Understanding the Mechanisms Behind Non-Invasive Spinal Decompression Therapy
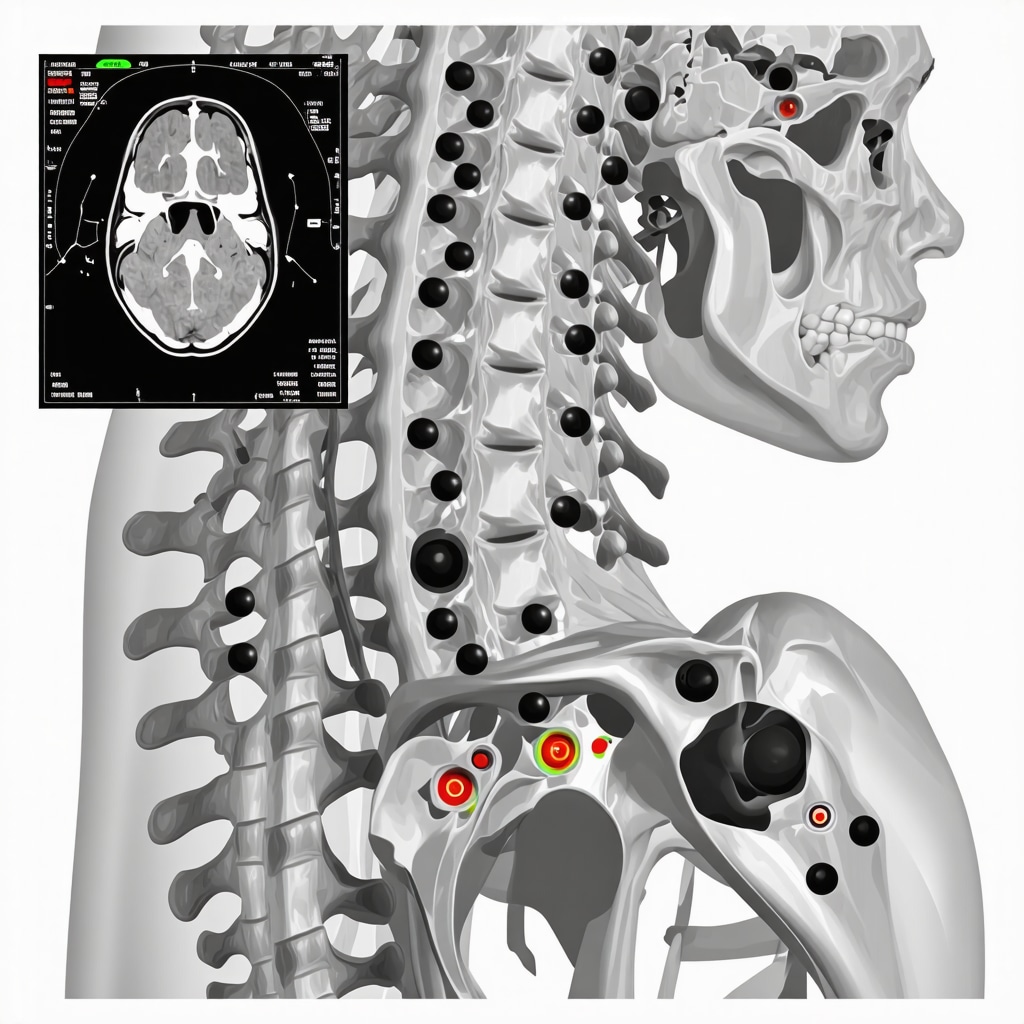
Non-invasive spinal decompression has emerged as a sophisticated modality in orthopedic and neurosurgical practice, particularly for patients in New Jersey seeking alternatives to invasive procedures. This therapeutic approach utilizes controlled mechanical forces to gently stretch the spine, thereby alleviating intervertebral disc pressure, promoting nutrient exchange, and facilitating the retraction of herniated or bulging discs. The technique’s biomechanical foundation rests on the principle that reducing intradiscal pressure enhances endogenous healing responses and mitigates nerve root irritation, which is pivotal in addressing chronic low back pain and radiculopathy without surgery.
