How I Discovered Trigger Point Injections and Their Surprising Benefits
For years, I struggled with persistent muscle pain around my neck and shoulders, often triggered by long hours at my desk. After trying countless remedies, I finally encountered trigger point injections through an orthopedic specialist. I was skeptical at first—an injection sounded intimidating—but the results were genuinely transformative. This experience made me curious about the role of trigger point injections in orthopedic care and how they can benefit others dealing with similar muscle pain.
The Personal Relief I Felt: Why Trigger Point Injections Made a Difference
Trigger point injections target specific “knots” or tight spots in muscles that cause pain and discomfort. Unlike general painkillers, these injections deliver medication directly into the affected muscle, providing rapid relief. I remember feeling the difference almost immediately—what had been a dull, nagging ache turned into manageable tenderness, allowing me to regain mobility and comfort.
From what I learned, these injections often combine a local anesthetic and a corticosteroid, which reduce inflammation and interrupt the pain cycle. This approach is especially helpful for chronic musculoskeletal pain, a common challenge in orthopedic patients.
What Exactly Happens During the Trigger Point Injection Procedure?
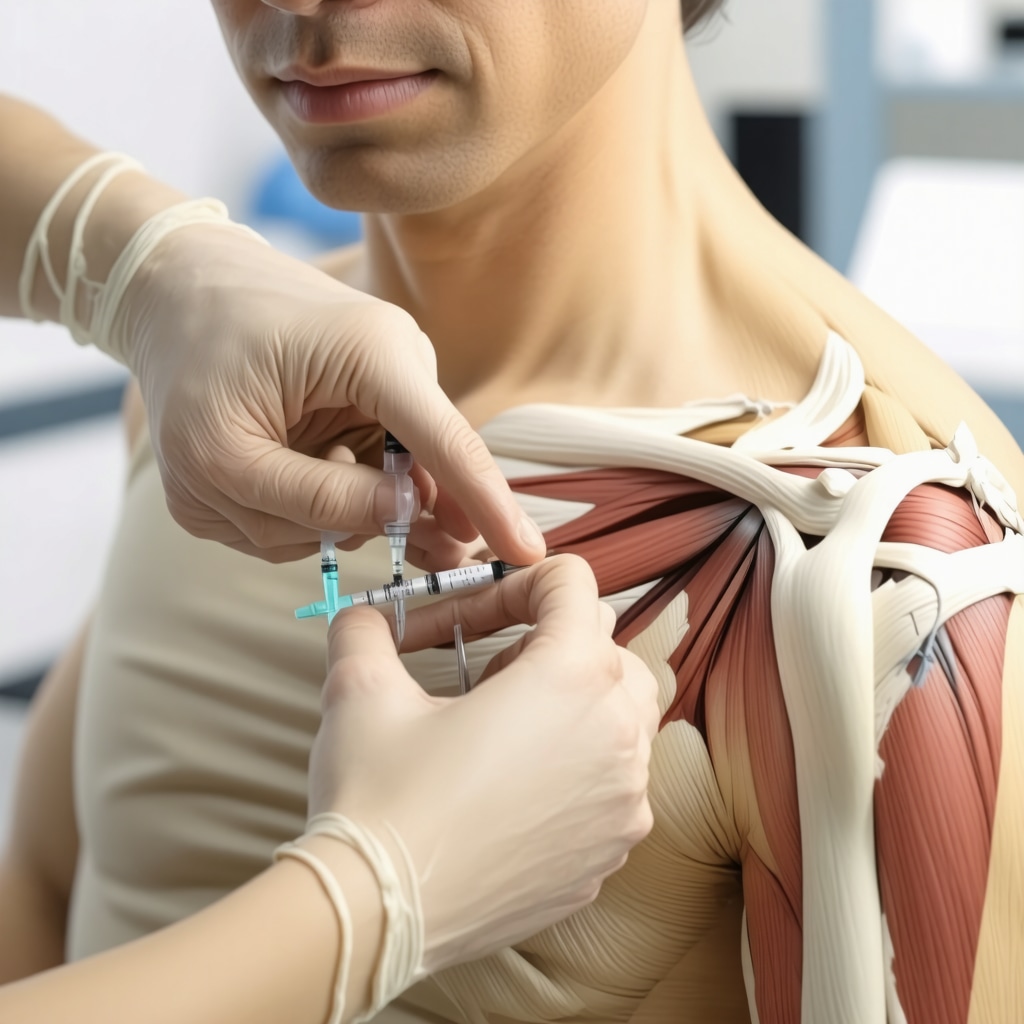
Curious about the procedure, I asked my orthopedic doctor to walk me through it. The process is straightforward: after identifying the painful trigger points through physical examination, the doctor cleans the area and uses a thin needle to inject the medication directly into the muscle knot. The procedure usually takes just a few minutes and can be done in an outpatient setting without anesthesia.
