of the multimodal approach to treating spondylolisthesis really resonated with me, especially the emphasis on tailored core stabilization exercises and bracing to reduce vertebral stress. From my observation, many patients often focus solely on pain management without appreciating how biomechanical rehabilitation plays a vital role in improving spinal stability and long-term outcomes. I also found the discussion on when surgical intervention becomes necessary particularly helpful. The mention of minimally invasive techniques like TLIF and PLIF as biomechanically sound options aligns with recent advances I’ve read about, which reduce recovery times significantly.
One aspect I’m curious about is how orthopedic specialists balance the timing and progression of neuromuscular re-education in post-surgical rehabilitation. Given its importance for retraining motor control and enhancing proprioception, how do clinicians ensure the rehab protocol adapts dynamically to individual patient recovery rates without risking overloading the spine prematurely? Has anyone had experiences with AI-driven rehab programs that tailor therapy sessions based on real-time patient feedback? It seems like this could be a game-changer in optimizing recovery while minimizing the risk of re-injury.
This post offers an enlightening overview of the complexities involved in managing spondylolisthesis, especially highlighting the importance of a balanced approach between conservative and surgical treatments. I particularly appreciate the emphasis on patient-specific factors, like age and etiology, which are often overlooked in the broader discussion. From my clinical experience, I’ve seen how tailored programs incorporating biomechanical modeling and regenerative therapies can make a significant difference in patient outcomes. The integration of advanced technologies like AI and 3D modeling is promising, but implementing these in the clinic requires careful validation to ensure they truly add value.
Regarding neuromuscular re-education, I wonder how practitioners can best monitor and adjust protocols in real-time, particularly during the fragile post-op phase. Have any of you employed or considered AI-powered systems that provide immediate feedback and adapt therapy intensity? It seems promising for preventing overloading and guiding optimal recovery. I’d love to hear about real-world examples or research findings that demonstrate the effectiveness of such technology in postoperative care. How do you see these innovations shaping future rehab strategies for spondylolisthesis?