Discovering the Power of Trigger Point Injections: My Personal Experience
As someone who has struggled with chronic back pain for years, I was eager to explore all available treatment options. When my orthopedic specialist recommended trigger point injections, I was initially skeptical but decided to give it a try. The relief I experienced was transformative, inspiring me to learn more about this minimally invasive procedure and share my insights with others.
What Exactly Are Orthopedic Trigger Point Injections?
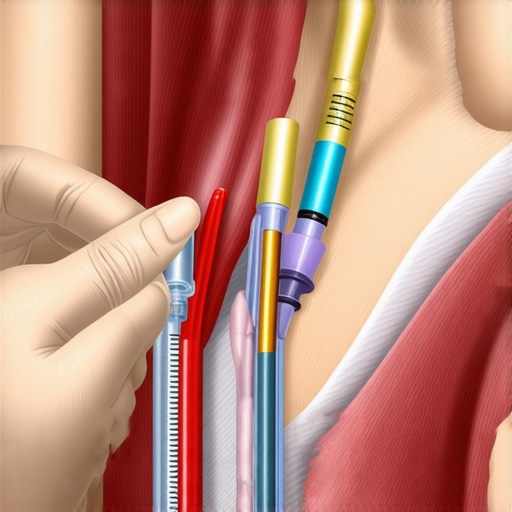
Trigger point injections are a targeted approach to alleviate muscle pain caused by myofascial trigger points—small, tender areas within muscles. During the procedure, a doctor injects medication directly into these points, often providing rapid pain relief. Over time, I found this approach to be effective for managing my discomfort and improving mobility.
My Journey Through the Procedure
The process was surprisingly straightforward. My doctor used ultrasound guidance to precisely locate the trigger points, ensuring the injections were accurate. The procedure took about 30 minutes, and I was able to return home the same day. I noticed significant pain reduction within days, and my daily activities became much more manageable.
What Are the Benefits of Trigger Point Injections?
From my personal perspective, one of the biggest advantages was the quick relief without the need for surgery. The injections helped break the pain cycle and relax tense muscles. Additionally, they served as a bridge to longer-term therapies like physical rehabilitation and lifestyle adjustments, which are crucial for sustained recovery.
Are There Risks or Limitations I Should Know?
As with any medical procedure, there are potential risks such as infection or allergic reactions, though these are rare. My doctor explained that trigger point injections are most effective when combined with physical therapy and proper ergonomics. For persistent or complex cases, consulting an experienced orthopedic specialist is essential. For more detailed insights, I recommend checking out authoritative sources like the American Academy of Orthopaedic Surgeons.
How Can I Decide if Trigger Point Injections Are Right for Me?
Deciding on this treatment depends on your specific condition, pain severity, and overall health. I suggest discussing thoroughly with your orthopedic doctor and considering additional options like non-surgical therapies or advanced interventions. Remember, personalized care is key to effective pain management.
If you’re exploring options for chronic muscle pain, I encourage you to share your experiences or ask questions below. Your journey might inspire someone else to seek relief and regain their quality of life.
Are Cutting-Edge Orthopedic Treatments the Future of Chronic Spinal Pain Management?
Chronic back and neck pain are complex conditions that often require a nuanced approach beyond traditional therapies. As an orthopedic specialist deeply involved in innovative care, I’ve seen firsthand how emerging treatments are transforming patient outcomes. For example, minimally invasive procedures like advanced spinal injections and regenerative therapies offer promising avenues for sustained relief, especially when combined with personalized rehabilitation plans.
The Role of Precision Diagnostics in Tailoring Effective Treatments
Accurate diagnosis is foundational to effective treatment. Advanced imaging techniques, such as high-resolution MRI and diagnostic ultrasound, enable clinicians to pinpoint the exact source of pain, whether it’s a herniated disc, nerve compression, or facet joint degeneration. This precision ensures that interventions like targeted injections or surgical procedures are directed precisely where they’re needed, enhancing success rates. For comprehensive diagnostic options, I recommend exploring orthopedic diagnostic imaging.
Are Non-Surgical Innovations Sufficient for Severe Cases?
While surgery remains a vital option for certain conditions, non-surgical innovations are rapidly closing the gap. Spinal decompression therapy, for example, utilizes gentle traction to relieve nerve pressure without invasive measures. Additionally, regenerative medicine techniques like platelet-rich plasma (PRP) injections aim to stimulate tissue repair, reducing inflammation and promoting healing naturally. These approaches are especially appealing for patients seeking alternatives to traditional surgery, and ongoing research continues to expand their efficacy. To learn more about non-invasive options, visit minimally invasive back pain treatments.
