Unlocking the Secrets of Nerve Compression: An Orthopedic Perspective
Experiencing persistent numbness, tingling, or sharp pain can often signal nerve compression, a condition that profoundly affects daily function and quality of life. Orthopedic treatment for nerve compression is a nuanced journey, blending advanced diagnostics and personalized therapies to restore nerve health and mobility. Understanding what to expect can empower patients to navigate this complex terrain with confidence and hope.
Beyond the Basics: How Orthopedic Experts Diagnose Nerve Compression
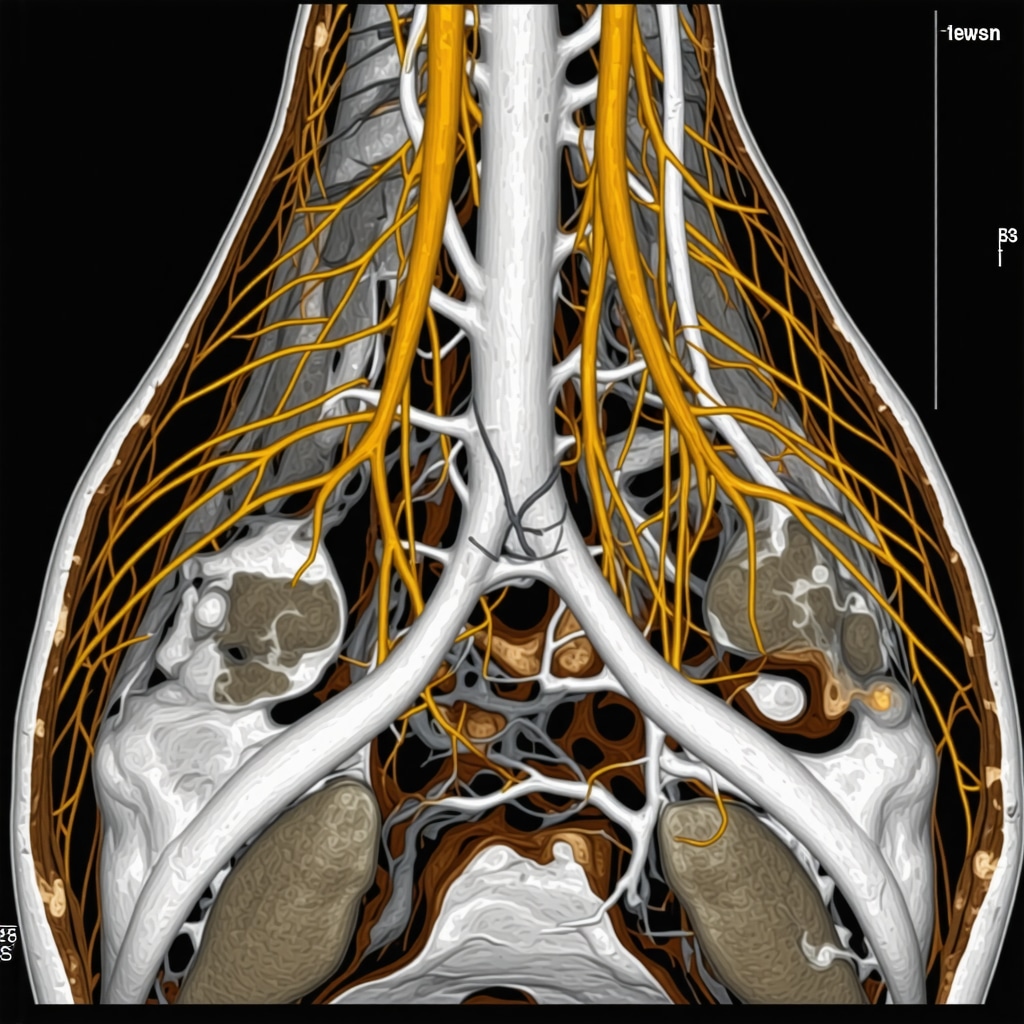
Diagnosis starts with a comprehensive clinical evaluation, where orthopedic specialists carefully assess symptoms and physical signs indicative of nerve entrapment. This often includes provocative maneuvers to reproduce symptoms and pinpoint the compression site. To deepen the insight, electromyography (EMG) and nerve conduction studies (NCS) are employed, providing objective data on nerve function and damage severity. These tests are pivotal, as explained in this authoritative guide on orthopedic nerve tests, offering a scientific backbone to clinical impressions.
