Unraveling the Complexities of Nerve Compression: Why Timing Matters
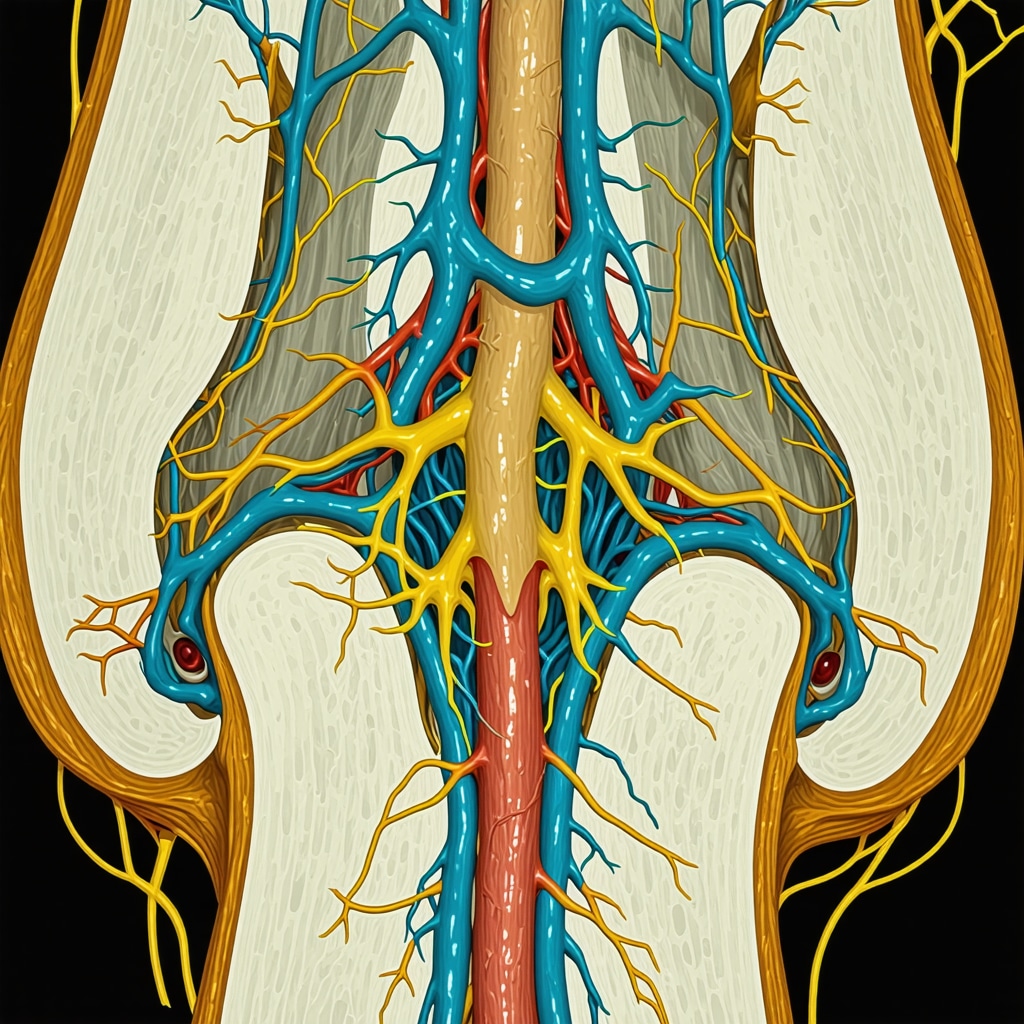
Nerve compression, often manifesting as persistent numbness, tingling, or sharp pain, is more than just a fleeting discomfort. It represents a complex interplay between the musculoskeletal system and neural pathways that, if left untreated, can lead to irreversible damage. Understanding when to seek expert orthopedic treatment is crucial not only for symptom relief but also for preventing long-term functional impairment.
Decoding the Signs: When Does Nerve Compression Demand Orthopedic Expertise?
Early symptoms of nerve compression might mimic benign conditions, but certain red flags signal the need for immediate evaluation by an orthopedic specialist. These include progressive weakness, loss of coordination, or persistent pain unresponsive to conservative management. Recognizing these signs early can be the difference between simple non-surgical interventions and more invasive procedures.
What are the key indicators that my nerve compression requires advanced orthopedic care?