How Do Regenerative Therapies Complement Surgical Interventions?
Regenerative therapies are increasingly being integrated into comprehensive treatment plans. For patients who undergo spinal fusion or discectomy, post-operative regenerative injections can enhance healing, reduce scar tissue formation, and restore function more quickly. Moreover, these therapies may decrease the likelihood of future degenerative changes by fostering healthier tissue regeneration. This holistic approach underscores the importance of a multidisciplinary strategy, combining surgical, regenerative, and rehabilitative expertise for optimal outcomes. For post-surgical rehab insights, check out rehabilitation after lumbar fusion.
Why Is Personalized Care Essential in Orthopedic Pain Management?
Every patient’s anatomy, pain pattern, and functional goals are unique. Personalized treatment plans that incorporate patient-specific factors—such as lifestyle, comorbidities, and activity level—are crucial for success. This approach often involves a combination of therapies, including physical therapy, medication management, and minimally invasive procedures tailored precisely to the individual. Engaging with specialized professionals who understand the latest advancements ensures that care remains both effective and adaptable. If you’re considering your options, consult with trusted orthopedic spine specialists for expert guidance.
For anyone interested in the latest developments in orthopedic care, I encourage sharing your experiences or asking questions below. Learning from others’ journeys can sometimes reveal new pathways to relief and recovery.
Beyond the Surface: The Subtle Art of Targeting Myofascial Pain
When I first experienced the relief from trigger point injections, I underestimated the intricate anatomy and the precision required. Over time, I realized that each trigger point is a unique nexus of muscular tension and nerve signaling. My journey led me to appreciate the importance of advanced diagnostic tools, such as high-resolution ultrasound, which allow clinicians to identify these tender spots with remarkable accuracy. This precision not only enhances the efficacy of the injections but also minimizes discomfort and potential complications.
The Nuanced Role of Medication in Trigger Point Therapy
Initially, I believed that the injections were merely numbing agents. However, I discovered that the choice of medication—whether local anesthetics, corticosteroids, or combining both—significantly influences outcomes. For example, corticosteroids can reduce inflammation within the muscle, promoting longer-lasting relief, especially in chronic cases. My experience underscores the necessity for personalized medication protocols, tailored to the patient’s specific pathology and response, which is a testament to the evolving sophistication in pain management strategies.
Integrating Trigger Point Injections into a Holistic Pain Management Plan
While the injections provided immediate relief, I found that their true value emerged when integrated into a broader, multidisciplinary approach. Physical therapy, ergonomic adjustments, and mindfulness practices synergize with injections to foster sustained healing. I also learned that patient education about muscle mechanics and posture is crucial; understanding the root causes of myofascial pain prevents recurrence and empowers patients to participate actively in their recovery.
What Are the Limitations and Future Directions in Trigger Point Therapy?
Despite their benefits, trigger point injections are not a panacea. Some myofascial pain syndromes are resistant, requiring repeated interventions or alternative therapies. Emerging research suggests promising avenues, such as regenerative medicine techniques like platelet-rich plasma (PRP) injections, which aim to repair damaged tissues at a cellular level. These innovations could revolutionize how we approach stubborn cases, moving from symptomatic relief to actual tissue healing. According to a recent review in the Journal of Pain Research, integration of regenerative therapies with traditional injections might hold the key to long-term solutions.
How Personal Experience Shapes My Perspective on Pain Management Choices
Having navigated the complexities of chronic muscle pain firsthand, I believe that personalized care remains the cornerstone of effective treatment. Each patient’s anatomy, pain triggers, and lifestyle are unique, necessitating a tailored approach that considers both immediate relief and long-term wellness. This philosophy guides my recommendations and deepens my appreciation for ongoing innovations in orthopedic and pain management fields. I encourage fellow patients and practitioners to share their stories and insights, fostering a community of learning and mutual support. If you’ve had similar experiences or questions, please consider commenting below or exploring further at orthopedic rehabilitation.
Refining the Art of Precision in Trigger Point Therapy
My ongoing exploration into trigger point injections has revealed that the key to maximizing their efficacy lies in the meticulous application of advanced diagnostic techniques. Utilizing high-resolution ultrasound and diagnostic electromyography, I’ve learned that pinpointing the exact location of myofascial trigger points can significantly enhance pain relief outcomes. This meticulous approach minimizes tissue trauma and reduces the need for repeated interventions, aligning with emerging best practices endorsed by leading orthopedic research, such as the detailed findings published in the Journal of Pain Research.