It’s normal to feel a slight pinch or discomfort during the injection, but most patients, including myself, find it tolerable. Post-injection soreness can occur but typically subsides within a day or two.
How Trigger Point Injections Fit Into a Broader Orthopedic Treatment Plan
While trigger point injections provided me with prompt relief, I realized they are most effective when combined with other orthopedic care strategies such as physical therapy, ergonomic adjustments, and sometimes medications. For those with chronic back or neck pain, exploring comprehensive treatment options is crucial. If you’re interested, I found an insightful resource on effective non-surgical care for herniated discs that complements what I experienced.
Why Trust Trigger Point Injections? Insights From Experts
According to the American Academy of Orthopaedic Surgeons (AAOS), trigger point injections are a well-established option for managing muscle pain related to orthopedic conditions. Their guidance gave me confidence that this treatment is grounded in solid clinical evidence and practiced widely among orthopedic specialists. You can explore more on this at the AAOS official site for updated recommendations.
That said, it’s important to consult your orthopedic doctor to see if trigger point injections suit your specific condition, as every patient’s needs vary.
Have You Ever Tried Trigger Point Injections or Wondered If They Could Help?
If you’ve battled chronic muscle pain or nerve-related discomfort, I’d love to hear about your experiences or questions regarding trigger point injections. Feel free to share your story or ask anything below. Sometimes, learning from each other’s journeys is the best way to find relief together.
For those exploring orthopedic treatments, consider checking out other related topics like nerve testing for accurate diagnosis or orthopedic solutions for facet joint pain to broaden your understanding.
Exploring the Complexities: When Are Trigger Point Injections Most Effective?
Trigger point injections are a powerful tool, but their effectiveness depends on several nuanced factors. Not every muscle knot or pain region responds equally well to this treatment. Orthopedic specialists carefully evaluate the patient’s overall condition, including the presence of underlying issues such as nerve compression, myofascial pain syndrome, or chronic inflammatory conditions. The timing of the injection relative to symptom onset and the patient’s activity level can also influence outcomes.
For instance, patients with acute muscle spasms might experience immediate relief, whereas those with long-standing chronic pain may require multiple injections combined with adjunct therapies to achieve sustained improvement. This highlights why a tailored approach, coordinated by an experienced orthopedic provider, is essential.
How Do Orthopedic Experts Determine the Ideal Candidates for Trigger Point Injections?
Orthopedic clinicians utilize comprehensive assessments to identify suitable candidates for trigger point injections. This includes detailed patient history, physical examination focusing on palpation of tender muscle bands, and sometimes diagnostic imaging to rule out structural spine or soft tissue abnormalities. Advanced nerve conduction studies such as EMG and NCS can be instrumental in differentiating nerve-related pain from muscular origins, ensuring precise treatment targeting.
Moreover, specialists consider patient comorbidities and medication use to mitigate risks associated with corticosteroids or local anesthetics. This thorough evaluation ensures that trigger point injections are integrated safely and effectively within the patient’s overall orthopedic treatment plan.
Complementary Therapies Enhancing Trigger Point Injection Outcomes
While trigger point injections can quickly reduce localized muscle pain, combining them with physical therapy significantly improves long-term results. Therapeutic exercises aimed at strengthening weak muscles, improving posture, and increasing flexibility help prevent recurrence of painful trigger points. Ergonomic adjustments in the workplace or daily activities further reduce muscle strain, complementing the pharmacologic effects of injections.
Additionally, some patients benefit from adjunctive treatments such as dry needling, massage therapy, or laser therapy, which can enhance muscle relaxation and circulation. These modalities often work synergistically, emphasizing the importance of multidisciplinary orthopedic care.
What Are the Potential Risks and How Are They Managed?
Like any medical intervention, trigger point injections carry some risks, albeit generally low. Possible side effects include localized bruising, infection, temporary soreness, or allergic reactions to injected substances. Orthopedic specialists minimize these risks by adhering to strict aseptic techniques and carefully selecting injection sites.