Patients often ask this critical question. Advanced care becomes necessary when symptoms escalate beyond mild discomfort to include motor deficits, muscle atrophy, or significant sensory loss. Additionally, if daily activities are hindered or there is no improvement after initial treatments such as physical therapy or anti-inflammatory medications, consulting an orthopedic expert is advised. Diagnostic nerve conduction studies (EMG/NCS) are often employed at this stage to precisely localize and quantify nerve impairment, guiding targeted treatment plans (learn more about EMG and NCS testing).
Orthopedic Treatment Modalities: From Conservative to Surgical Interventions
Orthopedic care for nerve compression spans a spectrum of therapies. Initial approaches typically involve physical rehabilitation, ergonomic adjustments, and pharmacologic management to alleviate inflammation and promote nerve healing. For example, tailored physical therapy can improve nerve gliding and reduce mechanical irritation, often yielding significant symptom relief.
However, when conservative measures fail, advanced options such as minimally invasive decompression surgery may be indicated. These procedures aim to relieve pressure on the affected nerve while minimizing tissue disruption, thus accelerating recovery and restoring function. Patients interested in understanding these cutting-edge techniques may explore minimally invasive back pain treatments for relevant insights.
Integrating Orthopedic Wisdom: Real-World Case Illustrations
Consider a middle-aged patient presenting with chronic wrist numbness diagnosed as carpal tunnel syndrome. Initial conservative treatment including splinting and anti-inflammatory drugs provided limited relief. Upon orthopedic consultation, nerve conduction studies confirmed median nerve entrapment severity, prompting a successful endoscopic release surgery that restored hand function.
Such cases underscore the importance of timely expert intervention to tailor treatment plans based on individual pathology and progression, ensuring optimal outcomes.
Empowering Your Health Journey: When and How to Connect with Orthopedic Specialists
If you suspect nerve compression or experience persistent symptoms despite initial remedies, reaching out to a board-certified orthopedic specialist can provide clarity and direction. They offer comprehensive evaluations that integrate clinical examination with advanced diagnostics, crafting personalized treatment strategies.
Explore resources on effective nerve compression orthopedic treatments and consider scheduling a consultation with experts who specialize in nerve-related musculoskeletal disorders.
Have you or someone you know experienced nerve compression symptoms? Share your story or ask questions in the comments below to engage with our orthopedic community.
For further authoritative guidance on nerve compression syndromes, the American Academy of Orthopaedic Surgeons (AAOS) provides in-depth resources and evidence-based treatment protocols (AAOS official site).
Listening to Your Body: The Importance of Early Detection in Nerve Compression
Reflecting on my journey and countless patient stories, one thing stands out: early detection can truly change the trajectory of nerve compression conditions. I remember a patient who initially dismissed occasional tingling in her fingers. By the time she sought orthopedic care, her symptoms had progressed significantly, necessitating more invasive treatment. This experience reinforced for me how vital it is to honor even subtle nerve-related symptoms and pursue timely evaluation.
Orthopedic specialists often recommend monitoring symptom patterns closely and seeking consultation if numbness or pain worsens or becomes persistent. This proactive approach can open doors to effective non-surgical options, sparing many from unnecessary procedures.
Understanding the Nuances: How Personalized Orthopedic Care Makes a Difference
Every nerve compression case is unique. In my practice, I’ve observed that customized treatment plans—based on detailed diagnostics and patient lifestyles—yield the best outcomes. For instance, ergonomic modifications at work combined with targeted physical therapy can dramatically alleviate symptoms in some patients without surgery.
Conversely, others might require advanced interventions like minimally invasive decompression to regain function. The key is integrating medical evidence with individual needs, a principle echoed by the American Academy of Orthopaedic Surgeons (AAOS), which highlights personalized care as a cornerstone of successful orthopedic treatment.
Have you ever wondered how lifestyle changes impact nerve compression recovery?
It’s a question I often get asked. Lifestyle really does play a pivotal role—adjusting activities to reduce repetitive strain, maintaining a healthy weight, and adopting regular exercise routines can support nerve health and enhance recovery. Even small changes can ease nerve pressure and improve blood flow, which is essential for healing.
For those navigating nerve compression, embracing these adjustments alongside professional care creates a powerful synergy for relief and long-term wellness.