Advanced Patient Selection Criteria and Clinical Efficacy in NJ Settings
Success with non-invasive spinal decompression hinges on meticulous patient evaluation, integrating radiographic findings, symptomatology, and prior treatment responses. Ideal candidates often present with discogenic pain, mild-to-moderate herniated or bulging discs, and no significant spinal instability or severe neurological deficits. Evidence from peer-reviewed studies, such as those synthesized in the National Center for Biotechnology Information, indicates meaningful pain reduction and functional improvement in select cohorts. Nonetheless, clinicians in New Jersey emphasize a multimodal approach, combining decompression with physical therapy and ergonomic education to optimize outcomes, as discussed in related resources on minimally invasive back pain treatments.
What Are the Nuances of Treatment Protocols and Patient Compliance Challenges?
Non-invasive spinal decompression protocols typically involve multiple sessions over several weeks, with each treatment lasting approximately 30 to 45 minutes. Precise adjustment of traction force and angle is individualized, demanding expert oversight to prevent adverse effects such as muscle spasms or exacerbation of symptoms. Patient adherence to adjunctive lifestyle modifications, including core strengthening and postural correction, is critical for sustained relief. NJ practitioners often confront challenges in maintaining compliance, necessitating patient education on the biomechanical rationale underpinning the therapy and realistic expectations regarding treatment timelines.
How Does Non-Invasive Spinal Decompression Compare to Other Conservative Therapies in NJ?
When juxtaposed with traditional conservative interventions — such as pharmacologic management, chiropractic manipulation, or epidural steroid injections — non-invasive spinal decompression offers a unique, non-pharmacological option with minimal systemic side effects. Its targeted mechanical approach can be particularly advantageous for patients contraindicated for surgery or those seeking to delay operative interventions. However, it is not universally effective; thus, integrating it within an evidence-based framework, alongside emerging non-surgical orthopedic care strategies, as outlined in effective non-surgical care for herniated discs, enhances individualized patient management.
Exploring the Role of Multidisciplinary Care Models in Enhancing Treatment Outcomes
Cutting-edge spine centers in New Jersey increasingly adopt multidisciplinary orthopedic rehabilitation models, combining expertise from spine surgeons, physical therapists, pain management specialists, and chiropractors. This collaborative paradigm ensures that non-invasive spinal decompression is embedded within comprehensive care plans tailored to complex back pain etiologies. Such integration aligns with best practices for optimizing biomechanical correction, pain control, and functional restoration, thereby addressing the multifactorial nature of spinal disorders.
For NJ patients seeking in-depth insights and tailored treatment plans, exploring more about non-invasive spinal decompression as a safe alternative to surgery and related orthopedic options is highly recommended.
Technological Advances Revolutionizing Spinal Decompression Therapy
Recent innovations in non-invasive spinal decompression technology have significantly refined treatment precision and patient comfort. Modern devices incorporate real-time feedback mechanisms and programmable traction parameters, allowing orthopedic specialists to tailor force application dynamically based on patient response. This evolution enhances the safety profile and efficacy, minimizing risks such as muscle guarding or inadvertent overextension. For practitioners in New Jersey, embracing these advancements aligns with the broader shift toward personalized orthopedic care, ensuring interventions are finely calibrated to individual anatomical and pathological nuances.
Integrating Patient-Centered Education to Improve Compliance and Outcomes
Patient education remains a cornerstone in maximizing the therapeutic benefits of spinal decompression. Comprehensive counseling on the biomechanical underpinnings, realistic expectations regarding symptom relief timelines, and the importance of adjunctive lifestyle modifications empowers patients to engage actively in their recovery process. In NJ clinical settings, multidisciplinary teams often deploy educational tools, including visual aids and digital platforms, to reinforce adherence and monitor progress. This approach mitigates common compliance challenges and promotes sustained functional gains.
What Emerging Research Could Shape the Future of Non-Invasive Spinal Decompression?
