My Unexpected Back Pain Saga: When I Knew It Was Time to Seek Expert Help
It all started with a dull ache in my lower back that gradually worsened over a few weeks. Like many, I initially brushed it off, hoping it would resolve on its own. However, when the pain became persistent and started interfering with my daily activities, I realized I needed to consult a specialist. This personal experience prompted me to learn more about the signs indicating when it’s crucial to see an orthopedic spine surgeon.
Recognizing the Warning Signs: My Personal Insights
When Does Back Pain Stop Being Normal and Start Being a Concern?
During my research, I discovered that persistent back pain lasting more than a few weeks is a red flag. For me, the pain persisted despite rest and over-the-counter remedies, signaling that I shouldn’t ignore it. According to experts, if your back pain doesn’t improve with home treatments, it might be time to consult a professional. My experience confirmed that ignoring ongoing pain can lead to worsening conditions.
Additional Signs That Need Medical Attention
Another critical sign I learned about was if the pain radiates down the legs or is accompanied by numbness and weakness. I remember feeling numbness in my leg that didn’t go away, which was alarming. This aligns with recommendations from authoritative sources like the American Academy of Orthopaedic Surgeons, emphasizing that nerve-related symptoms often require specialized evaluation and treatment.
Why I Chose to See a Spine Surgeon: My Reflection
After experiencing these symptoms, I realized that consulting an orthopedic spine surgeon was the best course of action. These specialists are trained to diagnose and treat complex spinal issues, often with minimally invasive procedures that can alleviate pain and restore function. If you find yourself in a similar situation, don’t hesitate to seek expert advice. For more on choosing the right surgeon, I recommend reviewing tips from trusted sources like this guide.
How Can an Orthopedic Spine Surgeon Help You?
From my personal experience, a spine surgeon can identify underlying issues such as herniated discs, spinal stenosis, or degenerative disc disease. These specialists can suggest effective treatment options, including both surgical and non-surgical approaches, tailored to individual needs. If your symptoms resemble mine, it might be time to explore your options with a trusted orthopedic expert.
What Are the Risks of Delaying a Consultation?
Delaying a visit to a spine specialist can sometimes lead to worsening symptoms or permanent nerve damage. I learned that early intervention often results in better outcomes. Remember, your health is worth it—don’t wait until pain becomes unbearable or debilitating.
If you’re experiencing persistent back pain, I encourage you to consult a qualified orthopedic spine surgeon. Feel free to share your experiences or ask questions in the comments—I’d love to hear how others are navigating their back health journey!
Understanding the Nuances of Back Pain: A Deep Dive for Patients
As a seasoned orthopedic spine specialist, I often see patients who dismiss early warning signs of serious spinal conditions. While occasional discomfort is common, persistent or worsening pain warrants a closer look. For instance, my patients frequently ask, “How do I distinguish between normal discomfort and symptoms that require expert intervention?” The answer lies in recognizing specific patterns and associated symptoms that hint at underlying issues like herniated discs, spinal stenosis, or degenerative disc disease, which often demand specialized care. According to a recent comprehensive review by the American Academy of Orthopaedic Surgeons, early diagnosis and timely intervention can significantly improve outcomes.
The Role of Advanced Diagnostic Tools in Accurate Assessment
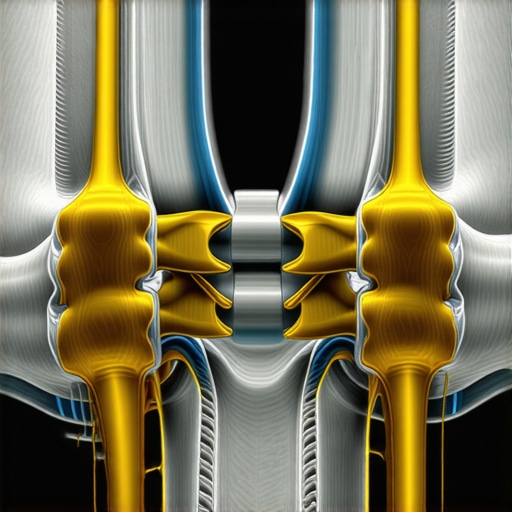
Accurate diagnosis is the cornerstone of effective treatment. Modern imaging techniques such as MRI scans provide detailed views of spinal structures, helping clinicians identify issues that might not be apparent through physical examination alone. For example, nerve compression caused by herniated discs can be precisely localized, guiding targeted interventions. If you’re unsure whether your symptoms merit imaging, consult an orthopedic specialist who can recommend the appropriate diagnostics. Exploring options like orthopedic diagnostic imaging can be a game-changer in your recovery journey.