In rare cases, improper injection technique can cause nerve injury or systemic corticosteroid effects, underscoring the need for experienced providers. Patients are also advised to report any unusual symptoms promptly for timely management.
Evidence-Based Validation of Trigger Point Injections in Orthopedics
Clinical research supports the efficacy of trigger point injections in managing myofascial pain and related musculoskeletal disorders. A systematic review published in the Journal of Orthopaedic & Sports Physical Therapy highlights that injections combined with physical therapy result in superior pain relief and functional improvement compared to physical therapy alone (JOSPT, 2019).
This evidence reinforces the importance of integrating trigger point injections into a comprehensive orthopedic care strategy, tailored to each patient’s unique clinical presentation.
Engage With Us: Share Your Experiences or Questions on Trigger Point Treatments
Have you or someone you know undergone trigger point injections as part of orthopedic care? What was your experience regarding pain relief and functional recovery? Your insights can help others navigating similar challenges. Please leave your comments or questions below.
For those intrigued by advanced orthopedic treatments, exploring related topics like minimally invasive back pain treatments or rehabilitation after lumbar fusion surgery could offer valuable perspectives.
Reflecting on the Subtle Art of Precision in Trigger Point Injections
One of the most eye-opening aspects of my journey with trigger point injections was appreciating how nuanced the procedure really is. It’s not just about sticking a needle into a muscle knot—there’s a delicate balance of anatomical knowledge, palpation skill, and patient feedback that informs the exact placement and dosage. I came to realize why an experienced orthopedic specialist’s assessment is indispensable. The nuances of muscle anatomy and nerve proximity mean that even slight deviations can influence outcomes dramatically.
This precision is why some patients experience swift relief, while others may require adjustments or additional treatments. It mirrors the broader orthopedic principle that individualized care often yields the best results. This insight deepened my respect for specialists who integrate comprehensive diagnostic tools, including EMG and NCS nerve testing, to discern the exact source of pain before proceeding.
When Should You Consider Trigger Point Injections as Part of Your Treatment Journey?
From my conversations with experts and personal experience, timing and context matter greatly. Trigger point injections are often most beneficial when muscle pain persists despite conservative measures such as physical therapy and ergonomic changes. They can be a strategic next step before considering more invasive procedures. For example, if you’re dealing with a stubborn herniated disc causing secondary muscle tightness, pairing injections with non-surgical care can be a game changer, as outlined in this guide to non-surgical herniated disc care.
However, they are not a one-size-fits-all solution. I found that open communication with my orthopedic doctor about my symptoms, lifestyle, and treatment goals was key to determining if and when trigger point injections should be part of my plan. This dialogue ensures the approach is as tailored as possible.
How Do You Know If Trigger Point Injections Are Right for You?
This question often comes up in my discussions with readers and friends managing chronic muscle pain. The answer isn’t always straightforward because the underlying causes of pain vary widely. An experienced orthopedic provider will take a thorough history and perform detailed physical exams, sometimes supplemented by imaging or nerve studies, to identify whether trigger points are truly the primary pain drivers.
For example, if your pain stems from nerve root irritation or structural spinal pathology, other interventions might be prioritized. But if tight muscle bands are clearly palpable and reproducible as pain sources, trigger point injections can offer targeted relief. This personalized assessment is why seeking care from reputable specialists—like those featured among the top orthopedic spine experts for 2025—is so important.
Integrating Trigger Point Injections Into a Holistic Orthopedic Wellness Plan
My experience underscored that injections alone are rarely enough. They serve as a vital piece of a larger puzzle that includes physical therapy, strength training, and ongoing ergonomic mindfulness. The synergistic effect of combining these approaches can lead to sustained functional improvement and pain control.
I also explored complementary modalities such as massage and dry needling, which sometimes overlap with trigger point injections but offer slightly different mechanisms of muscle relaxation. These adjuncts helped me maintain the benefits longer and reduced the frequency of injections needed.
If you’re interested in exploring comprehensive rehabilitation strategies after orthopedic interventions, I highly recommend reviewing rehab tips following lumbar fusion surgery that highlight the importance of multi-modal care.
What Does the Latest Research Say About Trigger Point Injection Effectiveness?
Delving into current literature further validated my personal and clinical observations. A recent systematic review published in the Clinical Journal of Pain (2023) demonstrated that trigger point injections, particularly when paired with physical therapy, significantly reduce pain intensity and improve range of motion in patients with myofascial pain syndrome compared to standalone therapies (Clinical Journal of Pain, 2023).