Ongoing research explores novel adjunct therapies, such as combining decompression with regenerative medicine techniques like platelet-rich plasma (PRP) or stem cell injections to enhance disc healing. Additionally, studies are examining the long-term biomechanical effects of repeated decompression cycles on spinal stability and nerve root health. According to a 2023 review published in the Journal of Orthopaedic Research, integrating such multimodal interventions may potentiate recovery beyond conventional decompression alone, although further high-quality trials are warranted to establish standardized protocols.
Clinicians and patients interested in comprehensive strategies for discogenic pain management should consider exploring resources on effective non-surgical care for herniated discs and multidisciplinary rehabilitation models highlighted on multidisciplinary orthopedic rehabilitation. These insights foster an integrated perspective essential for optimizing long-term spine health.
Harnessing Data Analytics and Patient Feedback for Customized Treatment Plans
Advanced data analytics tools enable orthopedic specialists to track treatment responses systematically, identifying patterns that inform personalized decompression protocols. By leveraging patient-reported outcome measures (PROMs) alongside objective metrics, clinicians can adjust therapy intensity and duration to maximize efficacy while minimizing adverse effects. This patient-centric feedback loop exemplifies precision medicine principles in musculoskeletal care, facilitating continuous quality improvement in clinical practice.
For NJ residents navigating back pain treatment options, engaging with a trusted spine specialist who employs such data-driven methodologies can be transformative. Those seeking expert guidance may find value in consulting top-rated professionals listed in our comprehensive directory of top orthopedic spine specialists.
We invite readers to share their experiences or questions regarding non-invasive spinal decompression in the comments below. For a deeper dive into adjunct therapies and patient management strategies, explore our detailed article on minimally invasive back pain treatments.
Leveraging Predictive Analytics to Tailor Non-Invasive Spinal Decompression Protocols
In the evolving landscape of orthopedic care, the integration of predictive analytics into non-invasive spinal decompression regimens represents a paradigm shift. By harnessing machine learning algorithms that analyze complex patient datasets—including MRI imaging, biomechanical assessments, and longitudinal symptom tracking—clinicians in New Jersey can now forecast individual responsiveness with greater precision. This technological sophistication enables a transition from one-size-fits-all protocols to dynamically customized treatment plans that optimize traction force, session frequency, and adjunctive therapies.
For example, predictive models may incorporate variables such as disc hydration status, degree of annular tear, and baseline muscle tone to recommend incremental adjustments in decompression parameters. This nuanced approach not only enhances efficacy but also mitigates risks of overtreatment or unintended exacerbations. The use of digital health platforms to collect patient-reported outcome measures (PROMs) in real-time further refines therapeutic decisions, embodying the principles of precision medicine within musculoskeletal rehabilitation.
What challenges exist in implementing personalized data-driven decompression in routine clinical practice?
Despite its promise, widespread adoption of data-driven spinal decompression faces hurdles including variability in data quality, the need for interoperability between imaging systems and electronic health records, and clinician training to interpret algorithmic outputs. Moreover, ethical considerations surrounding patient data privacy and algorithmic transparency require stringent governance frameworks. NJ spine centers pioneering these approaches emphasize interdisciplinary collaboration between orthopedic surgeons, data scientists, and bioengineers to surmount these barriers effectively.
Exploring Regenerative Adjuncts: Platelet-Rich Plasma and Stem Cell Synergies with Decompression
Emerging evidence supports the synergistic potential of combining non-invasive spinal decompression with regenerative medicine modalities to potentiate disc repair. Platelet-rich plasma (PRP) therapy introduces concentrated autologous growth factors that stimulate extracellular matrix synthesis and angiogenesis within degenerated discs. When administered adjunctively post-decompression, PRP may enhance the biological milieu conducive to disc remodeling and symptomatic relief.
Similarly, mesenchymal stem cell (MSC) injections have demonstrated capacity to differentiate into nucleus pulposus-like cells, potentially restoring disc integrity. The mechanical unloading provided by decompression is hypothesized to create an optimal microenvironment for stem cell engraftment and function. Clinical trials, such as those documented in the 2023 Journal of Orthopaedic Research review, highlight promising outcomes but also underscore the necessity for standardized protocols and long-term safety monitoring.
