My Personal Encounter with Nerve Block Orthopedic Management
As someone who’s navigated the challenging waters of chronic pain, I vividly remember the moment I first heard about nerve block procedures. Initially, I was skeptical, much like many patients I’ve spoken with. But after experiencing persistent back pain that no conventional treatment seemed to alleviate, I decided to explore this innovative approach. My journey into nerve block orthopedic management opened my eyes to the potential of targeted pain relief techniques that really work.
What Is a Nerve Block and How Does It Work?
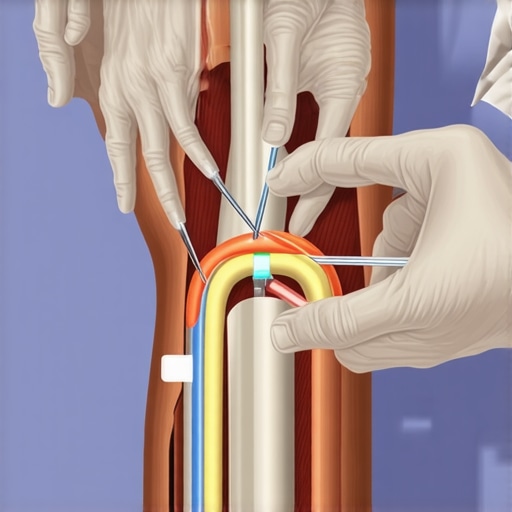
A nerve block is a procedure where anesthetic or anti-inflammatory medication is injected near specific nerves to block pain signals. In my case, my orthopedic specialist explained that this could provide temporary relief, giving my body a much-needed break from persistent discomfort. The procedure is minimally invasive and often performed under imaging guidance, such as fluoroscopy, to ensure precise placement. I found this process surprisingly straightforward, and the immediate reduction in pain was remarkable.
Why I Chose Nerve Blocks for My Pain Management
Living with degenerative disc disease, I was at my wit’s end with pain medications that only masked symptoms and had side effects. My doctor explained that nerve blocks could serve as both diagnostic and therapeutic tools, helping identify pain sources and providing relief. This dual role made me feel more confident about trying the procedure. Additionally, I learned that nerve blocks could be part of a broader treatment plan, including physical therapy and lifestyle modifications, which I was eager to pursue.
My Experience and Insights into the Procedure
The day of my nerve block was surprisingly uneventful. Under local anesthesia, the doctor guided the needle to the targeted nerve area. I appreciated the use of real-time imaging to enhance accuracy. Post-procedure, I noticed a significant drop in pain levels that lasted several hours, and for the first time in weeks, I could move more freely. However, I also learned that the relief might be temporary, and repeated procedures could be necessary for sustained benefits, as highlighted by the National Institute of Neurological Disorders and Stroke.
Is a Nerve Block Right for You? My Personal Reflection
How Do You Know When a Nerve Block Is the Next Step?
If you’re experiencing chronic pain that hasn’t responded well to conservative treatments, discussing nerve blocks with your orthopedic specialist might be worthwhile. They can help determine if imaging studies and diagnostic injections could pinpoint the pain source more accurately. Remember, each case is unique, and professional guidance is essential.
If you’re contemplating this treatment, I recommend consulting reputable sources like the National Institute of Neurological Disorders and Stroke for comprehensive information.
Have you tried nerve blocks or other minimally invasive procedures? Share your experiences in the comments—I’d love to hear your story!
Exploring the Nuances of Non-Surgical Pain Relief Options
While nerve blocks are a popular minimally invasive procedure for targeted pain relief, they are just one part of a comprehensive orthopedic pain management strategy. Advanced techniques, such as epidural steroid injections and radiofrequency ablation, offer additional avenues for patients seeking relief without immediate surgery. These procedures are often guided by imaging technology, ensuring precision and safety, and can be tailored to address specific sources of pain, such as facet joint syndrome or nerve root compression.
Understanding When to Elevate Treatment: The Expert’s Perspective
Determining the right time to escalate from conservative therapies to more invasive interventions requires a nuanced understanding of patient response and diagnostic accuracy. For instance, if a patient’s pain persists despite physical therapy and medication, a detailed diagnostic workup—including advanced imaging like MRI or CT scans—may reveal underlying issues such as disc herniation or spinal stenosis that warrant procedural intervention. Consulting with a specialist skilled in spinal surgery consultation can provide clarity on this decision.