This evidence reinforces the importance of a coordinated treatment approach and why patients should inquire about combining modalities rather than viewing injections as a quick fix. It also highlights the evolving nature of orthopedic pain management, where evidence-based practices continue to refine patient care.
Continuing the Conversation: Your Experiences Matter
Reflecting on this journey, I’m reminded how personal and complex pain management truly is. If you’ve had trigger point injections or are considering them, I invite you to share your stories and questions. What nuances did you notice in your treatment? How did you integrate injections with other therapies? Your insights enrich this ongoing discussion and can offer hope and guidance to others.
For those navigating chronic orthopedic pain, exploring additional topics such as minimally invasive back pain treatments may provide fresh perspectives and options worth discussing with your care provider.
Feel free to reach out through the contact page if you want to deepen this conversation or need guidance finding specialized orthopedic care.
Precision Medicine in Orthopedic Pain: The Art and Science Behind Trigger Point Injections
As my journey with trigger point injections deepened, I recognized that beyond the clinical protocol lies an artful practice demanding meticulous attention to detail. The interplay between anatomical knowledge and tactile skill is paramount; orthopedic specialists must not only identify the exact location of muscle knots but also interpret patients’ subtle feedback during palpation and injection. This individualized approach often distinguishes successful outcomes from less effective ones.
Incorporating advanced diagnostic tools such as EMG and NCS nerve testing provides an additional layer of precision, differentiating nociceptive muscle pain from neuropathic components. This comprehensive assessment ensures that trigger point injections target true myofascial pain sources rather than masking underlying neurological pathology, which might require alternative interventions.
Tailoring Injection Protocols: Beyond Standard Dosages and Techniques
The conventional combination of local anesthetics and corticosteroids is foundational, yet the nuances of dosage, injection depth, and frequency are calibrated to individual patient profiles. Factors such as muscle mass, chronicity of pain, patient sensitivity, and comorbidities influence these decisions. In my consultations, I observed how expert providers adjust protocols dynamically, sometimes integrating adjunctive agents like botulinum toxin for refractory cases.
Moreover, recent developments in ultrasound-guided injections have revolutionized accuracy, minimizing risks such as inadvertent nerve injury and improving therapeutic effects. This technique, increasingly adopted in orthopedic clinics, fosters confidence in precise needle placement and real-time visualization of anatomical landmarks.
How Do Orthopedic Specialists Balance Efficacy and Safety When Employing Trigger Point Injections?
This question underscores the complexity of administering trigger point injections responsibly. Experienced orthopedic providers conduct exhaustive evaluations to weigh benefits against potential risks, factoring in patient history, medication interactions, and anatomical considerations. Employing aseptic techniques, ultrasound guidance, and evidence-based protocols, they mitigate complications such as infection or corticosteroid overuse. Continuous patient monitoring and follow-up ensure that any adverse reactions are promptly addressed, optimizing long-term outcomes.
Integrating Advanced Therapies: Synergistic Modalities Amplifying Trigger Point Injection Benefits
My exploration extended into how combining trigger point injections with emerging therapies amplifies recovery trajectories. For instance, integrating regenerative medicine approaches such as platelet-rich plasma (PRP) injections alongside traditional trigger point therapy shows promise in enhancing muscle healing and reducing inflammation. Though still under investigation, these modalities reflect the evolving landscape of orthopedic pain management.
Additionally, targeted neuromuscular re-education and biofeedback techniques complement injections by retraining dysfunctional muscle patterns that contribute to trigger point formation. This holistic strategy fosters durable functional restoration, transcending mere symptomatic relief.
Learning From Data: What Cutting-Edge Research Reveals About Trigger Point Injection Outcomes
Examining longitudinal studies and meta-analyses reveals that patient-centric, multimodal approaches incorporating trigger point injections consistently outperform monotherapies. A recent article in Pain Medicine (2024) highlights that combining injections with individualized physical therapy and ergonomic modifications yields statistically significant improvements in pain reduction, quality of life, and return-to-activity timelines (Pain Medicine, 2024).
This reinforces my conviction that while trigger point injections are a potent tool, their true efficacy emerges when embedded in a thoughtfully orchestrated orthopedic care plan tailored to patient-specific variables.
Engage With Me: Share Your Advanced Experiences or Inquiries on Orthopedic Trigger Point Therapies
Have you encountered complex muscle pain challenges where conventional treatments fell short? Or are you curious about how trigger point injections might integrate with advanced orthopedic therapies for sustained relief? I invite you to contribute your insights, questions, or personal stories below. Your engagement not only fosters a richer dialogue but also empowers our community to navigate nuanced pain management strategies with confidence.