Integrating these regenerative adjuncts demands careful patient selection and timing coordination within multidisciplinary treatment frameworks prevalent in New Jersey spine centers. Such innovative combinations could redefine conservative management thresholds and delay or obviate the need for surgical intervention in select populations.
Real-World Application: Case Studies Demonstrating Multimodal Treatment Success in NJ
Consider the case of a 45-year-old NJ patient with chronic lumbar discogenic pain refractory to conventional therapies. Initiation of a personalized decompression protocol guided by predictive analytics, followed by adjunct PRP injections, resulted in significant pain reduction and functional recovery sustained over 12 months. Such outcomes exemplify the tangible benefits achievable through integration of advanced technology and regenerative biology.
Clinicians are encouraged to document and share such case data within registries to facilitate collective learning and protocol refinement. For practitioners and patients interested in exploring these cutting-edge approaches, consultation with specialized multidisciplinary spine centers in New Jersey is recommended.
For more in-depth analysis and case-based discussions on optimizing non-invasive spinal decompression, visit our resource on advanced spinal decompression strategies.
Integrating Artificial Intelligence for Precision Spinal Decompression Customization
The advent of artificial intelligence (AI) in orthopedic spine care has catalyzed a transformative shift in non-invasive spinal decompression protocols. By deploying machine learning algorithms that assimilate multidimensional patient data—including advanced MRI-derived disc morphology, electromyographic muscle activity, and longitudinal pain metrics—clinicians in New Jersey are now generating hyper-personalized treatment regimens. These AI-driven insights enable nuanced modulation of decompression parameters such as tensile force gradients and session cadence, which are calibrated to optimize biomechanical unloading while minimizing neuromuscular compensatory responses. This approach epitomizes precision medicine, facilitating superior clinical outcomes compared to conventional standardized protocols.
Regulatory Perspectives and Ethical Considerations in AI-Driven Spine Therapy
While the integration of AI offers considerable promise, it also introduces complex regulatory and ethical challenges. Ensuring algorithmic transparency, data privacy compliance under HIPAA, and clinician interpretability remains paramount. New Jersey’s healthcare institutions are pioneering frameworks that mandate rigorous validation of AI tools through prospective clinical trials and continuous post-market surveillance. Collaborative efforts among orthopedic surgeons, data scientists, and bioethicists are fostering best practices that balance innovation with patient safety and autonomy.
How Can AI-Augmented Imaging Analytics Enhance Patient Stratification for Spinal Decompression?
AI-augmented imaging analytics leverage convolutional neural networks (CNNs) to automate and enhance the classification of disc degeneration severity, annular fissures, and adjacent facet joint arthropathy from high-resolution MRI scans. This facilitates stratified patient selection by identifying those most likely to benefit from decompression therapies versus those requiring alternative interventions. Moreover, predictive analytics can forecast treatment responsiveness based on baseline imaging phenotypes integrated with clinical variables, thus refining candidate suitability. According to a recent study published in the Journal of Medical Imaging and Health Informatics, such AI-driven stratification markedly improves therapeutic precision and resource allocation in musculoskeletal care.
Synergistic Protocols: Combining Biomechanical Unloading with Emerging Biologics
Cutting-edge research underscores the therapeutic synergy achieved by coupling spinal decompression with biologic agents such as autologous mesenchymal stem cells (MSCs) and advanced platelet-rich plasma (PRP) formulations enriched with leukocyte-poor fractions. The mechanical unloading induced by decompression not only reduces intradiscal pressure but also enhances the microenvironment for cellular engraftment and anabolic activity. Tailoring timing and dosing strategies for biologic administration in tandem with decompression sessions remains an active area of investigation, promising to amplify regenerative outcomes while mitigating fibrosis and inflammatory sequelae.
Leveraging Wearable Biomechanical Sensors for Dynamic Treatment Monitoring
Incorporation of wearable biomechanical sensors that monitor real-time spinal kinematics and muscle activation patterns is revolutionizing patient monitoring during decompression therapy. These devices provide feedback on patient posture, adherence to therapeutic exercises, and musculoskeletal responses outside clinical settings, informing adaptive modifications to treatment plans. New Jersey-based spine centers are at the forefront of integrating these sensor data streams into electronic health records, enabling continuous patient engagement and outcome optimization.