Innovative Orthopedic Treatments: From Conservative Care to Surgical Solutions
Initial treatment typically favors non-invasive approaches. Orthopedic specialists often recommend targeted physical therapy designed to relieve pressure on the compressed nerve, improve posture, and strengthen supportive musculature. Adjunctive therapies such as corticosteroid injections can provide symptomatic relief by reducing inflammation around the nerve. For cases resistant to conservative measures, minimally invasive surgical options may be considered, aiming to decompress the nerve while minimizing tissue disruption. Exploring these surgical avenues is crucial, and patients can learn more about the latest techniques in minimally invasive back pain treatments.
What Does Recovery Look Like? Navigating the Path to Nerve Healing
Recovery from nerve compression treatment is highly individualized and may span weeks to months. Orthopedic rehabilitation often involves carefully supervised exercises to restore nerve glide and prevent scar tissue formation. Patients are encouraged to maintain ergonomic practices and adhere to activity modifications to avoid re-compression. Regular follow-up visits allow for monitoring progress and adjusting treatment plans as needed, ensuring an optimal recovery trajectory.
How Can Patients Optimize Outcomes After Orthopedic Nerve Compression Treatment?
Active patient participation is a cornerstone of successful recovery. Embracing prescribed physical therapy, adhering to lifestyle adjustments, and promptly communicating any new or worsening symptoms can dramatically improve outcomes. Moreover, seeking care from orthopedic specialists with expertise in nerve compression, as outlined in resources like nerve compression treatment: when to seek expert care, ensures access to cutting-edge interventions tailored to individual needs.
Have you or someone you know faced nerve compression challenges? Share your experiences or questions below to foster a community of support and knowledge sharing.
Listening to Your Body: Recognizing Subtle Signs Before It’s Too Late
In my experience, the early signs of nerve compression can be so subtle that they easily get overlooked. I remember the first time I noticed a slight tingling in my fingers after long hours at the desk. At first, I brushed it off as fatigue, but over time, the numbness crept in, and simple tasks became uncomfortable. It was only after discussing with my orthopedic specialist that I realized these were red flags indicating nerve entrapment. This personal journey reminded me how crucial it is to pay close attention to consistent symptoms and seek timely evaluation before damage progresses.
Customized Orthopedic Strategies: Why One-Size Doesn’t Fit All
What struck me during my treatment was how orthopedic care goes beyond a generic approach. My specialist tailored a therapy regimen that combined nerve gliding exercises, posture correction, and anti-inflammatory techniques suited specifically to my lifestyle. It’s enlightening how modern orthopedic interventions consider each patient’s unique anatomy and daily habits, a point emphasized in expert guidelines on when to seek specialized care. This personalized care maximized my recovery and minimized downtime, making me appreciate the art behind orthopedic science.
What Are the Most Effective Lifestyle Changes to Support Nerve Health?
This question often comes up among friends and readers curious about proactive steps. From my experience and supported by data from the American Academy of Orthopaedic Surgeons, simple modifications such as ergonomic workspace setups, regular breaks to stretch and move, and avoiding repetitive strain can significantly reduce the risk of worsening nerve compression. Additionally, maintaining a healthy weight and staying hydrated help nourish nerves and surrounding tissues. These practical lifestyle adjustments are empowering tools that complement formal treatment and promote long-term spine and nerve health.
For anyone navigating nerve compression or interested in learning more about orthopedic approaches, feel free to share your stories or questions below. Engaging with others who understand can make the journey less daunting and more hopeful.
Decoding Complex Nerve Compression Patterns: When Multiple Sites Complicate Diagnosis
In clinical practice, nerve compression is rarely straightforward. Patients may present with multifocal entrapments—simultaneous compression at different anatomical points such as cervical radiculopathy combined with carpal tunnel syndrome. This overlapping pathology complicates both diagnosis and treatment planning, requiring an integrative approach that combines advanced imaging modalities like high-resolution ultrasound and MRI neurography alongside electrophysiological testing. These tools unveil subtle nerve abnormalities and differentiate primary from secondary compression sites, allowing orthopedic specialists to customize interventions with precision.