Integrating Regenerative Medicine for Sustainable Relief
While traditional trigger point injections provide immediate relief, the future of pain management is moving toward regenerative therapies that promote long-term tissue healing. Platelet-rich plasma (PRP) and stem cell injections are gaining traction as adjuncts to conventional treatments, aiming to restore muscle and connective tissue integrity at a cellular level. My personal experience with these modalities has shown promising results, especially in cases resistant to standard therapies. This integrative approach exemplifies how a multidisciplinary strategy can transform patient outcomes, emphasizing the importance of personalized treatment plans tailored to individual tissue repair needs.
What Are the Next Frontiers in Non-Invasive Spinal Care?
Advances in non-invasive spinal therapies are opening new horizons for patients seeking alternatives to surgery. Techniques such as spinal decompression therapy, combined with targeted physiotherapy and digital health monitoring, are proving effective in managing complex cases of herniated discs and nerve compression. These innovations are supported by recent clinical trials demonstrating improved functional outcomes and reduced reliance on opioids or invasive procedures. For a comprehensive overview of cutting-edge treatments, visit minimally invasive back pain treatments.
How Does Personalized Orthopedic Care Elevate Patient Outcomes?
Recognizing that no two patients are alike, personalized care strategies incorporate detailed genetic, biomechanical, and lifestyle assessments. Utilizing sophisticated imaging and biomechanical modeling, clinicians can craft tailored intervention plans that address root causes rather than just symptoms. This patient-centric approach not only enhances immediate pain relief but also promotes long-term spinal health, reducing the risk of recurrence. For insights into building such personalized treatment frameworks, consider exploring orthopedic spine specialist selection.
How Can I Leverage Advanced Diagnostic Tools for Better Outcomes?
Incorporating cutting-edge diagnostics, such as functional MRI and 3D motion analysis, allows for an in-depth understanding of individual biomechanics and pain generators. These tools facilitate precise targeting of interventions like injections or minimally invasive surgeries, leading to faster recovery and enhanced function. If you’re interested in how these technologies can be integrated into your treatment plan, I recommend consulting with top specialists through resources like top orthopedic spine specialists.
Feel free to share your experiences or ask questions about these innovative approaches. Your insights might inspire others to pursue more personalized and effective pain management strategies, transforming their journey toward recovery.
Things I Wish I Knew Earlier (or You Might Find Surprising)
The Hidden Power of Precision
One thing I underestimated was how crucial precise localization is for trigger point injections. Using advanced imaging like ultrasound made all the difference in my recovery, ensuring the medication hit exactly where it was needed and minimizing discomfort.
The Role of Personalization
Every person’s muscle pain is unique, and tailored treatment plans truly work better. My experience taught me that discussing all my symptoms openly with my doctor led to more effective, personalized care.
Beyond Immediate Relief
I used to think trigger point injections were just quick fixes, but I’ve come to realize they’re part of a bigger picture—when combined with physical therapy and lifestyle adjustments, they can lead to lasting improvements.
The Importance of Follow-Up
One surprising insight was how critical ongoing follow-up is. Regular check-ins help adapt the treatment plan, ensuring sustained relief and preventing recurrence of the pain.
Risks Are Rare but Real
While complications are uncommon, understanding potential risks made me more confident in my decision. Choosing experienced practitioners reduces these risks significantly.
Future of Pain Management
Emerging therapies like regenerative medicine are promising. They’re not just about symptom relief but about repairing damaged tissues for long-term health, which excites me about the future of pain treatment.
Resources I’ve Come to Trust Over Time
American Academy of Orthopaedic Surgeons
This organization provides comprehensive, trustworthy information on orthopedic treatments, which helped me understand the broader context of trigger point therapy.
National Institutes of Health (NIH)
NIH research articles offered insights into new regenerative techniques and ongoing studies, giving me confidence in emerging therapies.
Peer-Reviewed Journals like the Journal of Pain Research
These publications keep me updated on the latest scientific findings, ensuring I make informed decisions about my care.
My Orthopedic Specialist
Personal guidance from my doctor was invaluable—trustworthy, tailored, and based on the latest evidence.
Patient Support Groups
Sharing experiences with others who underwent trigger point injections helped me learn practical tips and stay motivated during recovery.
Parting Thoughts from My Perspective
Exploring trigger point injections opened a new chapter in my journey toward pain relief. The combination of precision, personalization, and emerging regenerative therapies offers hope for many. If you’re considering this treatment, I encourage you to consult with experienced specialists and ask plenty of questions. Remember, every pain story is unique, and finding the right approach can truly transform your quality of life. If this resonated with you, I’d love to hear your thoughts or experiences—sharing our stories might help others find relief and hope. Feel free to reach out or explore more about innovative treatments at this resource.