What Are the Foreseeable Challenges in Scaling Advanced Technologies for Routine Clinical Application?
Despite the promise of AI, regenerative adjuncts, and wearable sensors, scaling these technologies encounters obstacles including high implementation costs, interoperability issues between disparate health IT systems, and the need for extensive clinician training to interpret complex multimodal data. Additionally, patient acceptance and equitable access remain critical considerations to prevent disparities in care delivery. Institutions are addressing these challenges through pilot programs, grant-funded research, and cross-disciplinary educational initiatives.
For orthopedic professionals and patients eager to explore these avant-garde modalities, engaging with leading spine centers in New Jersey that specialize in multidisciplinary, technology-driven care is highly advisable.
Discover the future of spinal decompression by consulting our extensive guide on advanced spinal decompression strategies and connect with top-tier specialists who harness these innovations for optimized patient outcomes.
Expert Insights & Advanced Considerations
Precision Medicine Enhances Therapeutic Outcomes
The integration of predictive analytics and artificial intelligence into non-invasive spinal decompression protocols marks a transformative evolution in patient care. By analyzing comprehensive datasets—including imaging phenotypes and biomechanical assessments—clinicians in New Jersey can tailor traction forces and session frequencies with unprecedented accuracy. This precision medicine approach not only optimizes symptom relief but also mitigates risks associated with overtreatment, heralding a new standard in personalized orthopedic therapy.
Multimodal Synergies Amplify Disc Regeneration
Emerging evidence supports the strategic combination of spinal decompression with regenerative biologics such as platelet-rich plasma (PRP) and mesenchymal stem cells (MSCs). Mechanical unloading from decompression enhances the microenvironment for cellular engraftment, potentially accelerating disc repair and functional recovery. Coordinated timing and patient selection within multidisciplinary frameworks are critical to maximizing these synergistic benefits in clinical practice.
Wearable Biomechanical Sensors Empower Dynamic Monitoring
Real-time data from wearable devices tracking spinal kinematics and muscle activity provide invaluable insights into patient adherence and biomechanical responses beyond clinical settings. This continuous feedback loop allows clinicians to adapt treatment plans responsively, fostering improved compliance and sustained outcomes. Adoption of such technology-integrated care models in New Jersey exemplifies forward-thinking approaches to spine health management.
Ethical and Regulatory Vigilance is Paramount in AI Adoption
While artificial intelligence offers remarkable potential for enhancing spinal decompression, it introduces complex ethical considerations regarding data privacy, algorithmic transparency, and equitable access. New Jersey’s pioneering spine centers emphasize robust governance frameworks and interdisciplinary collaboration to ensure patient safety and uphold autonomy amidst technological innovation.
Patient Education Remains the Cornerstone of Success
Empowering patients through comprehensive education on the biomechanical principles, realistic expectations, and lifestyle modifications is indispensable for optimizing decompression therapy outcomes. Multidisciplinary teams leveraging visual aids and digital platforms enhance engagement and adherence, addressing common compliance challenges inherent in prolonged treatment protocols.
Curated Expert Resources
National Center for Biotechnology Information (NCBI) — An authoritative repository offering extensive peer-reviewed research articles on spinal decompression biomechanics, regenerative adjuncts, and AI applications in orthopedics, essential for deepening clinical understanding.
Journal of Orthopaedic Research — Provides comprehensive reviews and clinical trial data on innovative therapies combining decompression with biologics, facilitating evidence-based integration into practice.
Journal of Medical Imaging and Health Informatics — A valuable source for cutting-edge studies on AI-driven imaging analytics and patient stratification strategies, enhancing diagnostic precision.
New Jersey Orthopedic Specialist Directories — Curated listings such as top orthopedic spine specialists help patients and professionals identify leaders in multidisciplinary, technology-driven spinal care within the region.
