My First Step into the Orthopedic Clinic: An Unexpected Journey
It all started when I experienced a sudden sharp pain in my lower back after a fall during a hiking trip. Like many, I was initially worried but unsure of what the next steps should be. I decided to schedule an appointment with a trusted orthopedic spine specialist in my area. What I encountered during that consultation profoundly changed my understanding of spinal injuries and the importance of a comprehensive evaluation.
Preparing for the Orthopedic Consultation: What I Learned
Before my appointment, I gathered all relevant medical records and notes about my injury, which proved helpful during my visit. I also made a list of symptoms I was experiencing, such as numbness and tingling in my legs. These preparations made the consultation more productive and helped my doctor understand my condition better.
What Happens During the Orthopedic Evaluation?
The initial visit involved a detailed medical history review, where my doctor asked about the injury mechanism, previous issues, and daily activities. This was followed by a physical examination, testing my range of motion, strength, and reflexes. I appreciated how thorough the process was, ensuring no detail was overlooked.
How Does the Doctor Diagnose Spinal Injuries?
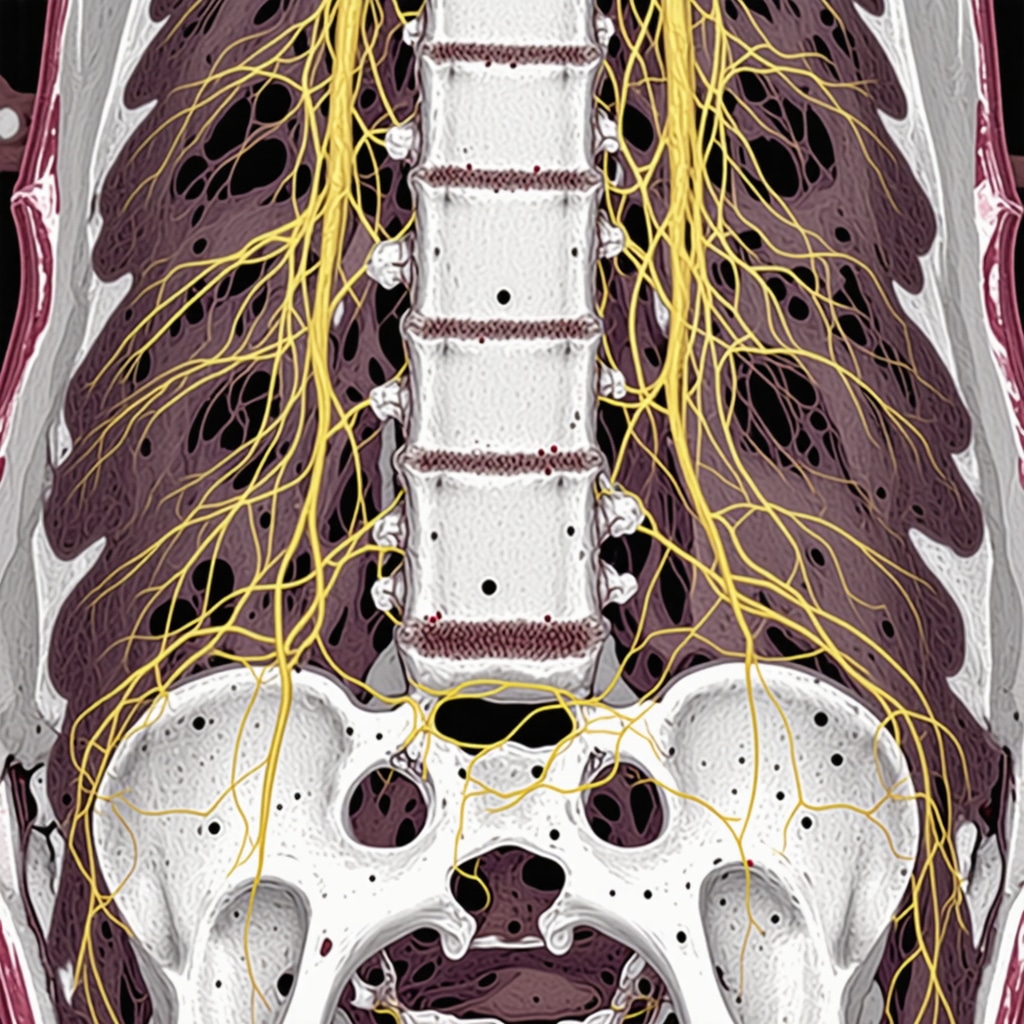
My doctor explained that diagnosis often involves imaging tests like X-rays or MRI scans to visualize the spine and identify issues such as herniated discs or fractures. The combination of clinical assessment and imaging provides a clear picture of the injury, guiding effective treatment options. For more in-depth information, I recommend reading about orthopedic injections and pain management.