How Do Orthopedic Specialists Differentiate Between Multifocal Nerve Compression Syndromes?
Discerning multifocal nerve entrapments demands a synthesis of clinical acumen and cutting-edge diagnostics. Orthopedic experts perform detailed neurological examinations focusing on sensory distribution and motor weakness patterns. Electromyography (EMG) and nerve conduction studies (NCS) are indispensable, providing quantitative data on conduction block locations and severity. Recent advancements include dynamic ultrasound assessment, which visualizes nerve mobility and compression during provocative maneuvers, as detailed in this peer-reviewed study on ultrasound in nerve entrapment. Such comprehensive evaluation ensures targeted therapies, minimizing unnecessary procedures and optimizing patient outcomes.
Integrating Regenerative Medicine: The Frontier of Orthopedic Nerve Repair
Beyond conventional decompression, regenerative medicine is revolutionizing nerve compression treatment paradigms. Techniques like platelet-rich plasma (PRP) injections and stem cell therapies aim to enhance nerve regeneration and reduce inflammation at the cellular level. Although still emerging, clinical trials demonstrate promising results in accelerating functional recovery and reducing neuropathic pain. Orthopedic specialists now increasingly incorporate these biologics alongside physical rehabilitation, particularly in refractory cases, heralding a new era of personalized nerve healing strategies.
Biomechanical Innovations: Ergonomic Solutions That Complement Orthopedic Care
Addressing the biomechanical contributors to nerve compression extends beyond the clinic. Customized ergonomic interventions—ranging from adjustable workstations to wearable posture sensors—play a pivotal role in sustained symptom relief and prevention. Recent developments include smart devices that provide real-time feedback on posture and repetitive motion patterns, empowering patients to self-correct behaviors that exacerbate nerve stress. Coupling these innovations with orthopedic guidance creates a holistic framework for long-term nerve health preservation.
What Emerging Technologies Are Shaping Orthopedic Management of Nerve Compression?
Emerging technologies such as 3D gait analysis and motion capture systems enable detailed assessment of patient biomechanics, revealing compensatory patterns that may contribute to nerve compression. Additionally, advances in wearable electromyographic sensors facilitate continuous monitoring of muscle activation, offering data-driven insights to refine rehabilitation protocols. These tools, combined with telemedicine platforms, enhance accessibility to expert orthopedic care, fostering proactive and personalized treatment plans.
For a deeper dive into how these advanced diagnostics and therapies transform nerve compression management, explore our comprehensive expert resources or connect with a specialist to tailor your care journey.
Decoding Double Trouble: The Challenge of Multifocal Nerve Compression in Orthopedics
Multifocal nerve compression represents a sophisticated diagnostic puzzle, wherein multiple anatomical sites simultaneously exert pressure on different nerve segments. This complexity demands an integrative orthopedic approach combining detailed clinical evaluation with advanced imaging and electrophysiological studies. High-resolution ultrasound and MRI neurography unveil subtle nerve pathologies, while electromyography (EMG) and nerve conduction studies (NCS) quantify functional impairment, enabling precise localization of each compression site. This layered strategy ensures tailored interventions that minimize unnecessary surgeries and optimize patient-specific outcomes.
How Do Orthopedic Specialists Differentiate Between Multifocal Nerve Compression Syndromes?
Distinguishing multifocal entrapment syndromes requires a confluence of expert neurological examination and sophisticated diagnostic tools. Orthopedic clinicians analyze sensory and motor deficits correlating to specific nerve distributions, while dynamic ultrasound assessments provide real-time visualization of nerve mobility during provocative maneuvers. Such techniques, as elucidated in this peer-reviewed publication on ultrasound applications in nerve entrapment, enhance diagnostic accuracy and refine treatment planning.
Harnessing Regenerative Medicine: Pioneering Cellular Therapies in Nerve Repair
Regenerative medicine is rapidly reshaping orthopedic strategies for nerve compression, introducing biologics that stimulate intrinsic healing mechanisms. Platelet-rich plasma (PRP) injections deliver concentrated growth factors to the injury site, promoting angiogenesis and neurogenesis, while mesenchymal stem cell therapies offer potential to modulate inflammation and support axonal regeneration. Despite their nascent status, emerging clinical trials report accelerated functional recovery and analgesia, positioning these modalities as promising adjuncts in refractory cases.