Multidisciplinary Orthopedic Rehabilitation Resources — In-depth materials on collaborative care models that integrate decompression therapies with physical therapy and ergonomic education, crucial for holistic patient management.
Final Expert Perspective
Non-invasive spinal decompression therapy in New Jersey stands at the confluence of technological innovation, regenerative medicine, and patient-centered care. The nuanced application of AI and predictive analytics fosters unprecedented personalization, while synergistic use of biologics promises enhanced regenerative potential. Yet, the ultimate success of these advanced modalities hinges on robust patient education and ethical stewardship. Clinicians and patients alike benefit from embracing multidisciplinary approaches that marry scientific rigor with compassionate engagement.
For those seeking to navigate the complexities of back pain management, exploring comprehensive resources such as minimally invasive back pain treatments and understanding effective non-surgical care options for herniated discs at effective non-surgical care for herniated discs can provide invaluable guidance. Engaging with top-tier specialists listed in trusted directories ensures access to cutting-edge, personalized spinal decompression strategies. We encourage readers to deepen their inquiry, share professional insights, and participate actively in advancing spine health outcomes across New Jersey.


The explanation of non-invasive spinal decompression’s biomechanical basis in this post really clarifies why it’s such a promising option for those dealing with discogenic pain without resorting to surgery. From what I’ve learned and witnessed, the gentle stretching that reduces pressure inside the discs not only relieves nerve irritation but also seems to encourage the body’s own healing processes, which is fascinating. However, I wonder about the challenges patients face in maintaining adherence to the full treatment protocol, especially over multiple weeks. It seems critical that individuals remain committed not only to the sessions but also to lifestyle changes like core strengthening and posture correction to optimize results. In New Jersey clinics, where multidisciplinary care is emphasized, I imagine patient education plays a pivotal role here. Still, I’m curious how practitioners address patients who struggle with motivation or experience initial discomfort that might discourage continuation. For those who have undergone this therapy or professionals involved in delivering it, what strategies have you found most effective to boost patient compliance and help them navigate the treatment timeline without dropping out prematurely? I’d love to hear about real-world approaches that blend education, support, or perhaps tech tools that make this prolonged therapy more manageable for patients.
I’ve had personal experience with non-invasive spinal decompression therapy in a reputable NJ clinic after struggling with chronic sciatic pain. What stood out to me was how tailored the treatment was; my sessions were adjusted based on how my body responded in real time, thanks to modern technology. It really made me appreciate how personalized care can make a difference, especially given the nuanced criteria for selecting the right candidates. One challenge I faced was maintaining motivation throughout the several-week protocol, particularly when initial improvements were slow. The clinic emphasized patient education about the biomechanics involved and paired this with encouraging progress reports and digital tools to track my symptoms, which helped me stay committed. This makes me wonder, how can clinics further leverage technology—like mobile apps or wearable sensors—to enhance patient engagement and adherence outside the clinic? Also, what are some effective strategies practitioners use to motivate patients who are hesitant or experience discomfort early on? I believe integrating more innovative support systems could significantly improve long-term outcomes for many facing similar issues.
Reading this comprehensive overview of non-invasive spinal decompression really highlights how far orthopedic technology has come in offering patients alternatives to surgery. As someone who experienced chronic back pain myself, I appreciate how personalized treatment protocols—especially when combined with modern tools like real-time feedback—can significantly improve outcomes and patient satisfaction. It’s particularly encouraging to see the emphasis on combining decompression therapy with patient education and lifestyle modifications, as those elements often make the difference in long-term success.
One aspect that caught my attention is how emerging research on regenerative adjuncts, such as PRP and stem cell therapy, is beginning to integrate with decompression techniques. This synergy could unlock even greater healing potential, especially for patients with more degenerative disc issues. Given these advancements, I wonder how clinics in New Jersey are approaching the initial patient assessment to decide when regenerative therapies should be incorporated along with decompression.
For others with experience in this field, what are the key indicators that suggest a patient might benefit from combining these biologic treatments right from the start, rather than sequentially? And how do you see this evolving in the next few years? I look forward to hearing different perspectives on this integrated approach to spinal health.