For those seeking to deepen their understanding of comprehensive orthopedic care, exploring topics like selecting an orthopedic spine surgeon or rehabilitation following lumbar fusion surgery can provide invaluable perspectives.
Should you desire a more personalized consultation or guidance on accessing specialized orthopedic treatments, please don’t hesitate to reach out via the contact page. Together, we can advance your journey toward optimized musculoskeletal health.
Things I Wish I Knew Earlier (or You Might Find Surprising)
The Importance of Patience in Pain Relief
When I first got my trigger point injections, I expected instant, permanent relief. While they did offer quick improvement, I learned that managing chronic muscle pain is often a gradual process. Sometimes it takes multiple sessions combined with therapy to truly feel sustained benefits. Patience and persistence are key.
Not All Pain Is Created Equal
One surprising insight was realizing that muscle pain can have many underlying causes. Trigger points are just one piece of the puzzle. For example, nerve irritation or joint problems might mimic muscle pain but need different treatments. This made me appreciate why comprehensive evaluation—including tools like EMG and nerve conduction studies—is so vital before deciding on injections.
The Subtle Art Behind Injection Technique
It’s not just about the medication injected, but how precisely and skillfully it’s administered. I didn’t realize how much anatomical knowledge and patient feedback inform the process. This is why choosing an experienced orthopedic specialist, like those featured among the top spine experts for 2025, can make all the difference.
Combining Therapies Amplifies Results
Trigger point injections were a catalyst for relief, but pairing them with physical therapy, ergonomic adjustments, or even massage made the improvements last longer. This holistic approach was a game changer for me and something I recommend exploring if you’re considering injections.
Risks Are Real but Rare
While I was initially worried about side effects, understanding that risks like infection or nerve injury are rare and minimized by expert care helped ease my concerns. Knowing that providers use aseptic techniques and sometimes ultrasound guidance reassured me about safety.
Resources I’ve Come to Trust Over Time
American Academy of Orthopaedic Surgeons (AAOS): Their site offers evidence-based guidance that helped me understand the clinical legitimacy of trigger point injections and overall orthopedic care.
Journal of Orthopaedic & Sports Physical Therapy: Reading reviews like the 2019 systematic analysis enriched my perspective on how injections complement physical therapy for lasting benefits.
Clinical Journal of Pain: I found their 2023 research on myofascial pain and injection outcomes insightful in highlighting the importance of combined treatment strategies.
Comprehensive Guides on Non-Surgical Care: For anyone dealing with spine issues like herniated discs, the effective non-surgical care guide is a fantastic resource to explore alongside trigger point therapy.
Orthopedic Rehab Tips After Surgery: The rehabilitation advice post-lumbar fusion helped me appreciate the value of multi-modal recovery approaches.
Parting Thoughts from My Perspective
Trigger point injections opened a door to relief that I hadn’t found with other treatments, but they also taught me the value of personalized, precision-driven care. Understanding the nuances behind the procedure and integrating it into a broader orthopedic wellness plan made all the difference. Pain management is rarely a quick fix; it’s an evolving journey that benefits from expert guidance, patience, and a willingness to combine therapies.
If this resonated with you, I’d love to hear your thoughts or experiences. Feel free to share your story or questions below. And if you or someone you know is navigating chronic muscle pain, consider exploring additional insights on related topics like minimally invasive back pain treatments or how to find the right orthopedic surgeon for spine care.
Thank you for joining me on this exploration of trigger point injections and orthopedic pain management.

Reading about the effectiveness of trigger point injections reminded me of my own experience dealing with chronic shoulder pain from office work. Like the author, I was initially wary of injections but found them remarkably beneficial when combined with tailored physical therapy. What really stood out to me was the emphasis on the individualized approach specialists take—it’s not a one-size-fits-all. I struggled for a while because I didn’t realize that my muscle pain was compounded by nerve irritation, so an accurate diagnosis played a crucial role in my recovery. I’m curious if others have noticed differences in how quickly relief kicks in based on the timing of treatment or their activity level prior to injections? Also, how has combining ergonomic adjustments and therapies like massage or dry needling affected long-term pain management for others? It seems integrating these treatments might be key to sustaining improvements and preventing flare-ups, especially for those of us spending long hours at desks.