Biomechanical and Technological Synergy: The Future of Orthopedic Nerve Compression Management
Advanced biomechanical assessments and wearable technologies are transforming how orthopedic care addresses nerve compression. Customized ergonomic solutions, including adjustable workstations and posture-correcting wearables, empower patients to mitigate biomechanical stressors. Furthermore, innovations such as 3D gait analysis and continuous electromyographic sensors deliver granular data on movement and muscle activation patterns, enabling clinicians to tailor rehabilitation with unprecedented precision. Integration with telemedicine platforms further democratizes access to expert guidance, fostering proactive management and sustained nerve health.
What Emerging Technologies Are Shaping Orthopedic Management of Nerve Compression?
Cutting-edge tools such as motion capture systems and wearable EMG sensors provide continuous, objective insights into neuromuscular function, facilitating dynamic adjustments in therapy. Telehealth consultations leverage these data streams for remote monitoring and personalized care adjustments. For comprehensive understanding, the National Center for Biotechnology Information offers extensive literature on these innovations, underscoring their clinical impact.
To deepen your expertise on these advanced diagnostic and therapeutic modalities, consider consulting with an orthopedic specialist proficient in nerve compression management. Engaging with these pioneering approaches can markedly enhance your recovery trajectory and quality of life.
Frequently Asked Questions (FAQ)
What are the earliest signs of nerve compression that I should be aware of?
Early signs often include subtle tingling, numbness, or mild pain in the affected area, which may initially appear intermittently. These symptoms can progress to persistent discomfort, muscle weakness, or loss of coordination if untreated. Recognizing these early symptoms and seeking prompt orthopedic evaluation is crucial to prevent permanent nerve damage.
How do orthopedic specialists differentiate between single-site and multifocal nerve compression?
Orthopedic specialists use a combination of detailed neurological examinations, electromyography (EMG), nerve conduction studies (NCS), and advanced imaging such as high-resolution ultrasound and MRI neurography. These tools help localize the exact sites of nerve entrapment by evaluating sensory and motor deficits, nerve conduction velocity, and dynamic nerve behavior during movement, enabling precise diagnosis of multifocal compression syndromes.
What conservative treatments are most effective before considering surgery for nerve compression?
Conservative management typically includes targeted physical therapy focusing on nerve gliding exercises, posture correction, and muscle strengthening. Additionally, corticosteroid injections may reduce inflammation around the nerve. Ergonomic adjustments and activity modifications are also vital. These methods often alleviate symptoms and improve function without the need for invasive interventions.
How does regenerative medicine contribute to nerve compression treatment?
Regenerative medicine introduces biologic therapies such as platelet-rich plasma (PRP) and mesenchymal stem cell injections that promote nerve healing at the cellular level by stimulating angiogenesis, neurogenesis, and reducing inflammation. While still emerging, these treatments show promise in accelerating recovery and reducing neuropathic pain, especially in cases refractory to conventional therapies.
What lifestyle changes can support long-term nerve health and prevent recurrence?
Maintaining ergonomic work environments, taking regular breaks from repetitive tasks, practicing good posture, staying physically active, keeping a healthy weight, and ensuring proper hydration all support nerve health. These lifestyle modifications reduce biomechanical stress on nerves and complement medical treatments to sustain long-term functional improvements.
Are there any new technologies that help monitor and manage nerve compression at home?
Yes, wearable posture sensors, electromyographic (EMG) devices, and smart ergonomic tools provide real-time feedback on posture and muscle activity. Combined with telemedicine platforms, these technologies allow ongoing monitoring and personalized adjustments to therapy, empowering patients to proactively manage their condition outside the clinical setting.
How long does recovery typically take after surgical decompression of a compressed nerve?
Recovery duration varies widely depending on the nerve involved, severity of compression, and individual patient factors. It generally ranges from several weeks to a few months. Postoperative rehabilitation including physical therapy is essential to restore nerve glide, strength, and function, and to minimize scar tissue formation that could impede recovery.
When should someone seek expert orthopedic care for nerve compression symptoms?
If symptoms such as numbness, tingling, or weakness persist beyond a few weeks, worsen, or interfere with daily activities, prompt evaluation by an orthopedic specialist is recommended. Early intervention improves outcomes by preventing irreversible nerve damage and tailoring treatment to individual needs.