Exploring Treatment Pathways: When to Consider Surgical Options
While conservative treatments are effective for many, some patients reach a tipping point where surgery becomes the best path forward. I recall a patient with persistent sciatica who tried physical therapy, medications, and bracing with minimal relief. After thorough evaluation and imaging, we agreed on a surgical decompression, which brought remarkable improvement.
If you’re curious about when surgery might be warranted, resources like our detailed guide on key warning signs to watch for can offer clarity and help you make informed decisions.
Engaging with the Orthopedic Community: Your Experiences Matter
Every patient story enriches our understanding of nerve compression and its treatments. I encourage you to share your experiences or questions below. Whether you’ve tried conservative care, faced surgical decisions, or simply want to learn more, your voice helps others feel less alone on their health journey.
And if you’re interested in exploring more about effective non-surgical options or finding trusted specialists, check out our resources on effective non-surgical care and top orthopedic spine specialists.
Decoding Complex Cases: When Standard Treatments Aren’t Enough
While many nerve compression cases respond well to initial conservative therapies, a subset of patients presents with multifactorial etiologies that challenge conventional treatment paradigms. These complex cases often involve overlapping neuropathies, coexisting musculoskeletal disorders, or systemic conditions such as diabetes mellitus that exacerbate nerve vulnerability. In such scenarios, an advanced orthopedic approach integrates multidisciplinary diagnostics and personalized treatment strategies to optimize outcomes.
For instance, patients exhibiting persistent radicular symptoms despite physical therapy and pharmacologic management may benefit from comprehensive imaging modalities like high-resolution MR neurography. This technique provides detailed visualization of nerve architecture and surrounding soft tissues, enabling precise identification of compression sites and inflammatory changes that standard MRI might miss (Chhabra et al., Radiology, 2019).
Innovative Surgical Techniques: Beyond Traditional Decompression
When surgery is indicated, modern orthopedic specialists leverage minimally invasive and nerve-preserving techniques that reduce operative morbidity and enhance functional recovery. Techniques such as targeted muscle reinnervation (TMR) and nerve transfer surgeries have emerged as transformative options for patients with refractory nerve compression or nerve injury complications. These procedures re-route or restore nerve function, improving motor control and sensory perception beyond what conventional decompression achieves.
Moreover, intraoperative neuromonitoring has become a critical adjunct, allowing surgeons to assess real-time nerve integrity and adjust surgical maneuvers accordingly, thereby minimizing iatrogenic injury.
How Does Advanced Imaging Influence Surgical Decision-Making in Nerve Compression?
Advanced imaging modalities, including diffusion tensor imaging (DTI) and MR neurography, provide unparalleled insights into nerve fiber tract integrity and pathological changes. This information directly influences surgical planning by delineating the extent of nerve damage, identifying focal entrapments, and differentiating between reversible ischemic changes and irreversible fibrosis. Consequently, surgeons can tailor interventions—from conservative decompression to complex nerve reconstruction—based on objective tissue characterization.
Integrating Emerging Therapies: The Role of Regenerative Medicine in Orthopedics
Cutting-edge regenerative approaches, such as platelet-rich plasma (PRP) injections and stem cell therapies, offer promising adjuncts to surgical and conservative treatments. These biologics aim to modulate inflammation, promote axonal regeneration, and improve microcirculation around compressed nerves. Although still evolving, early clinical trials suggest enhanced symptomatic relief and functional improvement when these therapies are integrated within a multidisciplinary orthopedic care framework.
Patients interested in exploring these options should consult with orthopedic specialists experienced in regenerative medicine to assess candidacy and individualized treatment protocols.
Collaborative Care Models: Bridging Orthopedics with Neurology and Pain Management
Complex nerve compression often necessitates a holistic approach involving collaboration among orthopedic surgeons, neurologists, and pain management specialists. This team-based model ensures comprehensive assessment of neuropathic pain mechanisms, electrophysiological abnormalities, and psychosocial factors influencing recovery. For example, integrating neuropathic pain pharmacotherapy with surgical decompression can enhance patient comfort and functional outcomes.
Such interdisciplinary coordination exemplifies modern orthopedic practice’s commitment to personalized, evidence-based care.
Are you facing persistent nerve compression symptoms despite treatment? Consult with a board-certified orthopedic specialist to explore advanced diagnostic and therapeutic options tailored to your unique condition.