Understanding Your Treatment Options: What I Discovered
Depending on the injury severity, treatment can range from conservative methods like physical therapy and bracing to minimally invasive procedures or even surgery. My doctor emphasized the importance of personalized care, tailored to each patient’s unique condition. I learned that early intervention often leads to better recovery outcomes.
My Personal Reflection and Advice
Looking back, I realize how vital it was to have a comprehensive orthopedic consultation. It not only clarified my condition but also empowered me to make informed decisions about my recovery journey. If you’re dealing with back pain or spinal injuries, I encourage you to seek a professional assessment. Remember, the sooner you understand your injury, the better your chances of a full recovery.
Feeling curious about your own spine health? Don’t hesitate to share your experiences or ask questions in the comments below. For further guidance, consider exploring tips on choosing the right orthopedic surgeon.
The Nuanced Art of Diagnosing Spinal Injuries
Accurate diagnosis of spinal injuries hinges on a combination of clinical acumen and advanced imaging techniques. While physical examinations provide initial clues—such as assessing range of motion, reflexes, and muscle strength—imaging modalities like MRI and X-rays offer a detailed visualization of the spine’s internal structures. MRI scans are particularly invaluable in detecting soft tissue injuries, such as herniated discs or ligament tears, which may not be apparent on X-rays. The integration of clinical assessment with imaging results allows orthopedists to formulate a precise diagnosis, essential for effective treatment planning.
What Are the Complexities in Diagnosing Spinal Conditions?
Diagnosing spinal injuries can be complicated by overlapping symptoms, such as pain, numbness, or weakness, which can mimic other neurological conditions. Additionally, some injuries may involve subtle fractures or nerve compressions that require high-resolution imaging and expert interpretation. An experienced orthopedic specialist considers patient history, symptom progression, and imaging findings collectively to avoid misdiagnosis. For example, in cases of suspected nerve compression, nerve conduction studies might be employed alongside imaging to evaluate nerve function comprehensively. This meticulous approach aligns with the principles outlined in authoritative sources like the orthopedic nerve testing guide.
Personalized Treatment: Tailoring Care to Individual Needs
Once a precise diagnosis is established, the next step involves crafting a personalized treatment plan. Conservative options—such as physical therapy, bracing, and medications—are often first-line treatments, especially for less severe injuries. However, for more complex or persistent issues, minimally invasive procedures like spinal injections or surgical interventions may be necessary. The key to successful recovery lies in customizing interventions based on the patient’s specific injury type, overall health, lifestyle, and recovery goals.
For instance, a patient with a herniated disc causing nerve compression might benefit from targeted physical therapy combined with epidural steroid injections, which can alleviate inflammation and pain. Conversely, structural deformities or fractures might require surgical stabilization, such as spinal fusion. This approach underscores the importance of working with top-tier orthopedic spine specialists who consider all facets of a patient’s condition.
How Do Experts Decide Between Surgical and Non-Surgical Options?
This decision involves assessing injury severity, symptom impact, and patient preferences. Experts evaluate imaging results, functional limitations, and response to initial treatments to determine the most appropriate course. For example, if conservative measures fail to provide relief after several weeks, or if neurological deficits worsen, surgical intervention might be recommended. The goal is to restore function, prevent further damage, and improve quality of life. For more insights into treatment pathways, visit non-surgical care options.