Can Conservative Treatments Suffice, or Is Surgery Inevitable?
Many patients wonder whether non-invasive therapies can resolve their back issues. While physical therapy, medication, and epidural injections can be effective, they may not always address the root cause if the condition is advanced. As an expert, I emphasize a personalized approach—evaluating the severity of the condition, patient health, and lifestyle factors. For example, minimally invasive procedures like spinal decompression or disc injections offer relief with reduced recovery times compared to traditional surgery. If symptoms persist despite conservative management, surgical options such as lumbar fusion or discectomy should be considered. For more insights into non-surgical treatments, visit this resource.
Understanding When Surgery Becomes the Best Option
Deciding on surgery can be daunting, but sometimes it’s the most effective way to restore function and quality of life. Indicators include progressive neurological deficits, significant nerve compression, or pain that severely limits daily activities. For example, if nerve impingement causes persistent numbness or weakness, delaying surgical intervention may risk permanent damage. As an expert, I advise patients to weigh the risks and benefits carefully, often in consultation with a multidisciplinary team. For tailored advice, I recommend discussing your case with a trusted orthopedic spine surgeon.
What Are the Hidden Factors That Might Influence Your Treatment Success?
Beyond the obvious symptoms, factors such as age, overall health, and previous spinal history play crucial roles in treatment planning. For instance, osteoporosis can complicate surgical procedures, necessitating preoperative management. Moreover, lifestyle modifications, ergonomic adjustments, and ongoing physical therapy are essential for long-term spinal health. To stay informed about advancements in orthopedic care, I recommend regularly checking trusted sources like top spine specialists in 2025.
If you’re uncertain about your symptoms or treatment options, don’t hesitate to reach out to a qualified orthopedic spine specialist. Sharing your experiences or questions in the comments can help others navigate their own back health journeys. Remember, early intervention can make a significant difference—your spine’s health is worth it!
Unveiling the Complexities of Back Pain: My Personal Journey and Deep Reflections
Over the years, I’ve come to realize that back pain is not just a simple discomfort but often a symptom of underlying issues that require a nuanced understanding. My own experience with persistent lower back pain taught me that beneath the surface, there are multiple layers of complexity—ranging from nerve impingements to degenerative changes—that demand careful evaluation and personalized treatment strategies.
Why Do Some Back Pain Symptoms Signal Urgent Attention?
From my professional perspective, I find that many patients underestimate the importance of certain warning signs. For example, I recall a patient who dismissed numbness and weakness as mere fatigue, only to find that delayed intervention led to permanent nerve damage. According to research published in the Global Spine Journal, early recognition of neurological deficits significantly improves recovery chances. Recognizing subtle clues—such as unexplained bowel or bladder dysfunction—can be life-changing, emphasizing the importance of listening to your body and seeking expert advice promptly.
My Deep Dive into Diagnostic Precision and Advanced Imaging
One thing I emphasize to my patients is the critical role of advanced diagnostic tools. MRI scans, for instance, provide unparalleled insights into soft tissue and nerve structures, often revealing issues hidden in plain sight. I’ve seen cases where a detailed MRI uncovered a herniated disc pressing on nerve roots, which was not apparent through physical exam alone. This underscores the importance of choosing a provider who utilizes state-of-the-art imaging techniques—like orthopedic diagnostic imaging—to tailor the most effective treatment plan.
How Do I Weigh Conservative vs. Surgical Interventions in Complex Cases?
Deciding between non-invasive treatments and surgery is a nuanced process. In my practice, I always consider patient-specific factors such as age, activity level, and overall health. While physical therapy, medications, and epidural injections can sometimes resolve symptoms, there are situations where surgical intervention becomes necessary—particularly when nerve compression leads to progressive weakness or loss of function. I’ve observed that minimally invasive procedures, like spinal decompression, often provide relief with shorter recovery times. It’s vital to have an open dialogue with your healthcare provider about the risks and benefits of each approach, especially considering the latest advancements in minimally-invasive back pain treatments.
Delving Deeper: How Precision in Diagnostic Imaging Shapes Surgical Outcomes
Throughout my years of practice, I have witnessed firsthand how advancements in diagnostic imaging, particularly high-resolution MRI and CT scans, revolutionize our ability to pinpoint spinal pathologies with exceptional accuracy. This precision not only guides the surgical approach but also significantly enhances patient prognosis. For instance, in complex cases of nerve root compression, detailed imaging enables surgeons to plan minimally invasive decompression procedures that reduce recovery time and minimize risks. An authoritative study published in the Global Spine Journal underscores that early and detailed imaging correlates strongly with improved functional recovery post-surgery.