Harnessing High-Resolution Imaging: Elevating Diagnostic Precision in Challenging Nerve Entrapments
In cases where traditional diagnostics fall short, advanced imaging modalities like high-resolution MR neurography and diffusion tensor imaging (DTI) have revolutionized the visualization of peripheral nerves. These technologies elucidate subtle structural and functional abnormalities, enabling clinicians to discern entrapment severity and differentiate reversible ischemic changes from permanent fibrosis. This heightened precision informs nuanced treatment decisions that optimize patient outcomes and minimize unnecessary interventions.
How do emerging imaging techniques transform surgical planning for refractory nerve compression?
Emerging imaging techniques provide surgeons with detailed maps of nerve fiber integrity and surrounding tissue pathology. This granular insight allows for tailored surgical approaches, such as selective decompression or nerve transfer procedures, targeting the exact loci of pathology. Consequently, operative strategies become less invasive and more effective, reducing recovery times and improving functional restoration (Chhabra et al., Radiology, 2019).
Regenerative Orthopedics: Integrating Biologics to Enhance Neural Recovery
Regenerative medicine modalities, including platelet-rich plasma (PRP) and mesenchymal stem cell (MSC) therapies, are gaining traction as adjunct treatments for nerve compression syndromes. These biologics facilitate axonal regeneration, modulate local inflammatory cascades, and improve perineural microvascular circulation, thereby accelerating symptom resolution and functional recovery. While clinical evidence continues to evolve, early adopters report promising outcomes when these therapies complement conventional orthopedic interventions.
Multidisciplinary Collaboration: Synergizing Expertise Across Specialties
Addressing complex nerve compression requires seamless integration across orthopedic surgery, neurology, and pain management disciplines. This collaborative framework ensures comprehensive care that encompasses structural correction, electrophysiological evaluation, and pharmacologic modulation of neuropathic pain. Such synergy enhances therapeutic efficacy and patient satisfaction, reflecting a paradigm shift toward holistic, patient-centered orthopedic care.
Engage with our expert community: Are you navigating complex nerve compression challenges? Connect with board-certified orthopedic specialists to explore advanced diagnostics and innovative therapies tailored to your condition.
Frequently Asked Questions (FAQ)
What are the earliest symptoms of nerve compression that should prompt a medical evaluation?
Early symptoms often include intermittent numbness, tingling, or mild pain in the affected area. While these can be subtle, any persistent or worsening symptoms, especially those interfering with daily function, warrant evaluation by an orthopedic specialist to prevent progression.
How do orthopedic specialists diagnose the exact site and severity of nerve compression?
Diagnosis typically involves a combination of clinical examination and advanced diagnostic tests such as electromyography (EMG), nerve conduction studies (NCS), and high-resolution imaging like MR neurography or diffusion tensor imaging (DTI). These modalities help localize the compression and assess nerve integrity for tailored treatment planning.
When is surgical intervention necessary for nerve compression?
Surgery is considered when conservative treatments fail to relieve symptoms, when there is progressive motor weakness, significant sensory loss, or muscle atrophy. Advanced imaging and electrophysiological studies guide the decision and help select the most appropriate surgical technique.
What are the benefits of minimally invasive surgery compared to traditional decompression?
Minimally invasive procedures reduce tissue disruption, decrease postoperative pain, shorten hospital stays, and accelerate functional recovery. They also allow for precise targeting of the compressed nerve segments while preserving surrounding structures.
Can lifestyle modifications really impact recovery from nerve compression?
Absolutely. Ergonomic adjustments, reducing repetitive strain, maintaining a healthy weight, and regular exercise improve nerve gliding and local blood flow, supporting nerve healing and reducing symptom recurrence.
How do regenerative medicine therapies complement conventional orthopedic treatments?
Biologic therapies like platelet-rich plasma (PRP) and stem cells promote nerve regeneration, modulate inflammation, and improve microcirculation around compressed nerves. When integrated with surgical or conservative therapies, they may enhance symptom relief and functional outcomes.
What role does multidisciplinary care play in managing complex nerve compression cases?
Complex cases often require collaboration among orthopedic surgeons, neurologists, and pain specialists to address structural, electrophysiological, and neuropathic pain components comprehensively. This approach ensures personalized and effective treatment strategies.
Are advanced imaging techniques widely available and necessary for all nerve compression patients?