Can nerve conduction studies (NCS) and electromyography (EMG) definitively diagnose nerve compression?
While NCS and EMG are invaluable diagnostic tools providing objective measures of nerve function and identifying conduction blocks, they are most effective when combined with clinical examination and imaging. These studies help localize the site and severity of compression but must be interpreted within the broader clinical context for accurate diagnosis.
What role do ergonomic interventions play alongside orthopedic treatment?
Ergonomic modifications reduce repetitive strain and biomechanical stress on nerves. Adjustable workstations, posture-correcting devices, and education on proper body mechanics complement medical and surgical treatments by preventing re-compression and promoting sustained nerve health.
Trusted External Sources
- American Academy of Orthopaedic Surgeons (AAOS) – Provides comprehensive clinical guidelines and patient education on nerve compression syndromes and orthopedic treatment modalities, serving as a foundational reference for evidence-based care.
- National Center for Biotechnology Information (NCBI) – Hosts peer-reviewed research articles on advanced diagnostic techniques like high-resolution ultrasound and emerging regenerative therapies, facilitating access to cutting-edge scientific evidence.
- Journal of Orthopaedic Research – Offers in-depth studies on biomechanics, nerve injury, and innovative treatment approaches, contributing to the understanding of pathophysiology and therapeutic advancements in nerve compression.
- International Society for Stem Cell Research (ISSCR) – Provides insights and updates on regenerative medicine applications including stem cell therapies relevant to nerve repair and orthopedic interventions.
- Ergonomics Society Publications – Delivers specialized knowledge on ergonomic solutions and biomechanical assessments, supporting integration of technological innovations into nerve compression management.
Conclusion
Effective management of nerve compression demands a sophisticated orthopedic approach that blends meticulous diagnosis, personalized treatment plans, and integration of emerging technologies. Early recognition of subtle symptoms, comprehensive evaluation using electrophysiological and imaging modalities, and tailored conservative or surgical interventions underpin optimal recovery. The advent of regenerative medicine and biomechanical innovations heralds a new frontier in nerve repair and long-term health preservation. Empowering patients through education, lifestyle modification, and advanced monitoring tools further enhances outcomes. By embracing these multifaceted strategies, both clinicians and patients can navigate the complexities of nerve compression with confidence and achieve meaningful restoration of function and quality of life. Share your experiences or questions to foster a knowledgeable community, and explore our expert resources to deepen your understanding of orthopedic nerve compression care.


I found the breakdown of diagnostics and the reminder that symptoms can be subtle really helpful. A year ago I ignored intermittent tingling in my ring and little finger until handwriting and buttoning shirts got harder. My orthopedic team used EMG/NCS to confirm ulnar entrapment, and that objective data made the difference in choosing treatment. My PT focused on nerve‑gliding drills, posture work for my desk setup, and gradual strengthening — combined with a nighttime splint and a single corticosteroid injection, I improved over about ten weeks without surgery. Two practical things that helped: (1) scheduled 5‑minute movement breaks every 45 minutes, and (2) swapping my mouse for a vertical design to reduce wrist rotation. The article’s section on multifocal compression resonated too — I was worried about overlapping issues until imaging and tests clarified the culprit. I’m curious: has anyone tried regenerative options like PRP for persistent symptoms, or adopted wearable posture sensors during recovery? If so, did they change your rehab plan or outcomes?
This post really emphasizes how critical early detection and personalized treatment are for nerve compression issues. I’ve seen firsthand how subtle symptoms like mild tingling or slight weakness can escalate if neglected, leading to more invasive interventions. I recently read about the promising results of regenerative therapies like PRP in nerve recovery, especially for cases resistant to conventional treatments. Has anyone had experience with PRP or stem cell injections as part of their recovery process? I wonder how these biologics compare in effectiveness and safety to traditional surgery or conservative approaches. It’s clear that emerging technologies, including wearable sensors and advanced imaging, are revolutionizing diagnosis and management. I’d love to hear some success stories or advice from those who have incorporated regenerative medicine into their treatment plans—do they truly accelerate healing or improve long-term function? Also, with the increasing availability of smart posture devices, do you find they significantly help in maintaining nerve health post-treatment or prevention? These innovations make me optimistic about future outcomes for nerve entrapment sufferers.