What Are the Long-Term Benefits of Combining Multiple Modalities?
Integrating various treatment options—such as nerve blocks, physical therapy, and lifestyle modifications—can significantly improve outcomes for chronic pain sufferers. This multidisciplinary approach not only alleviates symptoms but also addresses root causes, potentially reducing the need for repeated procedures. For example, combining nerve blocks with targeted rehabilitation, as outlined in post-surgical rehab strategies, can enhance mobility and functional recovery.
How do expert clinicians determine the most effective combination of therapies for each patient?
This process involves a thorough assessment of the patient’s medical history, diagnostic imaging, and response to previous treatments. Skilled orthopedic specialists consider factors such as the severity of degeneration, presence of nerve impingement, and overall health to craft personalized plans. Evidence-based guidelines, like those from the American Academy of Orthopaedic Surgeons, support these decisions, ensuring treatments are both safe and effective.
For those interested in exploring non-surgical avenues first, resources like non-surgical care options can provide valuable insights into alternative therapies.
If you’re considering a comprehensive evaluation or seeking expert guidance, don’t hesitate to reach out to a qualified orthopedic specialist. Sharing your experiences or asking for tailored advice can often lead to better, more informed decisions about your pain management journey.
Beyond the Surface: The Complexities of Nerve Blocks in Orthopedic Care
My journey into nerve block procedures has not only been a personal quest for relief but also an ongoing exploration of their intricate mechanisms and potential. I’ve come to realize that understanding the nuanced interplay of anatomy, pharmacology, and technology is crucial for both clinicians and patients aiming for optimal outcomes.
What Are the Hidden Layers of Nerve Block Effectiveness?
When I first experienced relief after my nerve block, I was amazed at how targeted the treatment was. However, I soon learned from advanced studies, such as those highlighted by the American Academy of Orthopaedic Surgeons, that the success of nerve blocks hinges on precise anatomical knowledge and real-time imaging guidance. The complexity lies not just in the injection itself but in accurately identifying the nerve pathways and understanding how individual variations can influence results.
How Do Emerging Technologies Enhance Personal Outcomes?
With the rapid development of imaging modalities like 3D fluoroscopy and ultrasound-guided injections, my experience has become increasingly refined. These innovations minimize the risk of misplacement and improve the duration of pain relief. As I reflect on my own treatment, I recognize that staying abreast of these technological advances is essential for anyone involved in pain management. They open new avenues for personalized care, making procedures safer and more effective.
What Are the Long-Term Implications of Repeated Nerve Blocks?
This question has intrigued me deeply, especially considering the potential for nerve sensitization or damage over multiple treatments. According to recent research published in the Journal of Orthopaedic Research, repeated nerve blocks can sometimes lead to nerve fibrosis or altered nerve physiology, which may impact future treatment options. As a patient and observer, I believe that a balanced approach—integrating nerve blocks with physical therapy, lifestyle modifications, and ongoing monitoring—can optimize long-term outcomes while minimizing risks.
Personal Reflections on Navigating Advanced Pain Management
My experience has taught me that nerve blocks are powerful tools, but they are part of a broader, nuanced landscape of orthopedic care. The decision to pursue such treatments should be made with a thorough understanding of the benefits and limitations, and in close consultation with experienced specialists. I’ve learned that ongoing education—both for clinicians and patients—is vital for navigating this evolving field.
If you’re exploring nerve blocks or other minimally invasive procedures, I encourage you to seek out reputable sources like the National Institute of Neurological Disorders and Stroke. Sharing your personal experiences or questions can also enrich the community’s collective knowledge. Are there aspects of nerve block treatments that you find particularly complex or promising? Feel free to comment below and join the conversation—your insight might inspire someone else’s journey toward pain relief.
Refining Pain Relief: The Role of Precision and Personalization in Nerve Blocks
My journey with nerve blocks has evolved from initial relief to a deep appreciation for the intricate balance of anatomy, technology, and individualized care. The success of these procedures depends heavily on precise anatomical knowledge and the use of advanced imaging modalities. Techniques such as ultrasound-guided injections have revolutionized the field, allowing for real-time visualization of nerve pathways, which minimizes complications and enhances efficacy. As described by the American Academy of Orthopaedic Surgeons, these innovations are pivotal in optimizing patient outcomes, especially in complex cases involving nerve entrapment or multifocal pain sources.