While not necessary for all, advanced imaging such as MR neurography and DTI are invaluable in refractory or complex cases where standard MRI is insufficient. They provide detailed nerve visualization critical for precise surgical planning.
How can I find a qualified orthopedic specialist experienced in nerve compression treatments?
Look for board-certified orthopedic surgeons with subspecialty training in peripheral nerve disorders or spine surgery. Professional organizations like the American Academy of Orthopaedic Surgeons (AAOS) offer directories and resources to locate experts.
Is nerve compression always reversible?
If detected early, many nerve compression syndromes can be effectively treated with full functional recovery. However, prolonged compression may cause irreversible nerve damage, underscoring the importance of timely diagnosis and intervention.
Trusted External Sources
- American Academy of Orthopaedic Surgeons (AAOS) – Provides comprehensive clinical guidelines, patient education materials, and evidence-based treatment protocols specific to nerve compression syndromes, ensuring authoritative orthopedic perspectives.
- Radiology Journal – Chhabra et al., 2019 (MR Neurography in Peripheral Nerve Disorders) – Offers seminal research on high-resolution nerve imaging techniques critical for diagnosing and planning treatment of complex nerve entrapments.
- National Institute of Neurological Disorders and Stroke (NINDS) – Delivers detailed overviews on nerve injuries, electrophysiological testing, and emerging therapies, bridging neurological and orthopedic insights.
- Journal of Orthopaedic Research – Publishes cutting-edge studies on regenerative medicine applications, including platelet-rich plasma and stem cell therapies in orthopedic nerve healing.
- North American Spine Society (NASS) – Provides clinical practice guidelines on surgical and non-surgical management of spine-related nerve compressions, supporting informed decision-making.
Conclusion
Understanding nerve compression from an orthopedic perspective involves recognizing early symptoms, utilizing precise diagnostics, and applying personalized treatment strategies ranging from conservative care to innovative surgical and regenerative options. Timing is paramount—early intervention can prevent irreversible nerve damage and restore optimal function. Advances in imaging and biologic therapies are transforming patient outcomes, while multidisciplinary collaboration ensures comprehensive management of complex cases. Whether you are experiencing mild symptoms or facing refractory nerve compression, consulting a board-certified orthopedic specialist can guide you through evidence-based treatments tailored to your unique condition. Embrace proactive care, share your experiences, and explore our expert resources to empower your journey toward nerve health and functional recovery.
We invite you to share this article, comment with your questions or experiences, and continue exploring related expert content to deepen your understanding of orthopedic nerve compression treatment.


This post really highlights the critical importance of recognizing and addressing nerve compression early. From my experience caring for a family member dealing with carpal tunnel syndrome, I noticed how subtle symptoms like mild tingling and occasional numbness were often ignored until they worsened significantly. It was the delay in seeking expert orthopedic evaluation that led to more invasive interventions later on. What resonated with me here is the emphasis on personalized treatment—how tailored physical therapy combined with ergonomic adjustments can sometimes prevent surgery altogether. I also appreciate the detailed explanation about advanced diagnostic tools like EMG/NCS and high-resolution imaging, which I now understand can make a big difference in planning the right intervention. Given the complexity of nerve compression syndromes, I wonder how others have managed to integrate lifestyle changes effectively alongside professional care to ease their symptoms? Have you found certain ergonomic modifications or exercises particularly helpful in promoting nerve healing and preventing symptom progression? It would be great to hear different approaches people have used since early detection and management seem so crucial for avoiding irreversible nerve damage.
What an informative and comprehensive post! I’ve had personal experience with nerve compression in my neck due to a herniated disc, and I can definitely relate to the importance of early detection. I started noticing subtle tingling and weakness in my hands, but I thought it was just fatigue initially. It wasn’t until I experienced muscle atrophy that I sought medical advice, which led to advanced diagnostics including nerve conduction studies. The timely intervention made a significant difference in my recovery. I appreciate the detailed explanations about when conservative management might fail and the role of surgical options. It made me think about how lifestyle modifications—like ergonomic work setups and regular stretching—can be powerful adjuncts in nerve health. Has anyone found particular exercises or ergonomic tips especially effective in preventing nerve compression from worsening? Sharing personal strategies could be really helpful for others navigating early symptoms or trying to avoid invasive procedures.