Balancing Conservative Management and Surgical Intervention: A Nuanced Approach
My clinical philosophy emphasizes a tailored strategy—evaluating each patient’s unique presentation, comorbidities, and lifestyle. While I advocate for conservative treatments like physical therapy, epidural injections, and medication as first-line options, I recognize their limitations in cases of persistent or progressive neurological deficits. For example, patients with significant disc herniation causing motor weakness often benefit from early surgical intervention to prevent irreversible nerve damage. The decision-making process is complex, requiring a comprehensive assessment and transparent communication with patients about risks, benefits, and expected outcomes. For detailed guidance on this balance, I recommend exploring latest trends in spinal support and stabilization.
How Do I Assess When Surgery Is the Best Course for Long-Term Spinal Health?
In my experience, definitive indicators for surgical intervention include unrelenting pain unresponsive to conservative therapy, neurological deterioration, and structural instability evident in imaging studies. For example, spinal fusion might be warranted in cases of significant spondylolisthesis or multi-level degeneration. I always emphasize a multidisciplinary approach, involving neurologists and pain specialists, to ensure that the decision aligns with the patient’s overall health goals. The critical aspect is timely intervention—delayed surgery can lead to nerve scarring or chronic disability, complicating recovery. If you’re contemplating your options, I suggest consulting with a trusted orthopedic spine surgeon who specializes in advanced surgical techniques.
What Are the Latest Innovations in Minimally Invasive Spine Surgery, and How Do They Improve Outcomes?
In recent years, my practice has integrated innovative minimally invasive techniques such as endoscopic discectomy and percutaneous spinal fusion. These approaches offer several advantages: reduced tissue trauma, shorter hospital stays, and faster return to daily activities. The evolution of specialized surgical tools and real-time imaging guidance has expanded the scope of what can be achieved with less invasive procedures. Studies in the field, including those highlighted in 2025 orthopedic advancements, demonstrate high success rates and patient satisfaction. I encourage patients and practitioners alike to stay informed about these cutting-edge procedures, as they are transforming the landscape of spinal care.
If you’re considering surgical options or seeking a second opinion, I invite you to reach out through our contact page. Engaging in a comprehensive consultation can clarify your treatment pathway, ensuring decisions are made with confidence and clarity. Remember, mastery in spinal care hinges on a combination of precise diagnostics, personalized treatment planning, and embracing technological innovations—each an essential element of my practice and philosophies.
Things I Wish I Knew Earlier (or You Might Find Surprising)
1. Persistent Pain Isn’t Normal
Early on, I thought back pain was just part of life, but I learned that pain lasting more than a few weeks signals that it’s time to seek professional help. Ignoring it can lead to worsening conditions, so listening to your body is crucial.
2. Numbness and Weakness Are Red Flags
Experiencing numbness or weakness in your legs or arms isn’t something to brush off. These symptoms often indicate nerve issues that require prompt evaluation by a specialist to prevent permanent damage.
3. Conservative Treatments Have Limits
While physical therapy and medication can help, they might not be enough for severe cases. Recognizing when to escalate your care to a spine surgeon can make all the difference in recovery and long-term health.
4. The Power of Advanced Imaging
Modern MRI scans reveal details that physical exams can’t, guiding precise treatment. Investing in proper diagnostics early can save you time and frustration down the road.
5. Surgery Isn’t Always the Last Resort
Deciding on surgery can be intimidating, but in some cases, it’s the best way to restore function. Knowing when conservative care has been exhausted helps you make informed choices about your health.
Resources I’ve Come to Trust Over Time
- American Academy of Orthopaedic Surgeons: Their guidelines and research have helped me understand the importance of early diagnosis and appropriate treatment options, making it a go-to resource for reliable information.
- National Institute of Neurological Disorders and Stroke: This source provides comprehensive insights into nerve-related back issues, aiding in understanding symptoms that need urgent attention.
- PubMed and Medical Journals: Peer-reviewed studies offer the latest evidence-based practices, keeping me updated on advancements in spine care.
Parting Thoughts from My Perspective
Reflecting on my journey, I realize that recognizing the signs of needing an orthopedic spine surgeon can prevent long-term disability and improve quality of life. Back pain isn’t something to ignore—early intervention often leads to better outcomes. If you’re experiencing persistent symptoms, don’t hesitate to consult a qualified specialist. Your spine’s health is worth it, and taking that first step can be life-changing. If this resonated with you, I’d love to hear your thoughts or experiences. Feel free to share in the comments or reach out through our contact page. Remember, taking action today can make all the difference tomorrow.