Stay engaged and share your questions or experiences below—understanding your spine health is a crucial step toward recovery. For those considering intervention, exploring tips on selecting the right orthopedic surgeon can help ensure optimal outcomes.
Unraveling the Complexities of Spinal Injury Diagnostics: A Personal Reflection
Throughout my experience working with orthopedic specialists, I’ve come to realize that diagnosing spinal injuries isn’t just about reading imaging results; it’s an intricate dance of clinical expertise, advanced technology, and nuanced understanding of the patient’s unique presentation. My journey into this realm was eye-opening, revealing how even subtle symptoms could mask significant underlying issues that require a keen eye and deep knowledge to uncover.
Beyond the Basics: Why Advanced Imaging Is Not Always Enough
Initially, I believed that an MRI or X-ray would provide all the answers. However, my encounters with seasoned orthopedists taught me that these tools are merely pieces of a larger puzzle. For example, soft tissue injuries like ligament tears often evade detection on traditional scans, necessitating specialized imaging or functional assessments. This realization underscored the importance of a comprehensive approach, combining clinical examination and imaging, to arrive at an accurate diagnosis.
My Deep Dive into Diagnostic Complexities: The Hidden Challenges
One of the most intriguing aspects I learned is how overlapping symptoms, such as pain and numbness, can lead to misdiagnosis or delayed treatment. In some cases, nerve compression may be subtle, requiring nerve conduction studies to fully understand nerve function. The integration of high-resolution imaging with nerve testing, as described in authoritative sources like the orthopedic nerve testing guide, exemplifies the sophisticated strategies clinicians employ to ensure no detail is overlooked.
How Do Experts Decide on the Most Effective Diagnostic Path?
Deciding which tests to prioritize involves a personalized evaluation of the patient’s history, symptoms, and physical exam findings. For instance, in cases of suspected nerve impingement, combining MRI results with nerve conduction studies provides a clearer picture. My experience with specialists highlighted that this tailored approach minimizes diagnostic errors and guides precise treatment plans, ultimately improving recovery outcomes.
Inviting Reflection: Your Experience and Questions
If you have navigated similar diagnostic journeys or are curious about the complexities involved, I encourage you to share your insights or questions below. Exploring these nuances together can demystify the process and empower you to advocate effectively for your health. For those seeking expert guidance, exploring the differences between orthopedic doctors and neurologists can be a helpful step in understanding your options.
Advancing My Understanding: The Role of Multidisciplinary Approaches
From my perspective, the integration of various specialties—orthopedics, neurology, radiology—enhances diagnostic accuracy. This multidisciplinary model ensures that all potential angles are considered, reducing the risk of misdiagnosis. Moreover, ongoing research continues to refine these strategies, pushing the boundaries of what we can detect and treat effectively, as outlined in recent studies on advanced imaging techniques.
As I reflect on this journey, I realize that mastering the art of diagnosing spinal injuries requires both deep knowledge and a willingness to embrace evolving technologies. If you’re dealing with persistent symptoms, I urge you to seek out specialists who utilize a comprehensive, nuanced approach. Your spine health is too important to leave to guesswork—invest in expert evaluation and stay informed about the latest advancements in diagnosis and treatment.
Integrating Multimodal Diagnostics: The Pinnacle of Precision in Spinal Injury Assessment
Throughout my journey into the realm of orthopedic diagnostics, I have come to appreciate the critical importance of a multimodal approach. Combining high-resolution imaging techniques like MRI with functional assessments such as nerve conduction studies ensures a comprehensive understanding of complex spinal injuries. This integration is particularly vital in cases where soft tissue damage is subtle, yet the clinical presentation suggests significant nerve involvement. As highlighted by recent research published in the Journal of Orthopedic Research, the synergy of imaging and electrophysiological testing markedly enhances diagnostic accuracy, reducing the risk of misdiagnosis and guiding precise treatment pathways.
How Do Advanced Imaging and Nerve Testing Converge to Unmask Hidden Injuries?