The Impact of Cutting-Edge Imaging Technologies on Personalized Outcomes
Incorporating 3D fluoroscopy and high-frequency ultrasound has dramatically improved the accuracy of nerve block placements. These technologies enable clinicians to tailor treatments to the patient’s unique anatomy, thus maximizing pain relief and reducing the need for repeated interventions. From my perspective, staying abreast of these tools has been essential in ensuring safe and effective care. Such advancements not only elevate procedural success rates but also contribute to a more personalized approach, aligning with the broader trend of precision medicine in orthopedics. For those interested in exploring these options further, resources like orthopedic imaging techniques offer valuable insights.
Are Repeated Nerve Blocks Detrimental or Beneficial in the Long Term?
This question has become increasingly relevant as I consider the long-term implications of multiple treatments. The literature, including a comprehensive review in the Journal of Orthopaedic Research, indicates that repetitive nerve blocks can sometimes lead to nerve fibrosis or altered nerve physiology, potentially complicating future interventions. However, when integrated into a multidisciplinary pain management plan—combining physical therapy, lifestyle modifications, and judicious use of nerve blocks—they can provide sustained relief without significant adverse effects. The key lies in careful patient selection and ongoing monitoring, ensuring that benefits outweigh risks. If you’re contemplating this approach, consulting with a specialist who understands these nuances is crucial. To explore personalized strategies, consider reaching out through professional consultation.
What Are the Emerging Trends That Could Transform Nerve Block Efficacy?
Emerging innovations such as nerve stimulation-guided injections and the integration of artificial intelligence for diagnostic precision are poised to further revolutionize orthopedic pain management. These technologies aim to enhance targeting accuracy, reduce procedure times, and improve patient outcomes. For example, AI algorithms can analyze imaging data to predict optimal injection sites, thereby increasing success rates. As I continue to follow these developments, I am excited about the potential they hold for customizing treatments even further. To stay informed about these advancements, I recommend engaging with expert communities and ongoing research publications.
If you’re eager to deepen your understanding of personalized orthopedic interventions or share your own experiences with nerve blocks, I invite you to connect with me. Your insights could contribute meaningfully to the ongoing conversation about innovative pain management strategies.
Things I Wish I Knew Earlier (or You Might Find Surprising)
1. The Power of Precision
When I first underwent a nerve block, I underestimated how crucial accurate placement is. The use of advanced imaging like ultrasound made a huge difference in ensuring the medication targeted the right nerve, leading to better relief. It’s amazing how technology can enhance outcomes when used properly.
2. Temporary Relief Can Be a Gateway
Initially, I thought nerve blocks were just a quick fix, but I realized they can provide valuable diagnostic information. Understanding whether pain improves after the block helps identify the source, guiding further treatment options.
3. Not All Relief is Permanent
My experience taught me that nerve blocks often need to be repeated, especially in chronic conditions. Patience and ongoing communication with your specialist are key to long-term management.
4. They’re Part of a Bigger Picture
Nerve blocks work best when integrated into a comprehensive treatment plan, including physical therapy and lifestyle changes. It’s a reminder that no single intervention is a silver bullet.
5. The Importance of Choosing the Right Specialist
Having an experienced orthopedic specialist guide you through the process makes all the difference. Their expertise in anatomy and imaging ensures safer, more effective procedures.
Resources I’ve Come to Trust Over Time
- National Institute of Neurological Disorders and Stroke (NINDS): This site provides reliable, research-backed information on nerve blocks and neurological treatments. I found it helpful for understanding the science behind the procedures.
- American Academy of Orthopaedic Surgeons (AAOS): Their guidelines and articles helped me grasp the latest advancements in orthopedic pain management, including minimally invasive procedures.
- PubMed and Medical Journals: For deeper dives into recent studies on nerve block longevity and safety, these sources are invaluable. I recommend them if you want to explore the research behind clinical practices.
Parting Thoughts from My Perspective
Experiencing nerve block orthopedic management firsthand has shown me how much precision, technology, and personalized care matter. These procedures can offer significant relief and valuable insights into your pain sources, but they’re most effective when part of a broader, well-coordinated treatment plan. If you’re considering this route, I encourage you to consult with a knowledgeable specialist and explore all your options. Remember, managing pain is often a journey, and each step forward counts. If this resonated with you, I’d love to hear your thoughts or experiences—sharing our stories can truly make a difference. Feel free to reach out or leave a comment below.