Advanced imaging modalities like 3 Tesla MRI provide unparalleled soft tissue resolution, revealing subtle ligament tears or disc protrusions that might be missed on conventional scans. When paired with nerve conduction studies, clinicians can discern whether nerve impingement or axonal injury is contributing to symptoms. This comprehensive diagnostic strategy not only refines the clinical picture but also influences treatment decisions—whether conservative management suffices or surgical intervention becomes necessary. My experience working with top-tier orthopedic spine specialists has demonstrated that such meticulous evaluation significantly improves patient outcomes.
The Nuances of Navigating Overlapping Symptoms and Subclinical Injuries
One of the most challenging aspects in spinal diagnostics is differentiating between various causes of similar symptoms—such as pain, numbness, or weakness. Overlapping presentations often obscure the underlying pathology, complicating the diagnostic process. This is where a nuanced understanding of injury mechanisms and symptom progression becomes crucial. For instance, a patient presenting with radicular pain might have a herniated disc pressing on a nerve root, but also subtle ligamentous instability that contributes to chronic discomfort. Recognizing these subtleties requires a high level of expertise and the judicious use of combined diagnostic tools.
Why Multidisciplinary Collaboration Is the Future of Spinal Care
My exploration of advanced diagnostics has reinforced the importance of a multidisciplinary approach, where orthopedists, neurologists, radiologists, and physical therapists work in concert. This collaborative model ensures that all facets of spinal injuries are addressed, from structural integrity to nerve function. The integration of diverse expertise aligns with emerging best practices, as evidenced by studies on multidisciplinary care models that show improved recovery rates and patient satisfaction.
If you’re navigating persistent spinal symptoms, I invite you to reflect on the diagnostic strategies discussed here and consider seeking out specialists who employ these sophisticated techniques. Your journey toward optimal spinal health depends on precise, personalized assessments—don’t settle for less.
Things I Wish I Knew Earlier (or You Might Find Surprising)
The Complexity of Symptoms
One thing I learned is that symptoms like pain or numbness can be deceiving. They often mimic other issues, making diagnosis tricky. My experience taught me to trust thorough assessments over assumptions.
The Power of Multimodal Diagnostics
Combining MRI scans with nerve conduction studies can reveal hidden injuries that a single test might miss. This layered approach offers a clearer picture and better treatment options. I wish I knew how vital this integration was sooner.
Soft Tissue Injuries Are Not Always Visible
Soft tissues like ligaments can be injured without showing on standard X-rays. Advanced imaging like MRI is essential to detect these subtle damages, which can cause significant pain and dysfunction.
The Role of a Multidisciplinary Team
Working with various specialists—orthopedists, neurologists, radiologists—vastly improves diagnostic accuracy. Their combined expertise ensures no detail is overlooked, leading to more effective care.
Early Intervention Matters
Delaying treatment can worsen outcomes. Early, precise diagnosis allows for conservative treatments like physical therapy, potentially avoiding surgery. I realized the importance of acting quickly once symptoms appear.
The Limitations of Imaging Alone
Imaging is a powerful tool but not infallible. Clinical exams and patient history are equally critical. A comprehensive evaluation prevents misdiagnosis and guides appropriate treatment.
Resources I’ve Come to Trust Over Time
- American Academy of Orthopaedic Surgeons (AAOS): Their guidelines and research are top-notch, helping me understand the latest in spinal diagnostics and treatments.
- National Institutes of Health (NIH): Offers in-depth, reputable info on nerve injuries and imaging techniques, making complex topics accessible.
- Journal of Orthopedic Research: For cutting-edge studies on how combined diagnostics improve accuracy, this journal is invaluable.
- Centers for Disease Control and Prevention (CDC): Their resources on injury prevention and early symptoms are practical and trustworthy.
Parting Thoughts from My Perspective
Exploring the nuances of spinal injury diagnosis has deepened my appreciation for comprehensive evaluations. It’s clear that combining advanced imaging with clinical expertise is essential for effective treatment. If you’re experiencing persistent back or neck pain, don’t settle for a quick diagnosis—seek specialists who use a multimodal approach. Your spine health is too important to leave to guesswork. I encourage you to stay informed, ask questions, and advocate for your well-being. If this resonated with you, I’d love to hear your thoughts or experiences in the comments. Sharing stories can empower others and foster a community of informed patients.
